Hyperleukocytosis (Re)Visited- Is it always Leukaemia: A Report of Two Cases and Review of Literature
Ashutosh Rath1, Richa Gupta2
1 Senior Resident, Department of Pathology, Maulana Azad Medical College, Delhi, India.
2 Professor, Department of Pathology, Maulana Azad Medical College, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Richa Gupta, C 502, Prince Apartments, 54 I. P. Extension, Delhi, India.
E-mail: richagupta0209@gmail.com
Hyperleukocytosis is defined as total leukocyte count of more than 100×109/L. Commonly seen in leukaemic conditions, non-leukaemic causes are usually not encountered and thought of. We report two such non-malignant cases of hyperleukocytosis. A six-year old girl presented with fever, cough and respiratory distress with a leukocyte count of 125.97×109/L. Another case is of a two-month old female infant, who presented with fever and respiratory distress and a leukocyte count of 112.27×109/L. The present case thrives to highlight various possible causes of hyperleukocytosis with an emphasis on non-malignant causes. Also, important complications and management of hyperleukocytosis are discussed.
Benign, Leukocytosis, Leukostasis
Case Report 1
A six-year-old girl was admitted with complaints of fever, non-productive cough for one week and severe respiratory distress for the past one day. There was no other significant history. On physical examination, the patient had mild pallor. Respiratory examination revealed tachypnea with bilateral auscultatory rales.
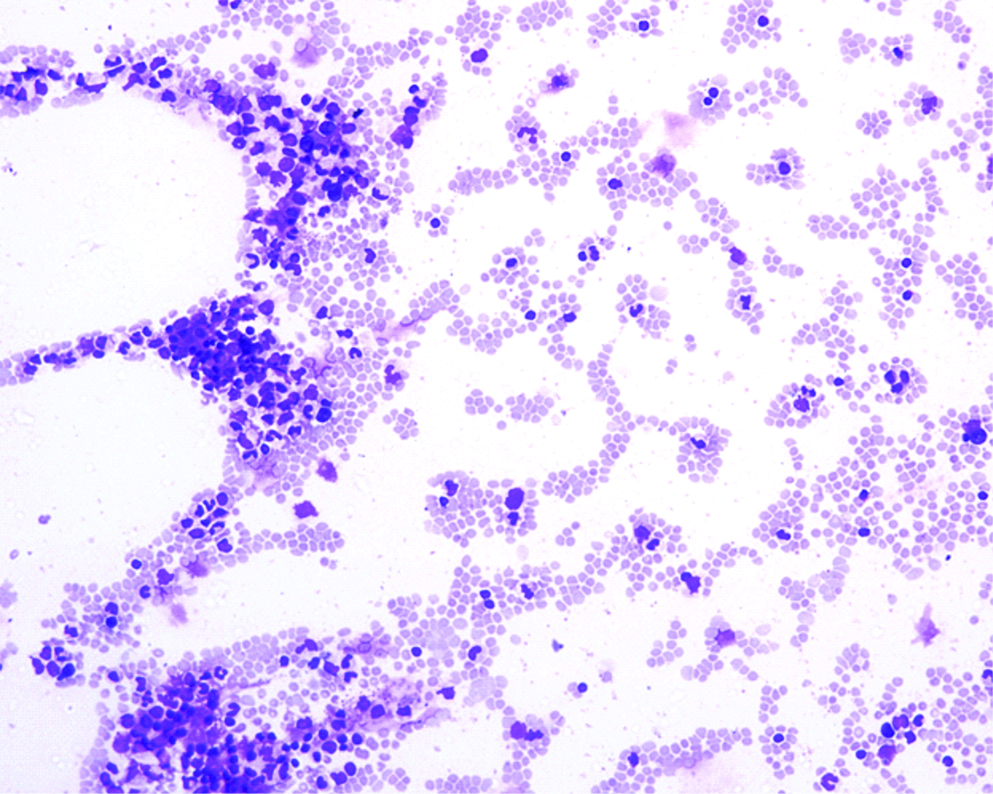
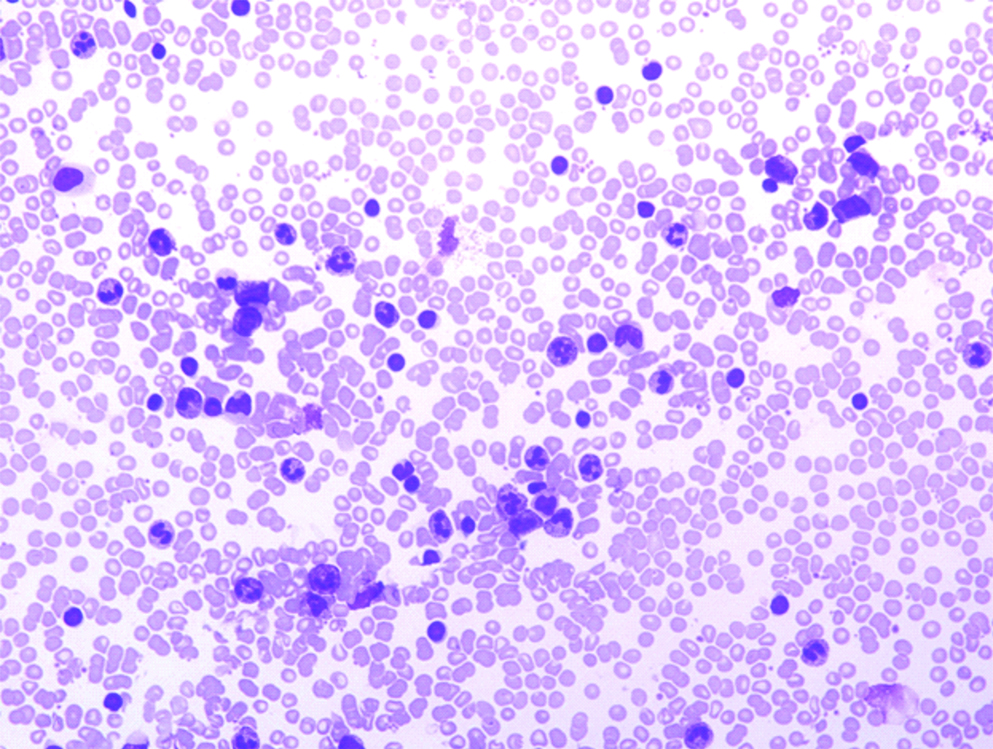
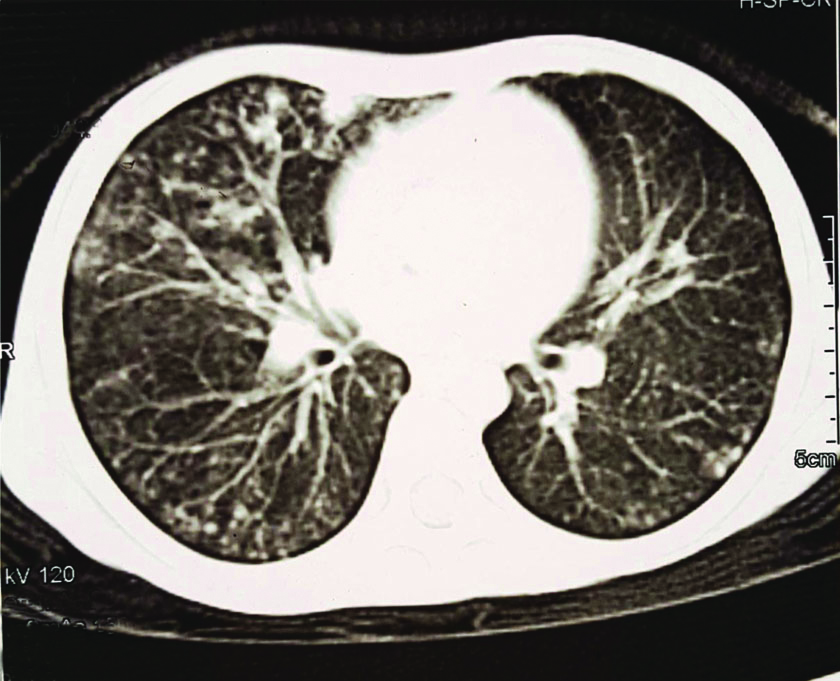
Complete blood count revealed Haemoglobin (Hb) of 10.1 g/dL, Total Leukocyte Count (TLC) of 125.97×109/μL and platelet count of 526×109/L. Peripheral smear examination showed neutrophilic leukocytosis with left shift with band forms- 07%, myelocytes- 06%, metamyelocytes- 08%, neutrophils- 69%, lymphocytes- 08%, monocytes- 01%, eosinophils- 01% and basophils- 0%. No blasts or any other atypical cells were seen in the peripheral smear [Table/Fig-1,2]. Her Erythrocyte Sedimentation Rate (ESR) was 20 mm/hr (normal: <15 mm/hr) and C-Reactive Protein (CRP) was 64.2 mg/L (<10 mg/L- age normal). Neutrophil Acid Phosphatase (NAP) staining was done on peripheral blood neutrophils and 100 neutrophils were graded from 0 to 4, 0 being no staining and 4 being stain obscuring nuclear details. Leukocyte Alkaline Phosphatase (LAP) score was found to be raised (score: 170) [Table/Fig-3]. Chest X-ray revealed multifocal opacities in both lung fields. Subsequent Contrast-Enhanced Computed Tomography (CECT) of the chest revealed bilateral multifocal patchy consolidation with tree in bud opacities in lung window, suggesting an infective aetiology [Table/Fig-4]. Meanwhile, patients her blood culture report came positive for methicillin-resistant Staphylococcus aureus and was started on intravenous Vancomycin along with supportive care. Serial monitoring of TLC revealed a gradual reduction and it returned to the baseline of 15×109/L after eight days. The patient was discharged after 10 days of hospital stay.
Case 1, Peripheral Blood Smear (PBS), Geimsa stain, 100X, hyperleukocytosis with marked tailing.
Case 1, PBS, Geimsa stain, 400X, high WBC count with neutrophils and band forms.
Case 1, NAP (Neutrophil Alkaline Phosphatase), 600X, showing most of the neutrophils with score of 2 and 3.

CECT showing tree in bud opacities.
Case Report 2
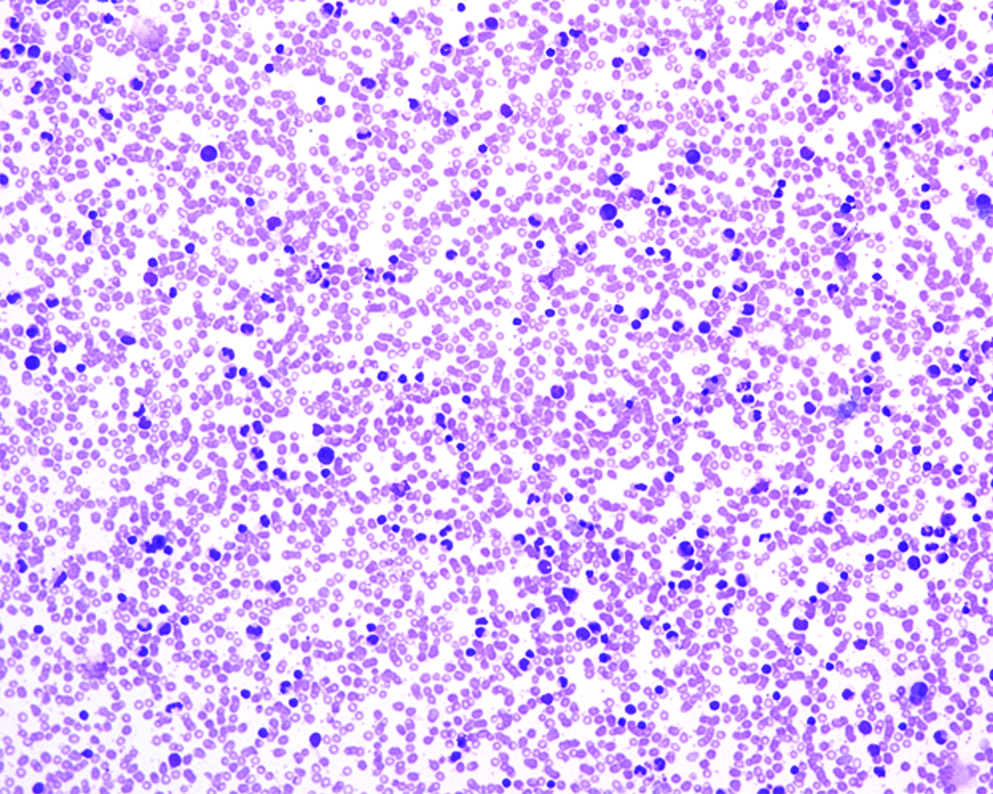
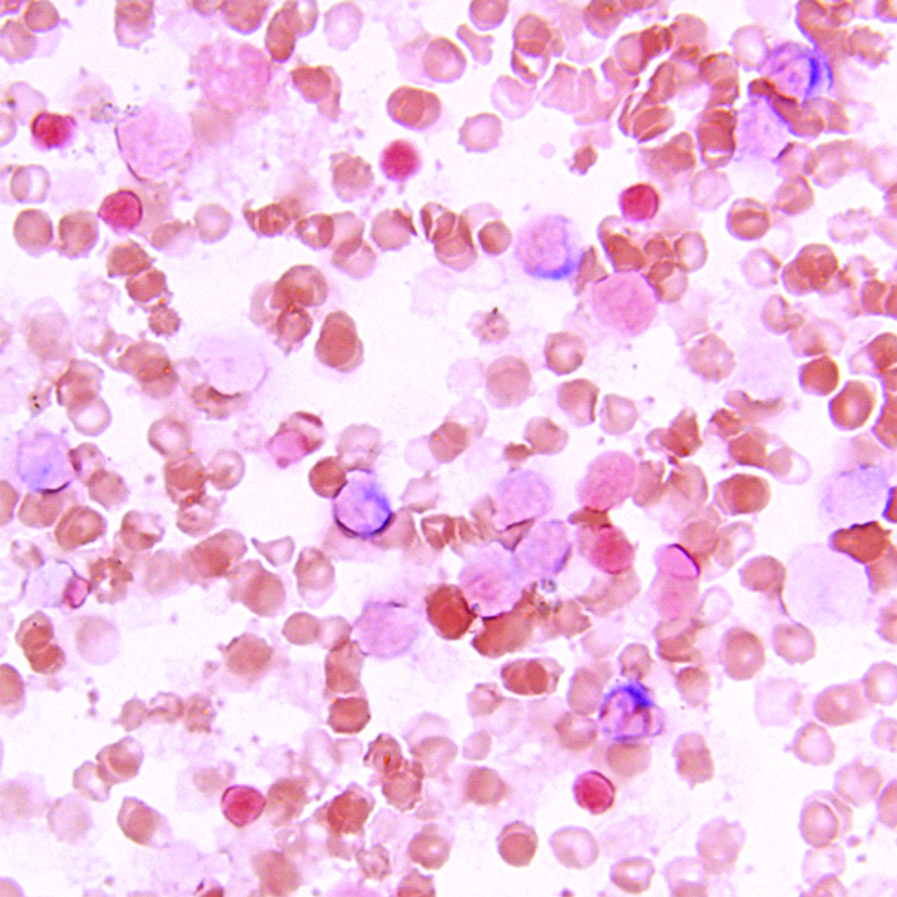
A two-month-old female infant presented with complaints of fever for four days, and decreased breastfeeding and respiratory distress for one day. There was no significant antenatal history, nor was there any history of infection or drug intake. On physical examination, she was lethargic, had pallor and tachypnea. The liver was just palpable below the costal margin. Respiratory examination revealed bilateral auscultatory rales. Complete blood counts revealed moderate anaemia with marked leucocytosis and thrombocytosis (Hb- 7.6 g/dL, TLC- 112.27×109/L, platelet count- 900×109/L). Peripheral smear showed microcytic hypochromic red blood cells and band forms- 12%, myelocytes- 02%, metamyelocytes- 05%, polymorphs- 65%, lymphocytes- 12%, monocytes- 03%, and eosinophils- 01%. No atypical cells were noted [Table/Fig-5]. NAP staining was done and LAP score calculated in a similar way as the first case. The LAP score was slightly raised (Score=150) [Table/Fig-6]. Her ESR was 20 mm/hr and CRP was 32 mg/L. Her chest X-ray showed mild opacity of both lung fields [Table/Fig-7]. Her blood and urine samples were sent for culture and sensitivity tests and she was started on empirical broad-spectrum antibiotics. A CECT scan of the chest was planned the next day; however, she developed extreme respiratory distress and succumbed on the second day of admission. The blood and urine culture reports came negative. Her parents refused to give consent for pathological autopsy.
Case 2, PBS, Geimsa stain, 100X, hyperleukocytosis.
Case 2, PBS, NAP(Neutrophil alkaline phosphatase stain), 600X, showing most of the neutrophils with score of 2 and 3.
Chest X-ray showing opacity in both lung fields.

Discussion
Hyperleukocytosis is defined as total leukocyte count of more than 100×109/L [1]. It’s importance lies in the correct identification of the cause and appropriate management to prevent or treat complications.
Hyperleukocytosis can arise due to several causes. Such alarming increase in counts most often raises the suspicion of leukaemia in clinical practice. Chronic leukaemias, both chronic myeloid leukaemia and chronic lymphocytic leukaemia, though rare in children, are most often malignancies associated with hyperleukocytosis [2,3]. Five percent to 13% cases of Acute Myeloid Leukaemias (AML) and 10% to 30% of Acute Lymphoblastic Leukaemias (ALL) have been found to be associated with hyperleukocytosis [4]. Among other haematologic malignancies, rare case series and reports mention an association with prolymphocytic leukaemias, follicular lymphoma, mantle cell lymphoma and plasma cell leukaemia [5-8]. Infants with Down syndrome may show extreme elevation in WBC count in cases of transient abnormal myelopoiesis [9].
Hyperleukocytosis has also been reported as a paraneoplastic syndrome associated with cutaneous and colonic squamous cell carcinoma and lung adenocarcinoma [10-12]. Pretreatment hyperleukocytosis and initial neutrophilia have been considered independent adverse prognostic factors in oral squamous cell carcinoma, lung cancers, colorectal and anal cancers, renal cell carcinomas and bladder cancers [13].
In contrast to available reports on malignancies associated hyperleukocytosis, non-malignant associations are scant. The most notable association is with pertussis, often lymphocytosis, leading to leukostasis and various other fatal complications [14]. Cases of Leptospirosis have been reported with hyperleukocytosis [15]. A pneumonia outbreak caused by virulent Chlamydia psittaci is reported with cases exhibiting lobar alveolar involvement, hypoxemia, hyperleukocytosis and liver dysfunction. All the patients recovered with no complications after administration of Spiramycin [16]. Among viral aetiology, Epstein Barr Virus (EBV) infection is the most common cause [17]. Neonatal herpes simplex virus infection has also been reported to have extreme leukocytosis of 116.7×109/L in one case report. The baby developed diffuse haemorrhagic encephalomalacia, cortical ischemia and cerebellar hypoplasia and finally succumbed [18]. Rarely, it may be physiological. Hyperleukocytosis and extreme neutrophilia are usually reported in extremely low-birth-weight infants (≤1000 g) [19].
Not much is known about the aetiopathology of hyperleukocytosis except that it is directly caused by the proliferation of malignant clone. In case of carcinomas, increase in β1-integrin expression mediated by G-CSF receptor is proposed to cause increased adhesion and invasiveness of carcinomas. G-CSF expressed by tumour cells thus, seems to be the cause of hyperleukocytosis in such cases [13].
Hyperleukocytosis can lead to various potentially fatal complications and hence is a potential emergency. The most important complications include leukostasis, Tumour Lysis Syndrome (TLS) and Disseminated Intravascular Coagulation (DIC). Leukostasis can manifest in various ways depending on the organs involved. Pulmonary leukostasis may manifest as hypoxemia, dyspnea, and tachypnea with the presence of auscultatory rales and appear radiologically as bilateral interstitial or alveolar infiltrates [20]. Our first case showed tree-in-bud appearance on the lung window of CT scan, which was most probably due to extensively inflamed bronchioles filled with pus due to hyperleukocytosis. Involvement of Central Nervous System (CNS) may lead to a headache, somnolence, dizziness, tinnitus, blurred vision, confusion, delirium and coma with evidence of retinal and intracranial haemorrhage [1]. Rare presentations include myocardial ischemia, acute leg ischemia, bowel infarction, renal vein thrombosis and priapism [21]. DIC in hyperleukocytosis occurs due to high cell turnover causing exposure of tissue factor to the circulation thereby triggering extrinsic pathway of coagulation [1].
Cases with hyperleukocytosis should be investigated thoroughly. In cases of neonates, a large number of nucleated red cells may spuriously cause elevation of TLC and hence a careful peripheral smear examination to look for nucleated red cells or any other atypical cells is important. Investigations related to complications include serum electrolytes, serum calcium and renal function tests for TLS, coagulation profile for DIC, blood gas analysis to look for acidosis, radiological investigations for pulmonary infiltrates, intracranial hemorrhage or any regional mass [22]. Blood sample for blood gas analysis should be transported on ice as hyperleukocytosis may cause spurious hypoxemia [23].
Prevention strategies include aggressive hydration, Allopurinol administration to prevent TLS, correction of metabolic abnormalities and platelet transfusion in cases of severe thrombocytopenia to prevent intracranial haemorrhage [21]. Symptomatic leukostasis can be managed by leukapheresis or exchange transfusion. Cranial irradiation in cases of CNS leukostasis has also been reported to be helpful [1].
Conclusion(s)
Hyperleukocytosis can arise in both leukaemic as well as non-leukaemic conditions. Complications like leukostasis make hyperleukocytosis a medical emergency. Active management is the key to resolve the fatal complications.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Dec 12, 2018
Manual Googling: Jul 31, 2019
iThenticate Software: Dec 18, 2019 (11%)
[1]. Ganzel C, Becker J, Mintz PD, Lazarus HM, Rowe JM, Hyperleukocytosis, leukostasis and leukapheresis: Practice managementBlood Rev 2012 26:117-22.10.1016/j.blre.2012.01.00322364832 [Google Scholar] [CrossRef] [PubMed]
[2]. Kurosawa H, Tanizawa A, Tono C, Watanabe A, Shima H, Ito M, Leukostasis in children and adolescents with chronic myeloid leukemia: Japanese paediatric leukemia/lymphoma study groupPediatr Blood Cancer 2016 63:406-11.10.1002/pbc.2580326485422 [Google Scholar] [CrossRef] [PubMed]
[3]. Shvidel L, Bairey O, Tadmor T, Braester A, Ruchlemer R, Fineman R, Absolute lymphocyte count with extreme hyperleukocytosis does not have a prognostic impact in chronic lymphocytic leukemiaAnticancer Res 2015 35:2861-66. [Google Scholar]
[4]. Porcu P, Cripe LD, Ng EW, Bhatia S, Danielson CM, Orazi A, Hyperleukocytic leukemias and leukostasis: A review of pathophysiology, clinical presentation and managementLeuk Lymphoma 2000 39:01-18.10.3109/1042819000905353410975379 [Google Scholar] [CrossRef] [PubMed]
[5]. Shvidel L, Shtalrid M, Bassous L, Klepfish A, Vorst E, Berrebi A, B-cell prolymphocytic leukemia: A survey of 35 patients emphasizing heterogeneity, prognostic factors and evidence for a group with an indolent courseLeuk Lymphoma 1999 33:169-79.10.3109/1042819990909373910194135 [Google Scholar] [CrossRef] [PubMed]
[6]. Inaba T, Okamoto A, Tatsumi T, Fujita N, Shimazaki C, Hyperleukocytosis in patients with leukemic follicular lymphomaAnn Hematol 2007 86:299-300.10.1007/s00277-006-0232-z17235518 [Google Scholar] [CrossRef] [PubMed]
[7]. Kwan L, Linden J, Gaffney K, Greene M, Vauthrin M, Ramanathan M, Therapeutic leukocytapheresis for improvement in respiratory function in a woman with hyperleukocytosis and mantle cell lymphoma with a circulating small lymphocyte phenotypeJ Clin Apher 2016 31:398-402.10.1002/jca.2141126332581 [Google Scholar] [CrossRef] [PubMed]
[8]. Rastogi P, Ahluwalia J, Parathan KK, Malhotra P, Plasma cell leukemia presenting with hyperleukocytosis and anaplasiaIndian J Hematol Blood Transfus 2017 33:128-29.10.1007/s12288-016-0740-528194071 [Google Scholar] [CrossRef] [PubMed]
[9]. Zwaan MC, Reinhardt D, Hitzler J, Vyas P, Acute leukemias in children with down syndromePediatric Clin North Am 2008 55:53-70.10.1016/j.pcl.2007.11.00118242315 [Google Scholar] [CrossRef] [PubMed]
[10]. Ben Said B, Maitre S, Perrot JL, Labeille B, Cambazard F, Hypercalcemia-hyperleukocytosis paraneoplastic syndrome complicating cutaneous squamous cell carcinoma. Report of two casesRev Med Interne 2010 31:309-11.10.1016/j.revmed.2009.08.00420167400 [Google Scholar] [CrossRef] [PubMed]
[11]. Yitta S, Liang MK, Berman R, Carter JJ, Yee HT, Marks JL, Primary squamous cell carcinoma of the colon associated with hypercalcemia and hyperleukocytosis. Report of a caseDig Surg 2005 22:371-74.10.1159/00009099616424667 [Google Scholar] [CrossRef] [PubMed]
[12]. Sreevatsa A, Babu SM, Babu GK, Suresh TM, Hyperleukocytosis, an unusual paraneoplastic manifestation of lung cancer: Case report and review of literatureJ Cancer Res Ther 2015 11:66910.4103/0973-1482.15186526458717 [Google Scholar] [CrossRef] [PubMed]
[13]. Su Z, Mao YP, OuYang PY, Tang J, Xie FY, Initial Hyperleukocytosis and neutrophilia in nasopharyngeal carcinoma: Incidence and prognostic impactPLoS One 2015 :1010.1371/journal.pone.013675226336064 [Google Scholar] [CrossRef] [PubMed]
[14]. Eltermann T, Wossner R, Liese J, Wieg C, Wirbelauer J, Thomas W, Fatal pertussis in a preterm with hyperleukocytosis and necrotizing enterocolitis: Considerations on pathogenesis and preventionKlin Padiatr 2012 224:461-62.10.1055/s-0032-131267622821286 [Google Scholar] [CrossRef] [PubMed]
[15]. Magne MC, Ondounda M, Mbethe LG, Mounguengui D, Nzenze JR, Leptospirosis in Libreville (Gabon): Four cases [Abstract]Medecine et sante tropicales 2013 23:347-50.10.1684/mst.2013.022824095884 [Google Scholar] [CrossRef] [PubMed]
[16]. Goupil F, Pelle-Duporte D, Kouyoumdjian S, Carbonnelle B, Tuchais E, Severe pneumonia with a pneumococcal aspect during an ornithosis outbreak [Abstract]Presse medicale 1998 27:1084-88. [Google Scholar]
[17]. Sarbay H, Polat A, Mete E, Balci YI, Akin M, Pertussis-like syndrome associated with adenovirus presenting with hyperleukocytosis: Case reportNorth Clin Istanb 2016 3:140-42.10.14744/nci.2015.1580728058402 [Google Scholar] [CrossRef] [PubMed]
[18]. Underwood MA, Wartell AE, Borghese RA, Hyperleukocytosis in a premature infant with intrauterine herpes simplex encephalitisJ Perinatol 2012 32:469-72.10.1038/jp.2011.13822643292 [Google Scholar] [CrossRef] [PubMed]
[19]. Parvez Y, Mathew AG, Hyperleukocytosis in newborn: A diagnosis of concernIndian J Hematol Blood Transfus 2014 30:131-32.10.1007/s12288-013-0286-825332558 [Google Scholar] [CrossRef] [PubMed]
[20]. Piro E, Carillio G, Levato L, Kropp M, Molica S, Reversal of leukostasis-related pulmonary distress syndrome after leukapheresis and low-dose chemotherapy in acute myeloid leukemiaJ Clin Oncol 2011 29:e725-26.10.1200/JCO.2011.36.275621825265 [Google Scholar] [CrossRef] [PubMed]
[21]. Ruggiero A, Rizzo D, Amato M, Riccardi R, Management of hyperleukocytosisCurr Treat Options Oncol 2016 17:710.1007/s11864-015-0387-826820286 [Google Scholar] [CrossRef] [PubMed]
[22]. Jain R, Bansal D, Marwaha RK, Hyperleukocytosis: Emergency managementIndian J Pediatr 2013 80:144-48.10.1007/s12098-012-0917-323180411 [Google Scholar] [CrossRef] [PubMed]
[23]. Van de Louw A, Desai RJ, Schneider CW, Claxton DF, Hypoxemia during extreme hyperleukocytosis: How spurious?Respir Care 2016 61:08-14.10.4187/respcare.0419626420901 [Google Scholar] [CrossRef] [PubMed]