Management of renal calculi is dependent on various factors such as size, composition and location of stones, existence of obstruction and anatomical variations of the urinary system. There are different therapeutic approaches available with continuously advancing techniques and surgical treatments. Earlier, the commonly used treatment options used for removal of stones include Extracorporeal Shock Wave Lithotripsy (ESWL), PCNL, and Retrograde Intrarenal Surgery (RIRS) [1]. According to European Association of Urology (EAU), PCNL is a standard treatment for stone larger than 2 cm or as a second option, RIRS can also be used [2]. Other modified minimally invasive techniques include mini-, micro-, and ultra-Percutaneous nephrolithotomy (Perc) which are used for removal of stone less than 1.5 cm [3].
A meta-analysis comparing these minimally invasive techniques with RIRS showed higher stone free rate with minimally invasive techniques as compared to RIRS. However, RIRS was associated with shorter hospitalisation and low reduction in haemoglobin levels [4]. Although, PCNL showed higher rate of stone clearance, it increases the risk of morbidity due to higher complication rates. The complications associated with PCNL technique include bleeding, the lesion of the collecting system, the risk of urinary infection and bacteraemia [5,6].
Jackman SV et al., first established the mini-Perc technique with 11F sheath and showed 85% stone free rate and minimal morbidity in patients with 2-6 years of age [7]. A recent systematic review showed promising results of lower blood loss and similar stone free rate with the use of mini-Perc having tract size less than or equal to 22 Fr as compared to standard PCNL procedure [6]. However, the duration of procedure was longer in patients treated with mini-Perc compared to standard PCNL technique.
Previous non-randomised study by Mishra S et al., demonstrated that the stone free rate and complications were similar between mini-Perc and standard PCNL in patients with 1-2 cm renal calculi size. It also showed reduced bleeding and hospital stay with mini-Perc as compared to standard PCNL treatment [8]. The aim of the present study was to evaluate and compare the intraoperative and postoperative outcomes of standard PCNL and mini-Perc treatments in patients with renal calculi ≤2 cm in size.
Materials and Methods
A Prospective Observational study was conducted at the Department of Urology, Bharati Vidyapeeth Medical College and Hospital, Pune, Maharashtra, India from February 2017 to January 2019.
Patients above 18 years with calculi size ≤2 cm in the kidney were included in the study. The exclusion criteria were patients with urosepsis, uncorrected coagulopathy and stones >2 cm in size. The patients were randomly (1:1, generated using online randomisation tool using block randomisation, size 4) allocated to standard PCNL treatment and mini-Perc treatment. The study was approved by the Institutional Ethics Committee (BVDU/Exam/972/2019-20). Written informed consent was obtained from each participant before enrolment.
Preoperatively, prophylactic antibiotic cefuroxime 1.5 gm was given intravenously, if urine culture showed evidence of infection. Each patient received 3 doses of injectable 1 gm paracetamol as a standard of care. Any extra dose (>3) was called as additional dose requirement. Total dose needed beyond standard of care was calculated for each group (grams). Intraoperative percutaneous nephrostomy fluid culture or stone cultures was sent whenever necessary.
Detailed history and physical examination were performed. Laboratory investigations were carried if required including haemogram, renal function test, blood sugar level, coagulation profiles and urinalysis with urine culture and sensitivity. Patients demographics, stone characteristics (size, number, and location), pre and postoperative haematology and biochemistry evaluations were recorded. Radiological evaluation was performed in the form of plain X-ray of Kidney, Ureter and Bladder (KUB) and ultrasound of the abdomen. All patients underwent an Intravenous Urography (IVU) or Computed Tomography (CT) urography prior to the procedure to assess the collecting system.
Cumulative stone burden was defined as the two-dimensional area determined by the length and width of the stone on preoperative plain X-ray KUB/CT KUB. In case of multiple stones, it was calculated by the sum of the area of each calculus (cm2). Clearance was defined as no stone visible on X-ray KUB and all fragments less than 4 mm were considered as clinically insignificant residual fragments. The study outcomes were operative time, postoperative analgesic requirement, stone clearance (at one month follow-up), tube or tubeless procedure, time for removal of the nephrostomy tube and Double J stent. Any intraoperative or postoperative complications were also recorded. Transfusions if needed were documented.
Statistical Analysis
A consecutive type of non-probability sampling was followed for selection of study subjects. Statistical analysis was performed using SPSS version 21.0. Qualitative data was represented in the form of frequency and percentage. Association between qualitative variables was evaluated using Chi-square test and Fisher-exact test. Quantitative data was represented using mean (Standard Deviation {SD}), median and Interquartile Range (IQR). Comparison of quantitative data between the two groups was performed using unpaired t-test, if data passed normality test and by Mann-Whitney U test, if data failed normality test. A p-value of <0.05 was considered as statistically significant.
Results
A total of 100 consecutive patients with renal stones were randomly selected for treatment with standard PCNL (n=50) or mini-Perc (n=50). The percentage of males in both standard PCNL (68%) and mini-Perc (64%) were greater than females (32% and 36%, respectively). The mean (SD) age (years) of patients from standard PCNL and mini-Perc groups were 40.78 (13.06) and 39.79 (12.98), respectively. In patients treated with standard PCNL technique, 31 patients (62%) had stone located on the left kidney and remaining 19 (38%) had stone on right side of the kidney. Whereas, in patients treated with mini-Perc technique, 29 (58%) had left kidney stone and 21 (42%) had right kidney stone. The mean stone burden (cm2) was comparatively higher in patients treated with standard PCNL (1.68) than with mini-Perc (1.62). However, the difference was not statistically significant (p=0.79). The mean number of calculi was comparable between both the groups (standard PCNL, 1.23 and mini-Perc, 1.37; p=0.07) [Table/Fig-1].
Demographics and baseline characteristics of patients with ureteric stones.
| Parameters | Standard PCNL (n=50) | mini-Perc (n=50) | p-value |
|---|
| Age, years, mean (SD) | 40.78 (13.06) | 39.79 (12.98) | 0.73 |
| Gender |
| Male | 34 (68) | 32 (64) | 1.0 |
| Female | 16 (32) | 18 (36) |
| Stone side |
| Left kidney | 31 (62) | 29 (58) | 0.83 |
| Right kidney | 19 (38) | 21 (42) |
| Stone burden, cm2, mean (SD) | 1.68 (0.27) | 1.62 (0.26) | 0.79 |
| Number of calculi, mean (SD) | 1.23 (0.42) | 1.37 (0.56) | 0.07 |
| Stone position |
| Upper calyx | 5 (10) | 4 (8) | 0.53 |
| Middle calyx | 2 (4) | 6 (12) |
| Lower calyx | 17 (34) | 18 (36) |
| Pelvis | 22 (44) | 17 (34) |
| Lower calyx and pelvis | 1 (2) | 2 (4) |
| Middle calyx and pelvis | 3 (6) | 1 (2) |
| Hydronephrosis |
| Nil | 7 (14) | 8 (16) | 0.75 |
| I | 14 (28) | 16 (32) |
| II | 21 (42) | 16 (32) |
| III | 7 (14) | 8 (16) |
| IV | 1 (2) | 0 (0) |
| Puncture location |
| Lower calyx | 40 (80) | 38 (76) | 0.23 |
| Middle calyx | 5 (10) | 10 (20) |
| Upper calyx | 5 (10) | 2 (4) |
Data shown as n (%), unless otherwise specified. PCNL, percutaneous nephrolithotomy; mini-Perc, miniaturised percutaneous nephrolithotomy
In standard PCNL group, most of the patients had stone located in pelvis (n=22, 44%). However, majority of patients in mini-Perc group had stone in lower calyx (n=18, 36%). A total of 70% of patients treated with standard PCNL and 64% of patients treated with mini-Perc had grade I and II hydronephrosis. The commonly punctured location was lower calyx in both groups (standard PCNL, n=40, 80% and mini Perc, n=38, 76%) [Table/Fig-1].
Outcomes of patients treated with standard PCNL and mini-Perc are reported in [Table/Fig-2]. The mean tract size (Fr) was significantly different between patients treated with standard PCNL (26.98) and with mini-Perc (15.61) (p<0.01). The rate of complete stone clearance was similar between patients treated with standard PCNL and with mini-Perc (94% versus 92%, p=1.0). Two patients in standard PCNL group and four patients in mini-Perc group underwent ESWL auxiliary procedure. However, one patient from standard PCNL group had II stage PCNL as an accessory procedure for complete stone removal. The mean operating time (minutes) was significantly lower in patients treated with standard PCNL as compared to patients treated with mini-Perc (73.72 versus 78.86; p<0.05). However, irrigation fluid required (L) for mini-Perc group was significantly reduced than standard PCNL group (7.24 versus 10.15; p<0.01).
Outcome of patients in standard PCNL and mini-perc withrenal calculi.
| Outcomes | Standard PCNL (n=50) | mini-Perc (n=50) | p-value |
|---|
| Tract size, Fr, mean (SD) | 26.98 (2.48) | 15.61 (0.74) | <0.01 |
| Clearance |
| Complete | 47 (94) | 46 (92) | 1.0 |
| Partial | 3 (6) | 4 (8) |
| Auxillary procedure done |
| ESWL | 2 (4) | 4 (8) | 0.43 |
| II stage PCNL | 1 (2) | 0 |
| Operating time (min), mean (SD) | 73.72 (10.10) | 78.86 (12.58) | <0.05 |
| Irrigation fluid required (L), Mean (SD) | 10.15 (1.99) | 7.24 (1.19) | <0.01 |
| Placement of PCN tube |
| Standard | 47 (94) | 40 (80) | <0.05 |
| Tubeless | 3 (6) | 10 (20) |
| Energy source |
| Pneumatic lithotripsy | 49 (98) | 6 (12) | <0.01 |
| Laser lithotripsy | 1 (2) | 44 (88) |
| Placement of stent |
| Double J stent | 44 (88) | 46 (92) | 0.74 |
| No stent | 6 (12) | 4 (8) |
| Complications |
| Pelvic perforation | 2 (4) | 2 (4) | 1.00 |
| Bleeding | 4 (8) | 0 (0) | <0.05 |
| Fever | 5 (10) | 4 (8) | 1.00 |
| Days of hospitalisation, mean (SD) | 4.12 (0.77) | 3.16 (0.83) | <0.01 |
| Drop in Haemoglobin (gm%) | 1.49 (0.49) | 0.72 (0.27) | <0.01 |
| Drop in PCV (%) | 5.07 (1.95) | 2.47 (1.03) | <0.01 |
Data shown as n (%), unless otherwise specified. ESWL, extracorporeal shock wave lithotripsy; PCN: Percutaneous nephrostomy; PCNL: Percutaneous nephrolithotomy; PCV: Packed cell volume; mini-Perc: Miniaturised percutaneous nephrolithotomy
Intraoperatively, majority of the patients in both the groups had placement of standard PCN tube and double J stent (Standard PCNL, 94% and 88%; mini-Perc, 80% and 92%, respectively). However, decision of a tubeless PCNL was significantly more in the mini-Perc group than standard PCNL group (20% versus 6%, p<0.05). The overall rate of complications was comparatively higher in patients with standard PCNL (22%) as compared to patients with mini-Perc treatment (12%).
The mean hospital stay (days) was significantly higher in patients treated with standard PCNL compared to patients treated with mini-Perc (4.12 versus 3.16; p<0.01). The mean drop in haemoglobin (gm%) as well as drop in PCV (%) were significantly decreased in mini-Perc group than in standard PCNL group (0.72 versus 1.49 and 5.07 versus 2.47; p<0.01). Pneumatic lithotripsy was commonly used in standard PCNL (n=49, 98%) while, laser lithotripsy was commonly used in mini-Perc group (n=44, 88%) (p<0.001).
Preoperative urine culture was performed in all the patients undergoing the procedure. Out of 100 patients, 25 patients had positive urine cultures and 75 patients had negative urine cultures [Table/Fig-3].
Organism isolated in preoperative urine culture and postoperative urine culture.
| Organism isolated | Preoperative (n=100) | Postoperative (n=12) |
|---|
| No growth | 75 (75) | - |
| Escherichia coli | 9 (9) | 8 (66.67) |
| Escherichia coli (ESBL) | 5 (5) | 1 (8.3) |
| Enterococcus faecalis | 2 (2) | 1 (8.3) |
| Pseudomonas aeruginosa | 3 (3) | 2 (16.67) |
| Klebsiella pneumonia | 5 (5) | 0 (0) |
| Proteus mirabilis | 1 (1) | 0 (0) |
Data shown as n (%). ESBL, extended-spectrum beta-lactamase
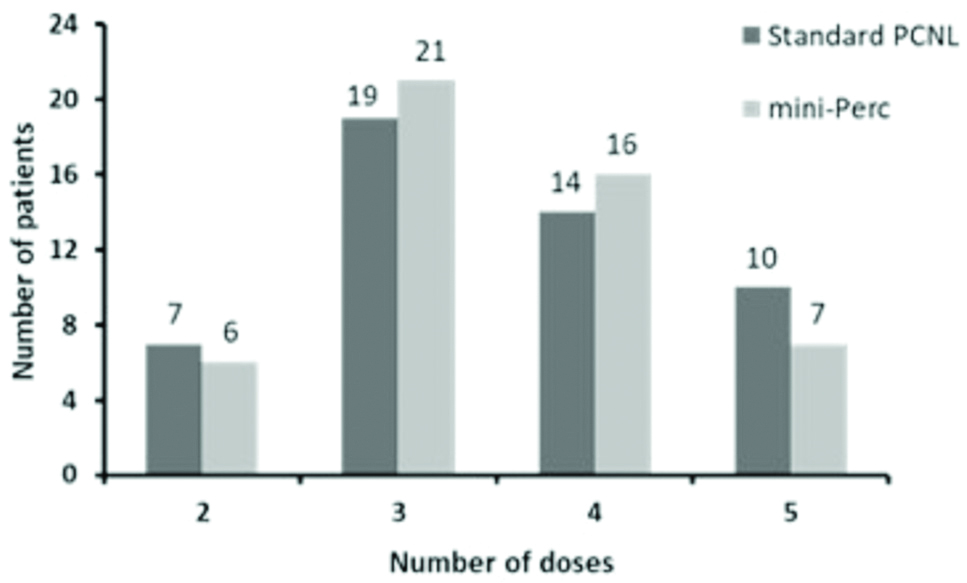
No significant (p>0.05) difference was observed between postoperative analgesic requirement in standard PCNL and mini-Perc groups [Table/Fig-4].
Requirement of postoperative analgesia.
mini-Perc: Miniaturised Percutaneous nephrolithotomy; PCNL: Percutaneous nephrolithotomy.
Discussion
The present study prospectively compared the intraoperative and postoperative outcomes of standard PCNL and mini-Perc treatments in patients with renal calculi ≤2 cm in size. This study revealed that patients with mini-Perc treatment were associated with decreased tract size indicating reduced invasiveness, reduced chances of fluid overload and associated complications with no signs of bleeding, a significantly shorter duration of hospital stay suggesting rapid recovery of patients and similar stone clearance rate indicating similar efficacy and better safety profile than standard PCNL group.
In the present study, the mean tract size (Fr) was significantly decreased in patients treated with mini-Perc (15.61) as compared to standard PCNL (26.98) (p<0.01). Mini-Perc requires lesser tract dilatation which reduces renal vasculature damage and infundibular calyceal tear. In a similar study by Mishra S et al., reported the significantly reduced mean tract size of 18.2 Fr in the mini-Perc than that of standard PCNL (26.8 Fr) (p<0.0001) [8]. These results are in concordance with the present study.
The success of the mini-Perc technique depends mainly on stone fragmentation and its removal by saline irrigation. Hence, the energy source used for stone fragmentation is an important aspect in mini-Perc. For intracorporeal lithotripsy, two types of energy sources were used in the present study. Pneumatic lithotripsy was commonly used in standard PCNL (98%) while, laser lithotripsy was commonly used in mini-Perc group (88%). Pneumatic lithotripsy was also successfully used in 12% of patients from mini-Perc group. A recent prospective randomised controlled trial comparing laser lithotripsy with pneumatic lithotripsy in mini-Perc for renal calculi concluded that laser lithotripsy is associated with lower stone migration and easier retrieval of the smaller fragments it produces [9]. In a previous study of Mishra S et al., holmium laser and pneumatic lithotripter were the main energy sources used in mini-Perc and standard PCNL, respectively [8]. These observations accord with the present study observations and indicate beneficial effects of laser over pneumatic lithotripsy in mini-Perc procedure.
Achieving complete stone free status is one of the main goals to achieve in the treatment of renal calculi. In the present study, rate of complete stone clearance was almost similar between patients treated with standard PCNL (94%) and with mini-Perc (92%). A major drawback of standard PCNL procedure is a surgical procedure requiring general anaesthesia. A stone free rate of 94% achieved using this technique outweighs the major disadvantage of standard PCNL. Several studies using mini-Perc technique have reported stone free rates in the range of 60-90% [10-12]. Apparently, stone fragments are known to be present after laser lithotripsy and it is advisable to see if they are clinically significant at one-month follow-up. Therefore, present study assessed stone clearance at one month which showed similar stone clearance rates in both treatment groups. Only one patient had stone fragment of 6 mm and rest of the patients were completely stone free. These observations indicate that min-Perc is effective in achieving acceptable clearance rates as with standard PCNL. In line with the present study observations, Mishra S et al., also reported similar complete stone clearance rates in mini-Perc (96%) and standard PCNL (100%) groups [8].
The present study reported a significantly longer mean operating time (minutes) in patients treated with mini-Perc (78.86) than those treated with standard PCNL (73.72) (p<0.05). In standard PCNL, it is possible to remove large stone fragments because of larger PCNL tract size whereas, in mini-Perc, stone has to be fragmented in small sizes for easy removal by hydrodynamics of irrigation and small baskets or ureteroscopic forceps. The learning curve during initial procedures of mini-Perc might have also caused longer operative time. Observations reported in a study by Mishra S et al., corroborate with the present study observations [8]. They reported significantly longer operative time for min-Perc procedure (45.2 minutes) than standard PCNL (31 minutes) (p=0.0008). In other previous series of studies, the reported operating time for mini-Perc ranged from 99-156 minutes [13-15]. On the contrary, a recent study by Sabnis RB et al., comparing mini-Perc with RIRS, reported significantly shorter mean operating time in mini-Perc group (40.81 versus 50.63 minutes; p=0.003) [16].
If the cardio-respiratory or renal status is compromised, due to lack of fluid absorption, fluid overload may occur. It is also linked with both infective and non-infective pyrexia. In the present study, irrigation fluid required (L) for mini-Perc group was significantly reduced than standard PCNL group (7.24 versus 10.15; p<0.01). Reduced requirement of irrigation fluid may help to reduce fluid overload which ultimately will aid in prevention of further complications [17].
In the present study, bleeding was observed in standard PCNL group only, while pelvic perforation and postoperative fever were observed in patients of both groups. The overall rate of complications was comparatively higher in patients with standard PCNL than those with mini-Perc treatment suggesting that patient’s tolerability for mini-Perc treatment is better than standard PCNL treatment. The results of previous studies are in accordance with the present study [11,18-21]. The common complications observed in those studies were fever, bleeding, pelvic perforation, urine leakage, haematuria and urine infection. Results of a study of Mishra S et al., concur with the present study. They also reported bleeding only in standard PCNL group with pelvic perforation and fever in both, mini-Perc and standard PCNL, groups [8].
Another significant advantage of mini-Perc treatment, over other treatments, is a reduced duration of hospital stay. In the present study, mean hospital stay (days) was significantly reduced in patients treated with mini-Perc compared to patients treated with standard PCNL (p<0.01). The mean drop in haemoglobin (gm%) as well as drop in packed cell volume (%) were significantly decreased in mini-Perc group than in standard PCNL group (p<0.01). These observations are parallel to the studies done by Mishra S et al., and Giusti G et al., who reported significantly decreased hospital stay and mean haemoglobin drop in mini-Perc group than standard PCNL group. Drop in haemoglobin and packed cell volume indicates blood loss occurred during these procedures [8,13].
Present study reported that decision of a tubeless PCNL was significantly more in the mini-Perc group than standard PCNL group (p<0.05). More number of tubeless procedures may reduce requirement of analgesics in mini-Perc group in postoperative period. A previous study done by Desai MR et al., concluded that the tubeless PCNL was associated with the least postoperative pain, urinary leakage and hospital stay [22].
The primary objective of mini-Perc treatment is to reduce the pain occurred due to the procedure. Since introduction of mini-Perc, a number of studies have questioned the utility of this procedure in reduction of postoperative pain. In the present study, mean dose of analgesics in standard PCNL group (3.54) was comparatively more that mini-Perc group (3.08). This suggests that there was less requirement of analgesia in mini-Perc group than standard PCNL group which ultimately indicates reduced pain in mini-Perc procedure. This might be because of a greater number of tubeless procedures done in the mini-Perc group. Therefore, these observations add significant support to the hypothesis of association of postoperative pain with presence of nephrostomy.
Limitation(s)
This was a single center study. Hence, results needs be generalised with caution.
Conclusion(s)
Present study observations revealed that the mini-Perc treatment and standard PCNL have achieved similar stone clearance rates. However, mini-Perc is beneficial to patients with significantly reduced pain, smaller tract size, decreased hospital stay and no bleeding complications. Therefore, mini-Perc treatment is as effective as standard PCNL in stone clearance, with mini-Perc being better tolerated in patients with renal calculi ≤2 cm in size. The mini-Perc treatment can replace standard PCNL treatment for these patients.
Data shown as n (%), unless otherwise specified. PCNL, percutaneous nephrolithotomy; mini-Perc, miniaturised percutaneous nephrolithotomy
Data shown as n (%), unless otherwise specified. ESWL, extracorporeal shock wave lithotripsy; PCN: Percutaneous nephrostomy; PCNL: Percutaneous nephrolithotomy; PCV: Packed cell volume; mini-Perc: Miniaturised percutaneous nephrolithotomy
Data shown as n (%). ESBL, extended-spectrum beta-lactamase