Lymphangioleiomyomatosis (LAM) is a rare multisystem disorder, predominantly affecting females in the reproductive age group, characterised by multiple cysts in lungs. A 15-year-old male was admitted in our institute for right sided renal mass for which he underwent right nephrectomy and was referred to our department for bilateral spontaneous pneumothoraces. CT thorax was done which showed bilateral pneumothoraces with multiple thin walled cysts and subtle ground glass opacities in both lung fields suggestive of changes of LAM. LAM is rarely seen in males, however if present ER/PR status can help in modifying the management. This is the youngest case of LAM reported in a male worldwide.
Lungs, Nephrectomy, Pneumothorax
Case Report
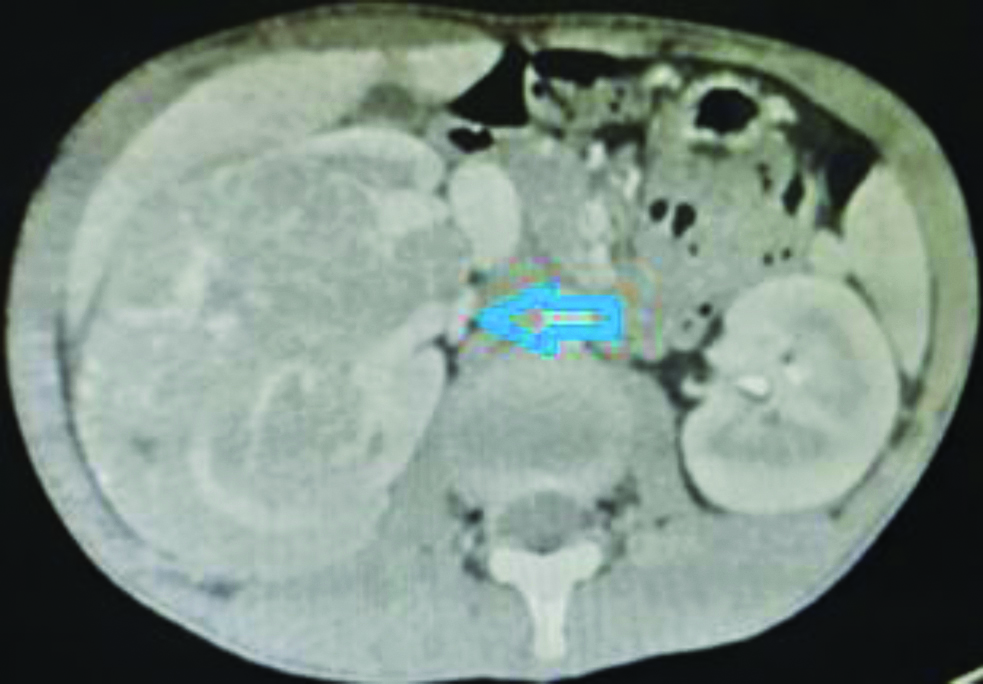
A 15-year-old male was admitted to the Department of Pulmonary Medicine for exertional dyspnea. He denied any history of fever, chills, chest pain or seizure episode. The patient denied any addiction. There was no history of similar complains in the family. He had a history of right nephrectomy done in the Department of Urology in the same institute in view of the right renal solitary mass of around 10 cm, 1 month ago [Table/Fig-1].
On examination, he was afebrile with RR 24/min, HR 125/min, and oxygen saturation 84% at room air. His external genitalia were normal with normal sexual hair distribution and body fat distribution with no gynaecomastia. He had typical facial angiofibromas [Table/Fig-2].

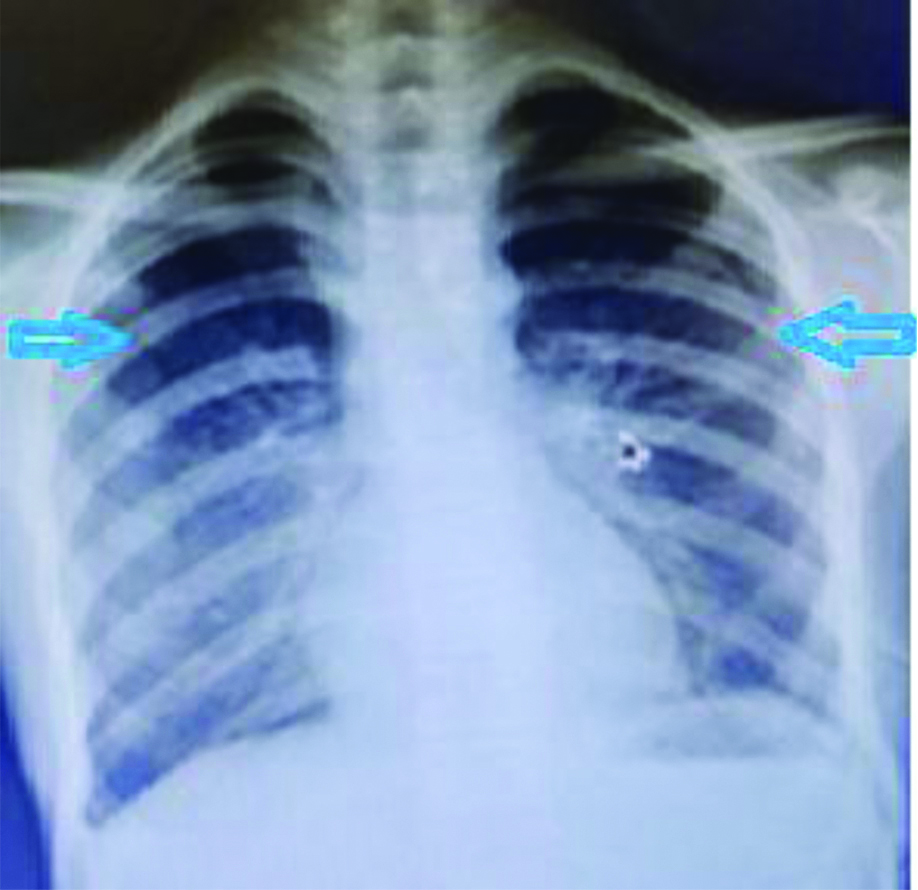
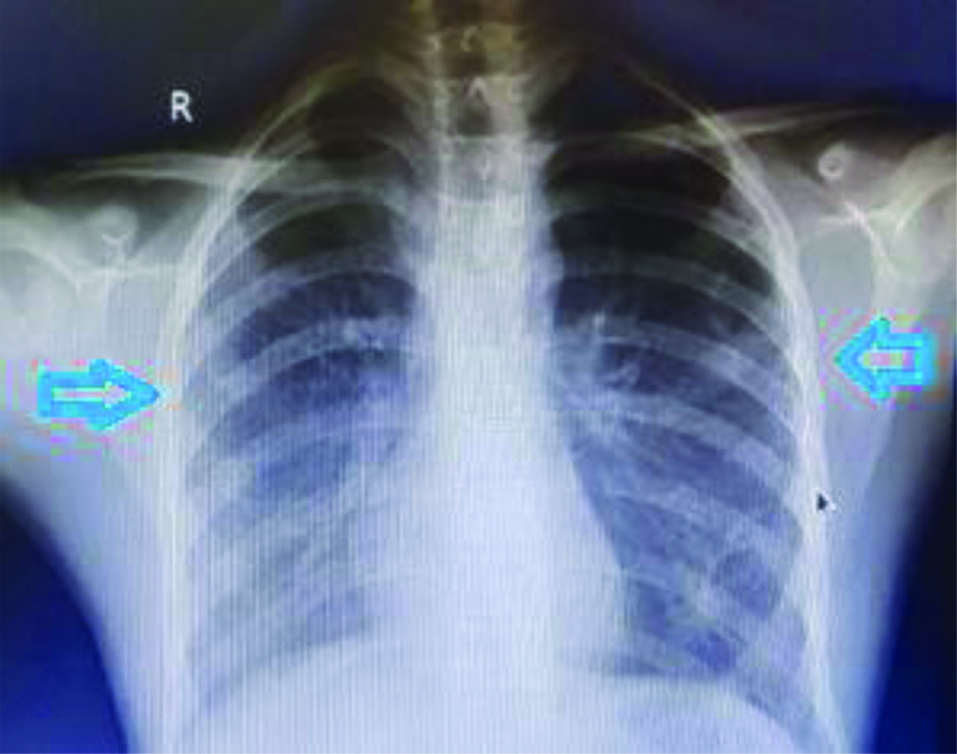
Chest X-ray PA view was done which was suggestive of bilateral pneumothoraces [Table/Fig-3].
Chest X-ray with bilateral pneumothoraces.
All other biochemical tests like Complete Blood Count, Liver Function Test, Renal Function Test, Random Blood Sugar, Urine routine were within normal limits.
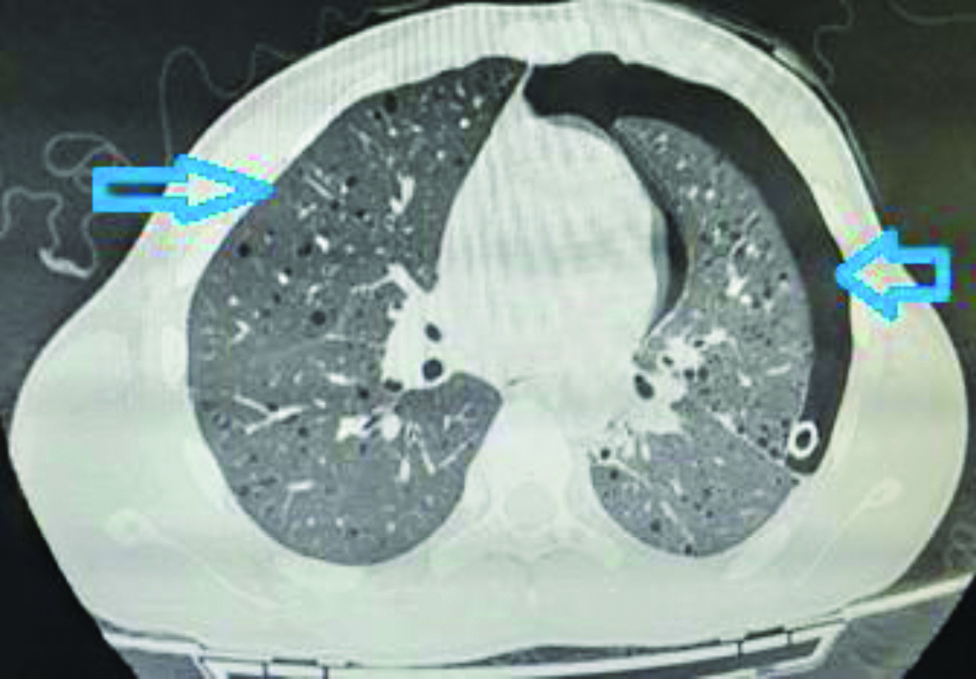
Intercoastal drainage tube was inserted bilaterally to relieve symptoms. Computed Tomography thorax was done after the patient became stable which showed left pneumothoraces with a left intercoastal drain in-situ with multiple thin-walled cysts and subtle ground glass opacities in both lung fields suggestive of cystic Interstitial Lung Disease most likely Lymphangioleiomyomatosis (LAM) [Table/Fig-4].
Left pneumothoraces with intercoastal drain in situ with bilateral thin walled cysts with ground glass opacities.
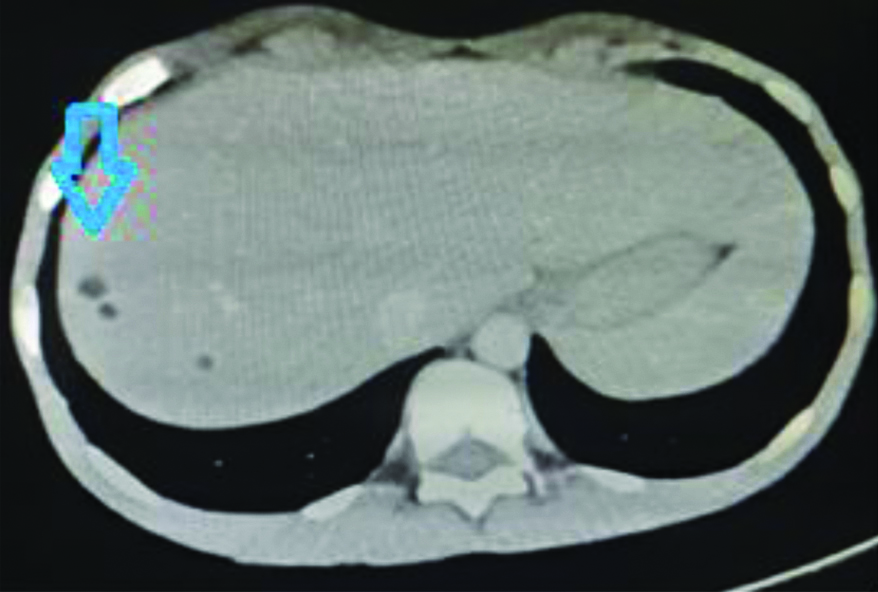
Contrast Enhanced Computed Tomography (CECT) Abdomen showed multiple well-defined hypodense lesions showing macroscopic fat within both lobes of liver suggestive of angiomyolipoma [Table/Fig-5].
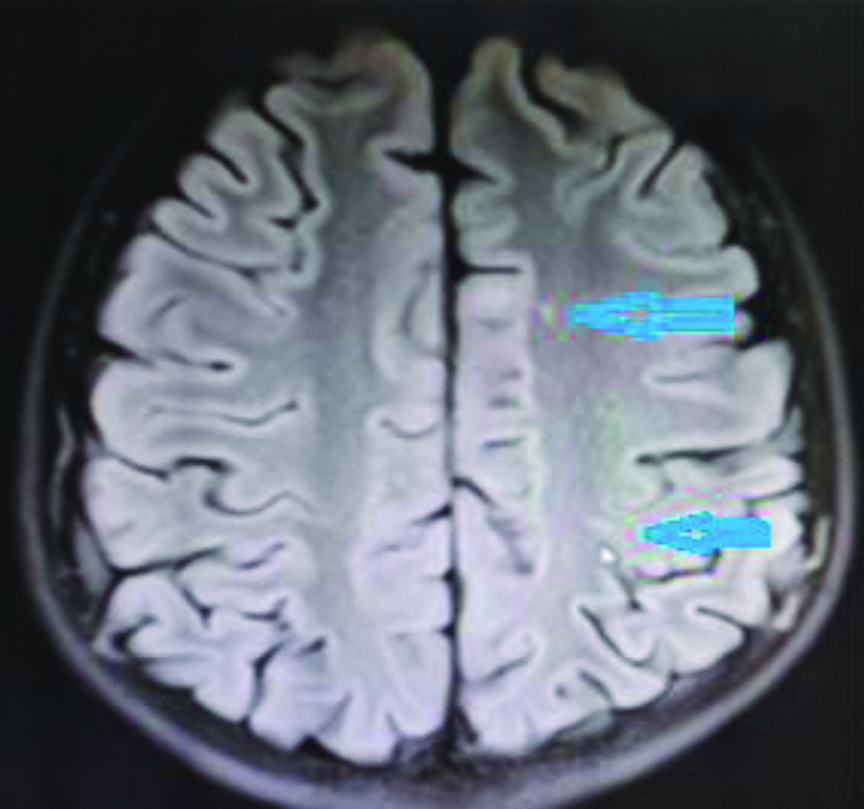
MRI brain was done which showed variably calcified subependymal nodules, radial white matter bands and few cortical tubers [Table/Fig-6]. All these findings confirmed the diagnosis of Tuberous Sclerosis.
MRI with sub-ependymal calcification.
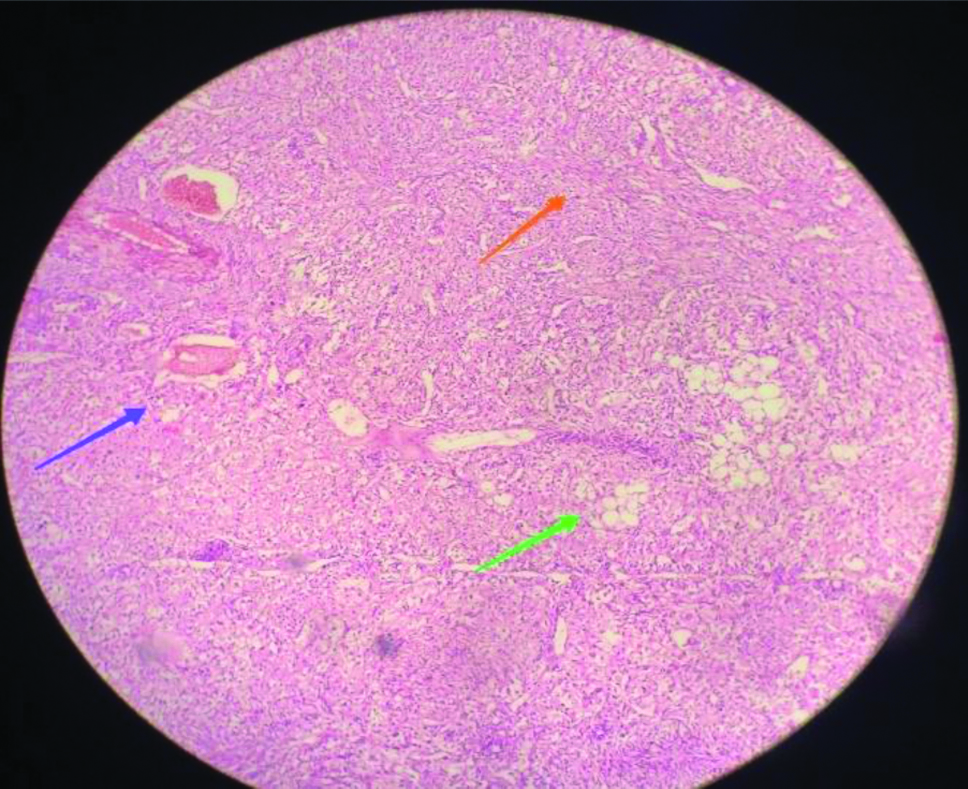
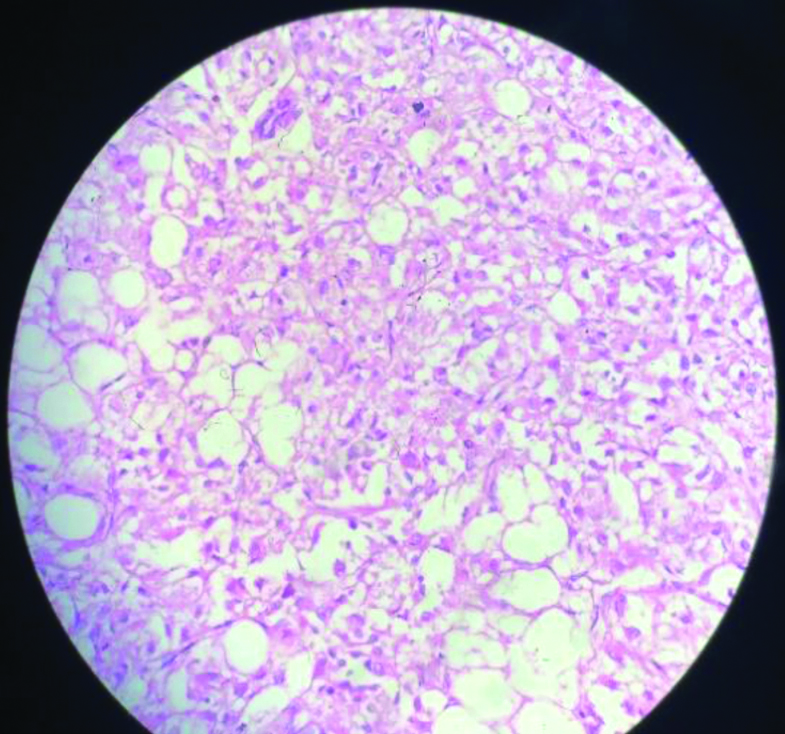
Histopathology of renal mass showed a tumour composed of spindle cells in a fascicular arrangement with scant adipose tissue and prominent muscular blood vessels [Table/Fig-7]. No significant nuclear atypia was appreciated. Mitotic activity was not apparent. Polygonal cells with dense eosinophilic cytoplasm, large hyperchromatic bizarre nuclei and multilobate nucleoli were also noted. No renal parenchyma was identified. On magnification lipoma was easily appreciated [Table/Fig-8].
Histopathology of renal mass showing Angiomyolipoma (H&E, 100x magnification).
Blue is angio component; Green is lipoma; Orange is spindle shaped cells
Lipoma component on magnification (H&E, 400x magnification).
On immunohistochemistry, tumour cells were positive for SMA and HMB-45, and negative for AE1/AE3, PAX8, and TFE3. Oestrogen and progesterone receptor proteins were also performed on the specimen which came out to be weakly positive.
A diagnosis of Tuberous Sclerosis Complex (TSC) with LAM was made based on clinical, radiological and histopathology with immunohistochemistry examination.
The patient underwent bilateral intercostal drainage insertion following which he had persistent air-leak which settled almost five days later and tube pleurodesis was done with 500 mg of doxycycline on the right side followed by the same on the left side after seven days and intercostal drain was removed thereafter. The complete expansion of the bilateral lung was seen on a chest radiograph [Table/Fig-9].
Post Pleurodesis complete lung expansion.
Pulmonary Function Test was done, once the patient was stable and was suggestive of restriction with small airway obstruction and poor bronchodilator reversibility with FVC-1.92 liter, Sirolimus (2 mg/day) was started along with bronchodilators. However, patient developed thrombocytopenia (platelets 30000) and acute kidney injury (creatinine raised to 3.2). Therefore, sirolimus was withheld and patient was started with Tamoxifen 10 mg BD as tumour was weakly positive for ER/PR (oestrogen and progesterone) receptors. Patient responded to treatment and is doing well since last 10 months. On regular follow-up stable chest X-ray and FVC of 1.90 and 1.89 liter when Pulmonary Function Test was performed after 5th and 10th month, respectively.
Discussion
LAM is a rare multisystem disorder, predominantly affecting females in the reproductive age group. It occurs due to the abnormal proliferation of smooth muscle-like cells leading to the formation of a thin-walled cyst in the lungs. It is almost always accompanied by angiomyolipomas, mostly in the kidney and liver [1-3]. Thirty percent of females with LAM also suffer from tuberous sclerosis, which is an autosomal dominant syndrome characterised by cerebral calcifications, seizures, cognitive dysfunction and hamartoma formation in various organ systems [4,5]. Rarely, LAM has also been reported in males [6].
However, present case was a 15-year-old male with features suggestive of tuberous sclerosis (angiomyolipoma of kidney and liver, adenoma sebaceum, calcified subependymal nodules, cortical tubers) with LAM.
TSC is a genetic disorder with autosomal dominant inheritance with an incidence of 1:5800 [7]. TSC affects almost every organ, with LAM as a pulmonary manifestation of TSC [8,9]. Genes responsible for LAM are TSC1 and TSC2 [1-3].
This patient is probably the youngest male (15 years) diagnosed as a case of LAM, reported worldwide. A 17-year-old male with LAM was reported from Kagoshima University, Japan in 2015 [10].
Another male patient of LAM was reported from Pennsylvania who was 39-year-old at presentation. He was presented with seizures and was a known case of schizophrenia with mild mental retardation [11]. TSC also manifests with neuropsychiatric illness like seizures, mental retardation, autism [12]. It is believed that the early onset of seizures may lead to mental retardation [13,14]. However this patient was neither mentally challenged nor he gave any history of seizure episodes.
Verma SK and SK Verma, published a case report of 28-year-old female who was diagnosed to have pulmonary LAM on basis of high resolution computed tomography findings and raised serum Vascular Endothelial Growth Factor (VEGF) [15]. She was on oral tamoxifen 10 mg BD. Clinical improvement without radiological deterioration was noticed after six months. There is no specific treatment in lymphangioleiomayomatosis but oophorectomy, progesterone, tamoxifen (20 mg/day) and Luteinizing Hormone Releasing Hormone (LHRH) analogue are being given with some antecedal support [16]. As the index patient could not tolerate sirolimus we decided to put him on tamoxifen after confirming ER/PR (estrogen/progesterone) receptor status.
Mahishale V et al., published a case report of a 34-year-old female, who presented with progressive breathlessness with bilateral basal crepitations and was diagnosed as LAM on basis of high-resolution computed tomography findings [17]. She was started on progesterone and domiciliary oxygen therapy and patient showed significant improvement.
Conclusion(s)
LAM is a cystic lung disease which mostly occurs in females, it can present with tuberous sclerosis or can also be found in isolation. It is rare in males. This young male presented with bilateral pneumothoraces, adenoma sebaceum, angiomyolipoma of liver and kidney which was positive for ER and PR receptors. Apart from sirolimus, tamoxifen can be given in patients of LAM, if ER/PR status is known. This is probably the first and the youngest case of LAM in male which is reported from India.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 08, 2019
Manual Googling: Dec 05, 2019
iThenticate Software: Dec 23, 2019 (9%)
[1]. Kitaichi M, Nishimura K, Itoh H, Izumi T, Pulmonary lymphangiomyomatosis: A report of 46 patients including a clinicopathologic study of prognostic factorsAm J Respir Crit Care Med 1995 151:527-33.10.1164/ajrccm.151.2.78422167842216 [Google Scholar] [CrossRef] [PubMed]
[2]. Urban T, Lazor R, Lacronique J, Murris M, Labrune S, Valeyre D, Pulmonary lymphangioleiomyomatosis: A study of 69 patients. Groupe d’Etudes et de Recherche sur les Maladies “Orphelines” Pulmonaires (GERM“O”P)Medicine (Baltimore) 1999 78:321-37.10.1097/00005792-199909000-00004 [Google Scholar] [CrossRef]
[3]. Chu SC, Horiba K, Usuki J, Avila NA, Chen CC, Travis WD, Comprehensive evaluation of 35 patients with lymphangioleiomyomatosisChest 1999 115:1041-52.10.1378/chest.115.4.104110208206 [Google Scholar] [CrossRef] [PubMed]
[4]. Costello LC, Hartman TE, Ryu JH, High frequency of pulmonary lymphangioleiomyomatosis in women with tuberous sclerosis complexMayo Clin Proc 2000 75:591-94.10.4065/75.6.59110852420 [Google Scholar] [CrossRef] [PubMed]
[5]. Franz DN, Brody A, Meyer C, Leonard J, Chuck G, Dabora S, Mutational and radiographic analysis of pulmonary disease consistent with lymphangioleiomyomatosis and micronodular pneumocyte hyperplasia in women with tuberous sclerosisAm J Respir Crit Care Med 2001 164:661-68.10.1164/ajrccm.164.4.201102511520734 [Google Scholar] [CrossRef] [PubMed]
[6]. Liu Y, Guo Z, Zhao C, Li X, Liu H, Chen J, Lymphangioleiomyomatosis: A case report and review of diagnosis and treatmentOnco Targets Ther 2018 11:5339-47.Published online 2018 Aug 3110.2147/OTT.S16136030214240 [Google Scholar] [CrossRef] [PubMed]
[7]. Taveira-DaSilva AM, Steagall WK, Moss J, LymphangioleiomyomatosisCancer Control 2006 13:276-85.10.1177/10732748060130040517075565 [Google Scholar] [CrossRef] [PubMed]
[8]. Aubry MC, Myers JL, Ryu JH, Henske EP, Logginidou H, Jalal SM, Pulmonary lymphangioleiomyomatosis in a manAm J Respir Crit Care Med 2000 162:749-52.10.1164/ajrccm.162.2.991100610934115 [Google Scholar] [CrossRef] [PubMed]
[9]. Schiavina M, Di Scioscio V, Contini P, Cavazza A, Fabiani A, Barberis M, Pulmonary lymphangioleiomyomatosis in a karyotypically normal man without tuberous sclerosis complexAm J Respir Crit Care Med 2007 176:96-98.10.1164/rccm.200610-1408CR17431222 [Google Scholar] [CrossRef] [PubMed]
[10]. Kazuhiro W, Lymphangioleiomyomatosis in a maleThe Annals of Thoracic Surgery 2015 100(3):1105-07.10.1016/j.athoracsur.2014.11.06926354644 [Google Scholar] [CrossRef] [PubMed]
[11]. Aubry M-C, Myers JL, Ryu JH, Henske EP, Logginidou H, Tazelaaraug HD, Pulmonary lymphangioleiomyomatosis in a manAmerican Journal of Respiratory and Critical Care Medicine 2000 162(2 Pt 1):749-52.10.1164/ajrccm.162.2.991100610934115 [Google Scholar] [CrossRef] [PubMed]
[12]. Sedky K, Hughes T, Yusufzie K, Lippmann S, Tuberous sclerosis with psychosisPsychosom 2003 44:521-22.10.1176/appi.psy.44.6.521-a14597689 [Google Scholar] [CrossRef] [PubMed]
[13]. Hunt A, Dennis J, Psychiatric disorder in children with tuberous sclerosisDev Med Child Neurol 1987 29:190-98.10.1111/j.1469-8749.1987.tb02135.x3582788 [Google Scholar] [CrossRef] [PubMed]
[14]. Pampiglione G, Pugh E, Infantile spasms and subsequent appearance of tuberous sclerosis syndromeLancet 1975 2:104610.1016/S0140-6736(75)90343-8 [Google Scholar] [CrossRef]
[15]. Verma SK, Verma SK, Pulmonary lymphangioleiomyomatosis (PLAM)Lung India 2007 24:150-52.10.4103/0970-2113.44382 [Google Scholar] [CrossRef]
[16]. Rossi GA, Balbi B, Oddera S, Response to treatment with an analogue of luteinizing-hormone-releasing hormone in patients with pulmonary lymphangioleiomyomatosisAm Rev Respir Dis 1991 141:174-76.10.1164/ajrccm/143.1.1741824744 [Google Scholar] [CrossRef] [PubMed]
[17]. Mahishale V, Patil B, Ramannavar A, Suresh G, Rathi A, Sindhuri A, Lymphangioleiomyomatosis: A rare case reportJ NTR Univ Health Sci 2014 3:189-91.10.4103/2277-8632.140944 [Google Scholar] [CrossRef]