It is a established fact that the incidence of SIL is increasing within teenage populations [1] and is most likely related to the increased rate of sexual activity and rising incidence of Human Papilloma Virus infection in adolescents [2-6]. The recommendation of National Cancer Institute is to cytologically screen the young girls at 18 years of age or at the onset of sexual activity. These girls are recommended to undergo Pap smear examination at yearly interval and when all the three reports are normal, the screening interval should be extended to three years [7]. In rural areas of India, it has been customary to perform the marriage of the girls at early age in the adolescent stage of 15-16 years. This practice puts these girls to sexual exposure at young age and they become prone to the onset of any cytopathological changes in the cervix. Hence, cytological study is mandatory in these girls to rule out any development of pre-malignancy and also any infection of sexually transmitted diseases. Since promiscuity is rare in the rural women, chances of HPV infection are minimal. The cytology services organised by the Government seldom reach to the rural women. Hence study like ours is itself a novelty and need of the hour.
Since young rural girls have increased prolonged sexual activity after marriage, we have compared the cytological findings in the three cohorts- adolescent girls between 16-20 years, young adult girls between 21-25 years and adult women between 26-30 years to find out relation between the increasing sexual exposure and incidence of cervical cytopathology and the entire data has been analysed in the context of different predisposing factors of cervical carcinogenesis.
Materials and Methods
This was a prospective cervical screening study conducted since May 2013 which was in progress in the villages of Kakori and Malihabad blocks of Lucknow through camp approach under the auspices of Era’s Lucknow Medical College and Hospital, Lucknow, Uttar Pradesh, India. Ethical clearance was obtained from the Ethical Committee of the Institution for starting the program (Institution Ethical clearance no. ELMC/R.Cell/Fac/I-52/2013). Till July 2019, a total of 174 camps were organised after counseling and motivation of women for undergoing Pap smear examination (Total duration of study- 6 years and 3 months). A total of 5,006 women have attended these camps and 2789 of these (55.7%) have undergone Pap test. As marriages are performed in the villages at early age below 20 years, the majority of these 2789 women in whom Pap smear has been taken were below 30 years of age (1185). Many of them were literate and had knowledge of the risk factors of carcinoma cervix and utility of early detection of the disease. Further most of these girls were nulliparous suffering from the primary infertility and came to attend the camp for treatment. They were referred to the Hospital for proper management.
To see the effect of prolonged sexual exposure on the cytological status of cervix, these 1185 women were divided into 3 cohorts based on their ages as defined above. These women could not tell exact year of their marriage but roughly told that they were married at an early age below 20 years. Hence the age when the smears were taken in them have been taken as age to include them in either of the 3 cohorts accordingly. Those women who have undergone hysterectomy or were pregnant or were more than 60 years of age were excluded from the study.
All the cervical smears were collected by the gynaecologist attending the camp and stained in the cytology lab of the Pathology department of the college according to the Papanicalaou’s technique. The cytopathological changes in the cervical smears were graded according to the Revised Bethesda System of classification of 2002 [8]. The STDs were diagnosed in the cytology smears on the basis of either their individual presence (Candida albicans and Trichomonas vaginalis) or cytopathological changes produced by them- koilocytosis (HPV) and ground grass appearance of nuclei and multinucleation (Herpes simplex virus).
The informed consent of the women was taken as thumb impression if illiterate or signature if educated.
Statistical Analysis
The entire data was statistically analysed applying Chi-square test. The software used was SPSS version 22.
Results
Of the total 2789 women who have undergone Pap smear examination at the camps, 97 were adolescents, 338 were young adult’s girls and 750 were adult women. The remaining 1604 women were above 30 years of age ranging from 31 to 60 years and these women were not included in the study. Cytological examination of cervical smears in these three cohorts revealed following pattern of changes:
a. Adolescents- Atypical Squamous Epithelial changes of unknown significance (ASCUS) - 9 (9.2%)
Low grade SIL (LSIL) - 16 (16.4 %)
Inflammation-10 (10.3%)
Normal-62 (63.9%)
b. Young adult girls- ASCUS - 20 (5.9%)
LSIL - 58 (17.1%)
Inflammation- 80 (23.6%)
Normal- 180 (53.2%)
c. Adult women- ASCUS -35(4.6%)
SIL-145 (19.3%); LSIL -140 (18.6%)
High grade SIL (HSIL) -5 (0.6%)
Inflammation- 118 (15.7%)
Normal- 452 (60.2%)
The SIL rate was calculated from the percentage of women showing SIL in total number of cases studied in a particular group.
Inflammatory smears were maximum in number in young adult girls (23.6%) than 10.3% seen in the adolescents. The incidence subsided to 15.7% in the adult women. ASCUS was common in all the three cohorts [Table/Fig-1] while majority of cases noticed were LSIL [Table/Fig-2]. The HSIL was seen in only five cases in the adult women group [Table/Fig-3]. As expected, ASCUS which precede SIL were found higher in adolescents (9.2%) and showed decline to 5.9% in the young adult girls and 4.6% in the adult women but this difference was found to be statistically insignificant (χ2=0.279: p=0.597). However, the SIL rate was found rising with the increasing sexual exposure from 16.4% in the adolescents to 17.1% in the young adult girls and 19.2% in the adult women. However, here also the difference in the SIL rate between three groups was found to be insignificant (χ2=3.438: p=0.064). Further, 5 of the 145 SIL cases (0.6%) noticed in the adult women were HSIL.
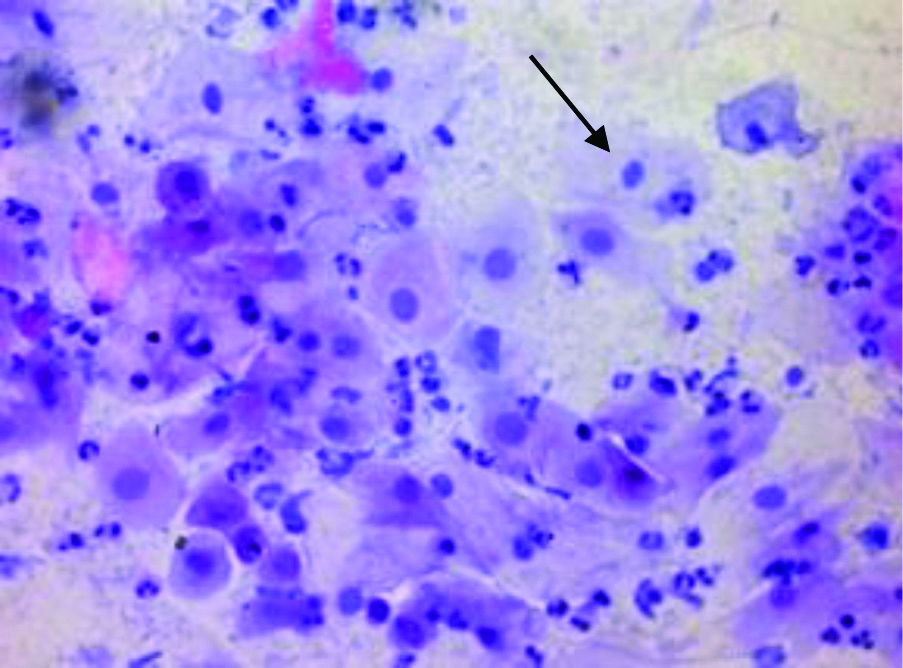
Atypical squamous epithelial changes of unknown significance (ASCUS).
Ectocervical smear showing atypical squamous intermediate cells with nuclear enlargement and mild hyperchromasia (Pap×400)
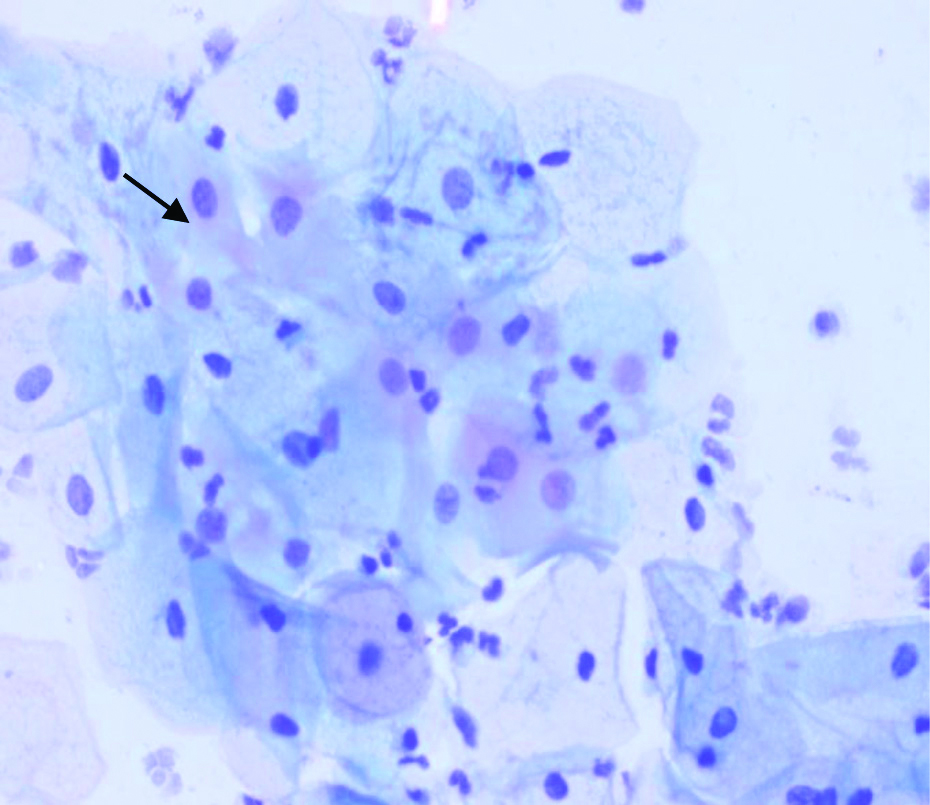
Low Grade Squamous Intraepithelial Lesion of ectocervix (LSIL).
Intermediate and parabasal cells showing nuclear enlargement and coarse chromatin (Papx400)
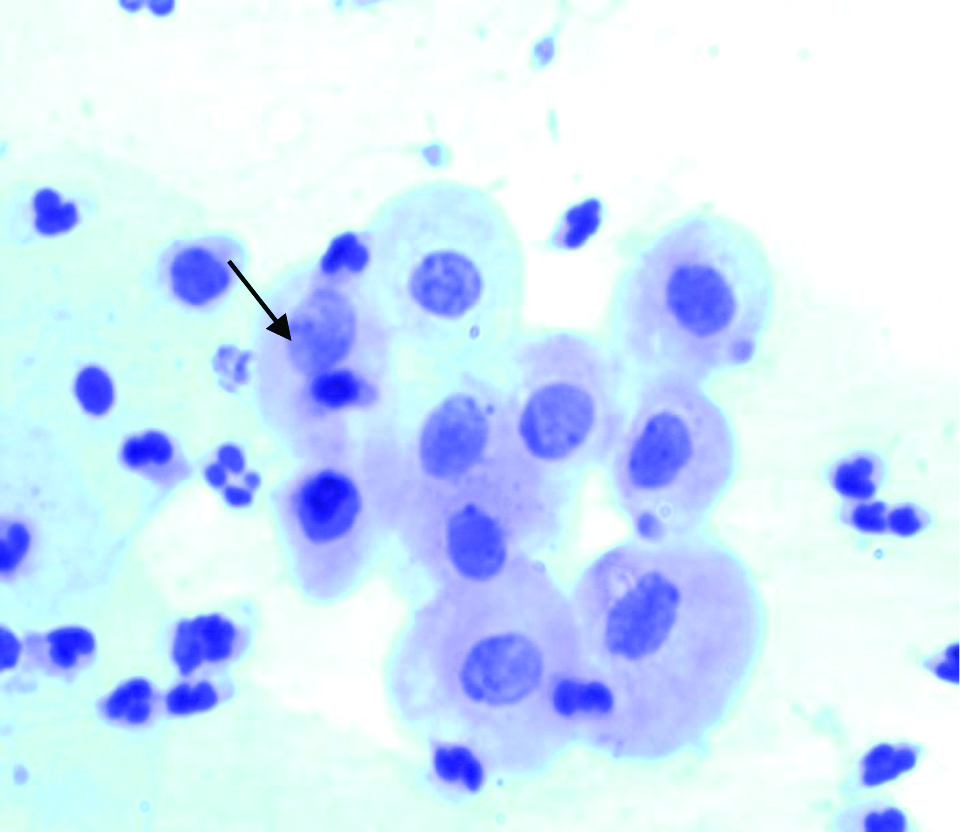
High grade squamous intraepithelial lesion of ectocervix (HSIL).
Parabasal cells showing nuclear enlargement and coarser chromatin (Papx400)
All the diagnosed cases of ASCUS and SIL were given adequate treatment and were called for repeat smear after six months to the hospital but no one turned up for follow-up. This might be due to ignorance regarding the importance of follow-up as most of the women were illiterate and poor. Hence we planned to follow them up in their villages. We paid home visits to all the ASCUS and SIL cases diagnosed and told them about the importance of repeat Pap check-up which will tell whether the lesion has regressed to normal, persisting or has progressed to higher grade. The treatment modalities had to be decided on the Pap result outcome. We called them for repeat check-up on the same venue in the village where the camp was held. Next day at the mini camp, Pap smear was taken in women who turned up.
Follow-up pattern in the ASCUS and SIL case was found to be as follows:
a. ASCUS casesa.1) Adolescent group: Follow-up was available in only 3 of 9 ASCUS cases detected in this group which revealed progression of ASCUS to LSIL in 1 (33.3%) and regression of the lesion to normal in 2 (66.6%)
a.2) Young adult girls: Out of 20 ASCUS cases diagnosed in this group, follow-up was available in 15. Progression to LSIL was seen in 5 (33.3%) while in the remaining 10 (66.6%), the ASCUS had regressed to normal.
a.3) Adult women: Follow-up was available in 22 of the 35 ASCUS cases noticed in this group and progression of ASCUS to LSIL was seen in 6 (27.2%) and regression to normal in the remaining 16 (72.7%)
Thus the progression of ASCUS to LSIL was almost equal in all the three groups.
b. SIL casesb.1) Adolescent group- Follow-up was available in 6 of the 16 LSIL cases diagnosed in this group. Persistence of LSIL was seen in 1 (16.6%) while in the remaining 5 (83.4%), the lesion has regressed to normal.
b.2) Young adult girls- Follow-up was available in 24 out of the 58 LSIL cases diagnosed. Persistence of LSIL was seen in 7 (29.1%), while in the remaining 17 (70.9%), regression of LSIL to normal was seen.
b.3) Adult women- Follow-up were available in 63 of the 145 LSIL cases. The persistence of LSIL was seen in 22(34.9%) while in the remaining 41, LSIL regressed to normal (65.1%).
Follow-up was also available in 3 of the 5 HSIL cases noticed in this group and all 3 showed regression of HSIL to LSIL.
The persistence of SIL was higher in the young adult girls (29.1%) and adult women (34.9%) than 16.6% noticed in the adolescents and this might be due to increased sexual activity and the trauma produced by the repeated child birth.
Different types of infections of STDs have also been studied in the three cohorts of the adolescents, young adult girls and adult women. The incidence of Candida was highest in adolescents (7.2%) and showed declining trend with increasing age to 4.7%. in young adult girls and 1.8% in adult women. The associated SIL rate also showed same trend declining from 14.2% in adolescents to 7.1% in adult women. A reverse trend was seen with trichomonal infection, the incidence being higher in the young adult girls and adult women and no Trichomonas vaginalis infection was seen in the adolescents. Among the viral STDs, only three cases of koilocytosis (HPV) were seen, 2 in young adult girls (0.5%) and 1 in adult women. Only of 1 cases of HSV was seen in the adult women group with associated SIL. Since sexual promiscuity is rare phenomenon in rural women, the STD infection especially viral has been found very low in number.
Though illiteracy rate was found to be very high in the rural women attending camps (63.4%), it was interesting to note that literacy was quite high in the adolescents (87.6%) and showed decline to 67.4% in young adult girls and 47.6% in the adult women and this difference was found to be statistically highly significant (χ2=41.91: p<0.001). Hence literacy plays significant assisting role in counseling and motivating the young rural women for undergoing Pap test as they easily realised the importance of early detection of the disease. However, the SIL rate between the illiterate and literate women in the three cohorts did not reveal any statistical difference (χ2=0.76: p=0.384).
The clinical lesions of cervix was also evaluated in all the three cohorts [Table/Fig-4]. In adolescents, clinical lesions were not so common and only 4 cases of erosion cervix (4.1%) and 1 hypertrophied cervix (1.03%) were diagnosed. The SIL was present in 1 of the 4 cases of erosion cervix (25%) while the only case of hypertrophied cervix also showed SIL. In the young adult girls and adult women, all the 3 types of clinical lesions were seen, the erosion cervix being more common, (8.5% and 4.5%, respectively). A high occurrence of clinical lesions of cervix in the young adult girls and adult women is obviously related to the increasing sexual life cycle of these women. The SIL rate was higher with all 3 types of cervical lesions in the adult women ranging from 38.2% with erosion cervix to 50% with lesions like cystocoele. The study points out the utility of clinically down staging of cervical cancer in the younger women under rural conditions as majority of the cervical lesions were found to harbor the pre-malignant changes in the cervix.
Relation of SIL with clinical lesions of cervix in adolescents, young adult girls and adult women.
| Age group | Erosion cervix | Hypertrophied cervix | Others (Cystocoele, cervicitis etc.,) |
|---|
| No. | SIL rate | No. | SIL rate | No. | SIL rate |
|---|
| Adolescents (97 cases) | 4 (4.1%) | 1 (25%) | 1 (1.03%) | 1 (100%) | - | - |
| Young adult girls (338 cases) | 29 (8.5%) | 9 (31.1%) | 1 (0.2%) | - | 4 (1.2%) | 2 (50%) |
| Adult women (750 cases) | 34 (4.5%) | 13 (38.2%) | 11 (1.4%) | 5 (45.4%) | 10 (1.3%) | 5 (50%) |
Gynaecological symptoms namely vaginal discharge, vague pain in lower abdomen and menstrual disorders were also investigated in the three cohorts [Table/Fig-5]. Vaginal discharge was common in all the three groups and showed rise with increasing age. The pain in lower abdomen was also common in all three groups but the menstrual disorders were low. The SIL rate associated with three gynaecological symptoms was higher in the adolescents than in young adult girls and adult women but the difference was found to be statistically insignificant (vaginal discharge- χ2=0.84: p=0.353, pain in lower abdomen- χ2=5.13: p=0.024, menstrual disorders-χ2=0.64: p=0.793). Hence, all the girls belonging to the three cohorts should be cytologically examined for any onset of SIL if they complain of any of the three gynaecological symptoms.
Relation of SIL with gynaecological symptoms in adolescents, young adult girls and adult women.
| Age group | Vaginaldischarge(581 cases) | Pain in lowerabdomen(315 cases) | Menstrual disorder(170 cases) |
|---|
| No. | SIL rate | No. | SIL rate | No. | SIL rate |
|---|
| Adolescents (97 cases) | 35 (36.1%) | 6 (17.1%) | 22 (22.6%) | 12 (22.7%) | 12 (12.3%) | 2 (16.6%) |
| Young adult girls (338 cases) | 162 (47.9%) | 23 (14.1%) | 110 (32.5%) | 18 (16.3%) | 47 (13.9%) | 4 (8.5%) |
| Adult women (750 cases) | 384 (51.2%) | 42 (10.8%) | 183 (24.4%) | 73 (39.4%) | 111 (14.8%) | 18 (10.1%) |
Number of the cases with different parities and SIL rate in the three groups is shown in [Table/Fig-6]. In the adolescent group, the maximum number of girls were nulliparous (52/97- 53.6%) and the SIL rate was very high in these girls (25%). In the young adult girls and adult women, the number of cases and SIL rate showed increasing trend with rising parity but the difference in the SIL rate in the different parity groups was found to be statistically insignificant (χ2=6.42: p=0.092).
Relation of SIL with parity in adolescents, young adult girls and adult women.
| Parity group | Adolescents | Young adult girls | Adult Women |
|---|
| No. | SIL rate | No. | SIL rate | No | SIL rate |
|---|
| Nulliparity | 52 (53.6%) | 13 (25.0%) | 50 (14.7%) | 2 (4.0%) | 40 (5.3%) | 7 (16.1%) |
| Para 1 | 16 (16.4%) | 1 (6.2%) | 76 (22.4%) | 14 (18.4%) | 36 (4.8%) | 4 (11.1%) |
| Para 2 | 10 (10.3%) | - | 85 (25.1%) | 18 (21.1%) | 141 (18.8%) | 23 (16.3%) |
| Para 3 and above | 19 (19.5%) | 2 (10.5%) | 127 (37.5%) | 24 (18.8%) | 533 (71.0%) | 111 (25.6%) |
Discussion
Cervical cytology carried out in the three cohorts of adolescents, young adult girls and adult women living in the rural areas revealed high ASCUS rate in the adolescents but receding with increasing age. The trend was reverse with SIL, the incidence showing rise with increasing age. The cytological monitoring is thus mandatory in these girls as the marriage in the villages is solemnised at an early age and hence these girls are exposed to the early and prolonged sexual activity. This also becomes imperative as majority of these women complain of vaginal discharge which the study pointed out as the major risk factor of the carcinoma cervix under rural conditions. Further large number of adolescent girls were nulliparous and attended the camp for treatment. The SIL rate was found high in these nulliparous girls. However, WHO recommendations are to screen at least once for every women in the target group of 30-49 years when it is most beneficial. “Screen and treat” is valuable approach [9]. Sadoghi SB et al., have found severe dysplasia as early as at 15 years and invasive carcinoma as early as 20 years while conducting prevelance studies of cervical dysplasia and carcinoma cervix in a national wide planned population [10]. They have stressed for importance of cytological screening programs for sexually active women in view of severe cytopathological changes occurring at young age. Carlson HJ and DeMay KM, have also analysed the mode ages of women with cervical dysplasia and have found that the onset of dysplasia was asymmetrically related with young age [11].
Mount SL and Papillo JL, have also seen 14% abnormal smears in women between 15 to 19 years with only 0.7% of the smears showing HSIL and no case of invasive carcinoma [3]. In another organised cervical screening program in Norway, only 2% of the smears from the adolescents aged 15-19 years were found to be HSIL but LSIL was higher in this group [12]. Wright JD et al., have studied cytology in a large number of adolescents and has found 5.7% of LSIL and 0.7% of HSIL [1]. They have followed LSIL cases noticed in the adolescents for 1,2 and 3 years and have found increased frequency of regression of the lesion from 27.5% to 61.7%, persistence of LSIL declining from 57.6% at one year to 6.7% at three years and progression of LSIL to HSIL from 14.1% to 31.3% at three years. They have also reported that adolescents with cytology reported as SIL carry a similar risk for underlying Cervical Intraepithelial Neoplasia (CIN) as adults. Moscicki AB also found increased rate of regression of LSIL in adolescents and young adult girls and adult women (94%), LSIL regressed to normal within 36 months of detection. Progression of LSIL to HSIL has been reported to vary from 7% to 14% in adult women [13]. They have also seen that only 3% of LSIL in adolescents and young adults went through HSIL. In present study, the regression of the lesion was very common than persistence or progression to SIL. Progression of ASCUS to LSIL was almost equal in all the three cohorts. However, persistence of LSIL was higher in the young adult girls and adult women than in adolescents. It was satisfying to note that none of the LSIL cases progressed to HSIL in all three groups. On contrary, 3 of the 5 HSIL cases found in young adult women regressed to LSIL.
Among the 4 STDs evaluated in the study, Candida was more common especially in adolescents and this may be related to the poor personal genital hygiene prevailing in the rural women. Here it should be pointed out that most of the girls in the study group were literate but their literacy was limited to only primary level education. Trichomonal infection (1.8%) and viral STDs (3 cases of koilocytosis and 1 HSV case were only seen in the young adult girls and adult women). In present study also only 3 cases of koilocytosis (HPV) in urban young girls was seen. On contrary, Muckeman DR has found 10% of the sub clinical HPV infection in the cervix in teenagers [14]. Massad LS and Adrina D, has also reported koilocytosis in 27.6% of the colposcopic directed cervical biopsies in adolescents [15].
Clinical lesions of cervix were more frequent in the young adult girls and adult women than in adolescents. Since SIL was seen in 37.2% of the total 94 cases of cervical lesions, they are presumed to harbour early cases of carcinoma cervix and should be considered as a high risk group. Hurtley SL et al., have also found significant incidence of cervical lesions in the young teenagers and have suggested that this population needs to be screened at regular intervals [16].
Limitation(s)
Though, the authors have tried for follow-up and treatment of all SIL cases through home visits but many of them did not report for Pap check-up. The ignorance of these women about the risk factors of the disease might be the reason. Further, many of the severe cases of vaginal discharge were referred to the hospital for treatment. Also, many of the adolescent’s girls were found nulliparous and SIL rate was very high in these girls. Hence adolescents suffering from primary infertility should be cytologically examined for any pre-cancerous manifestations in the cervix and should be evaluated at regular intervals. These girls were also referred to the hospital for management but it was ironical that were only few of the referred cases could reach the hospital because of poverty and lack of transport.
Conclusion(s)
In conclusion, it is felt that in view of high SIL incidence in adolescents, young girls and adult women, their cytological evaluation is mandatory in the symptomatic cases specially those complaining of vaginal discharge and also those showing cervical lesions and both these groups should be taken as high risk for development of carcinoma cervix. This becomes mandatory under rural conditions where the cytology services are not available. The WHO has also recommended that the key to effective screening program is to reach large number of women at risk with quality screening and treatment. Further the elders in the family of the village should also be educated against the child marriage which put their adolescent girls to prolonged sexual exposure with likelihood of leading to the premalignant changes in the cervix. They should also be taught about the risk factors of the cervical cancer and utility of Pap smear examination for early detection of the disease to advise their female family members.
Funding source: The authors thank Secretary, Era’s Educational Trust of Era University, Lucknow, India for providing the financial assistance for ongoing Rural Cervical Cancer Screening program.