Cystic Hygroma of Bilateral Parotid Glands and Neck
Sanjay M Khaladkar1, Suhani Jain2, Amit Arun Choure3, Radhika K Jaipuria4
1 Professor, Department of Radiodiagnosis, Dr. D.Y. Patil Medical College, Pimpri, Pune, Maharashtra, India.
2 Resident, Department of Radiodiagnosis, Dr. D.Y. Patil Medical College, Pimpri, Pune, Maharashtra, India.
3 Resident, Department of Radiodiagnosis, Dr. D.Y. Patil Medical College, Pimpri, Pune, Maharashtra, India.
4 Resident, Department of Radiodiagnosis, Dr. D.Y. Patil Medical College, Pimpri, Pune, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Sanjay M Khaladkar, Professor, Department of Radiodiagnosis, DR. D.Y. Patil Vidyapeeth, Pimpri, Pune, Maharashtra, India.
E-mail: drsanjaymkhaladkar@gmail.com
Lymphangiomas are congenital malformations of lymphatic system. Most of the lymphangiomas appear before the age of 2 years. Microscopically lymphangiomas are capillary, cavernous and cystic. Cystic hygromas usually show extensive infiltration in surrounding tissues. Cystic hygromas of the parotid gland are rare. It is more common for cystic hygromas of neck to secondarily involve the parotid gland. Increase in the size of the mass is associated with haemorrhage into the cyst and upper respiratory tract infection. Recurrence is common if incompletely excised. Here, authors report a case of 16-month-old child (female) presented with swelling in bilateral parotid regions for 15 days. USG, CT and MRI showed bilaterally enlarged parotid glands showing multilocular cystic lesions of variable sizes with extension in bilateral masticator spaces, parapharyngeal and carotid spaces, posterior triangle and bilateral tonsillar fossa. Small cystic hygroma was also seen in superior mediastinum in prevascular space. Bilateral parotid gland involvement is the peculiar finding of the present case.
Congenital malformation, Lymphangioma, Venolymphatic malformation
Case Report
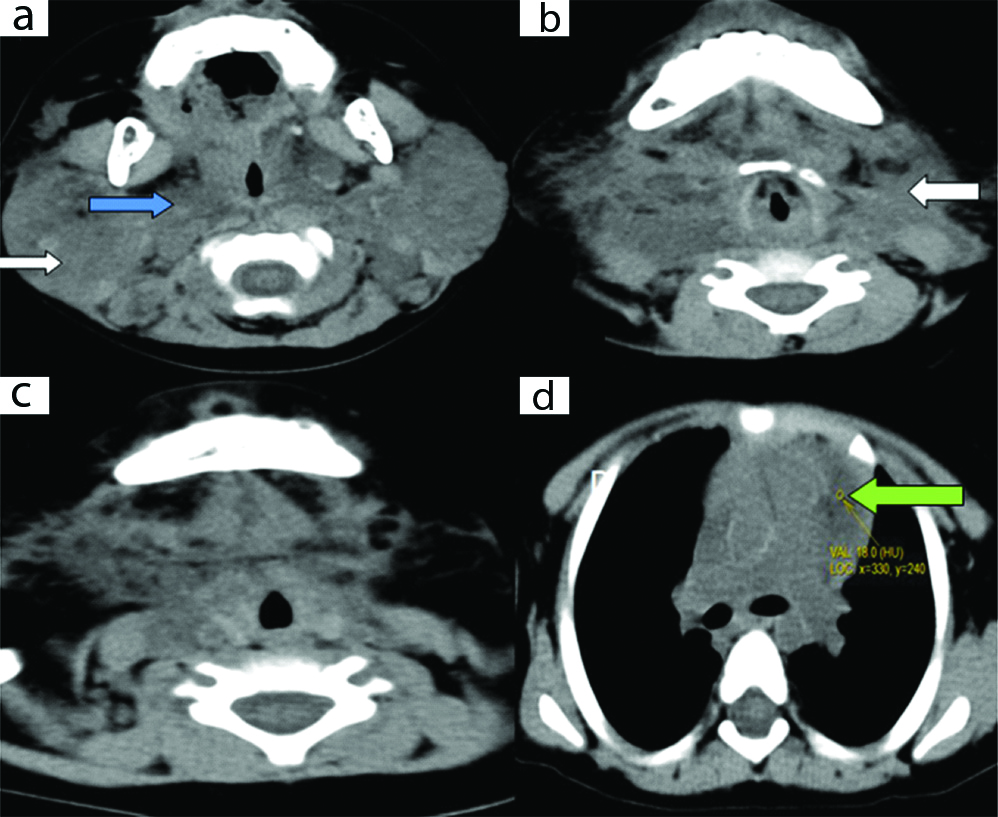
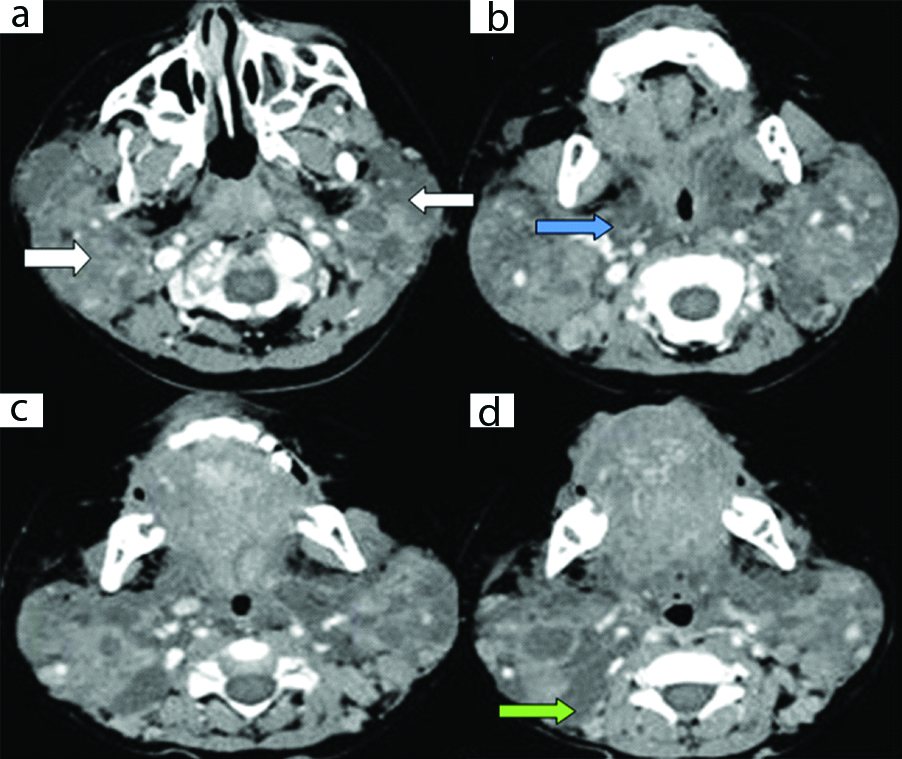
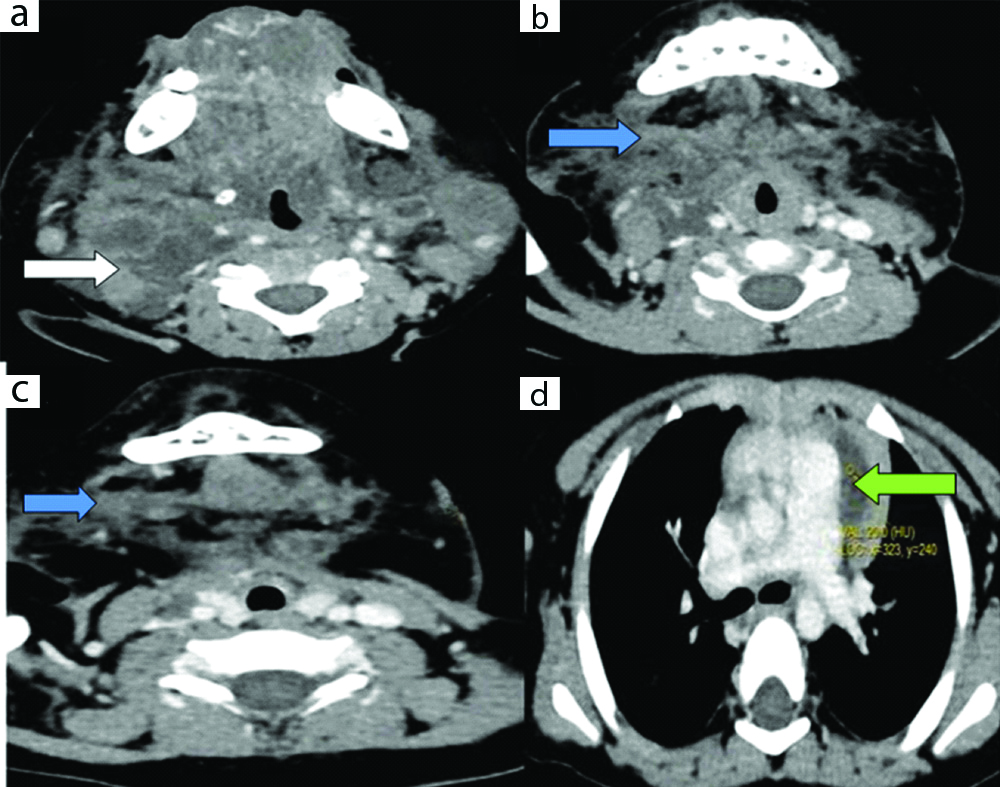
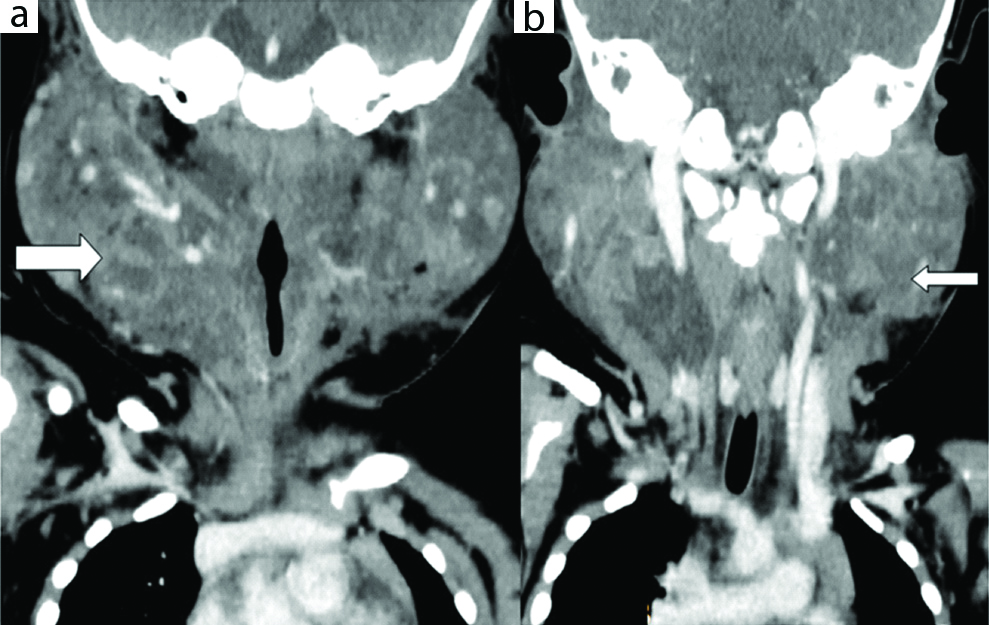
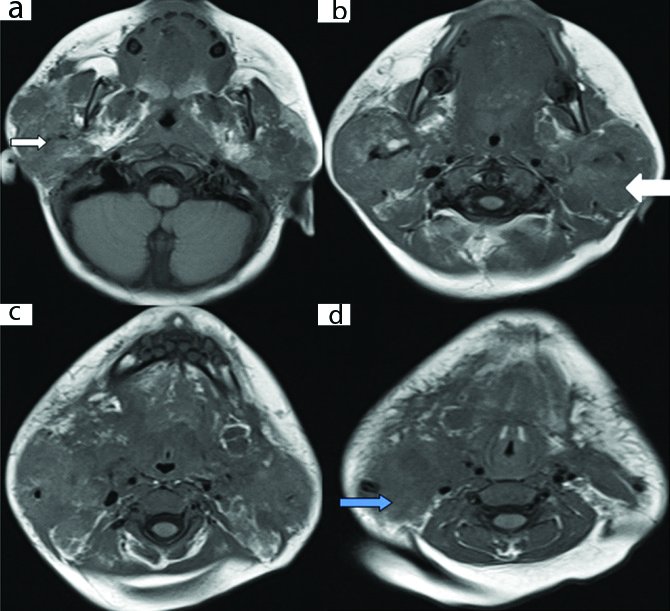
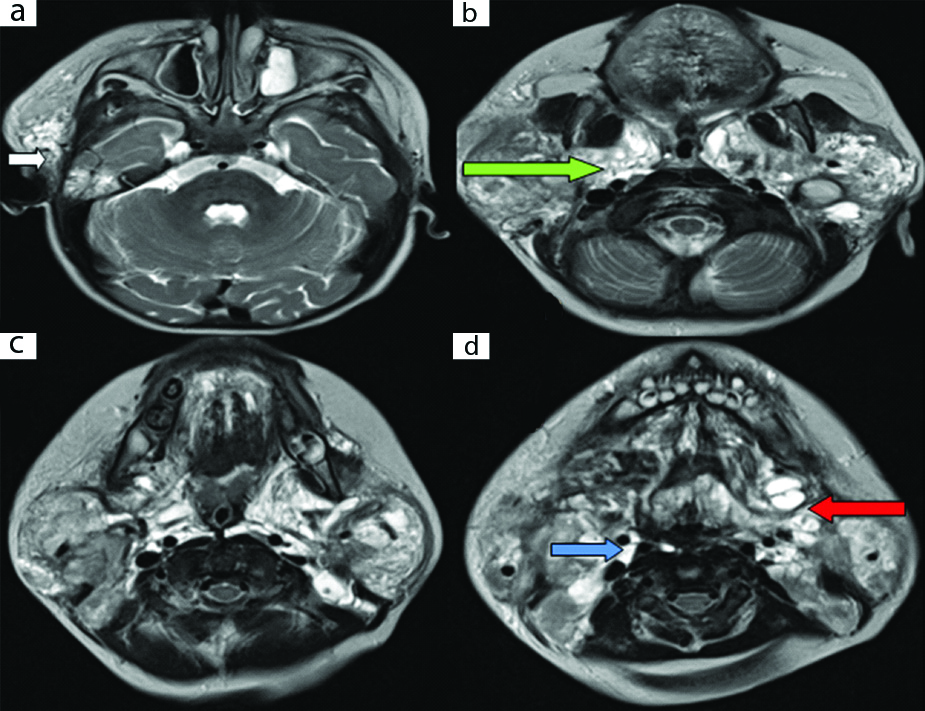
A 16-month-old child (female) presented with swelling in bilateral parotid regions for 15 days. There was no history of cough, breathing difficulty or difficulty in swallowing. There was no history of recent viral infection. Previous records showed normal karyotype. As there was a history of previous surgery, this was a case of recurrence. Clinically there was bilateral parotid swelling and diffuse swelling in neck bilaterally which was soft and cystic in nature. Ultrasound (USG) of neck showed bilaterally enlarged parotid glands with heterogeneous echotexture due to multiple small anechoic cystic lesions with no vascularity. Multiple cystic lesions were seen in bilateral submandibular regions and posterior triangles. Plain and contrast enhanced CT scan of neck showed bilaterally enlarged parotid glands due to multiple cystic lesions of variable sizes, showing mild peripheral rim of enhancement on contrast [Table/Fig-1,2,3 and 4]. These cystic lesions were extending in right temporal region, prevertebral space, left masseter, bilateral parapharyngeal spaces, bilateral posterior triangles, bilateral submandibular regions. A cystic lesion of size 20mm × 7mm was noted in superior mediastinum in prevascular space.
Plain axial CT scan of neck showing bilateral enlarged parotids due to multilocular hypodense cystic lesions (a, b: white arrows), extending in prevertebral space, bilateral parapharyngeal spaces (a: blue arrow), bilateral posterior triangles, bilateral submandibular regions and superior mediastinum in prevascular space (d: green arrow).
Contrast enhanced axial CT scan of neck showing bilateral enlarged parotids due to multilocular hypodense cystic lesions (a: white arrows); extending in bilateral parapharyngeal spaces (b: blue arrow), bilateral posterior triangles (d: green arrow).
Contrast enhanced axial CT scan of neck showing bilateral enlarged parotids due to multilocular hypodense cystic lesions (a: white arrow) extending in bilateral parapharyngeal spaces and tonsillar fossa, bilateral posterior triangles, bilateral submandibular regions (b,c: blue arrow), right carotid space and superior mediastinum in prevascular space (d: green arrow).
Contrast enhanced CT scan of neck (coronal) showing multilocular hypodense cystic lesions in bilateral parotids (a, b: white arrows).
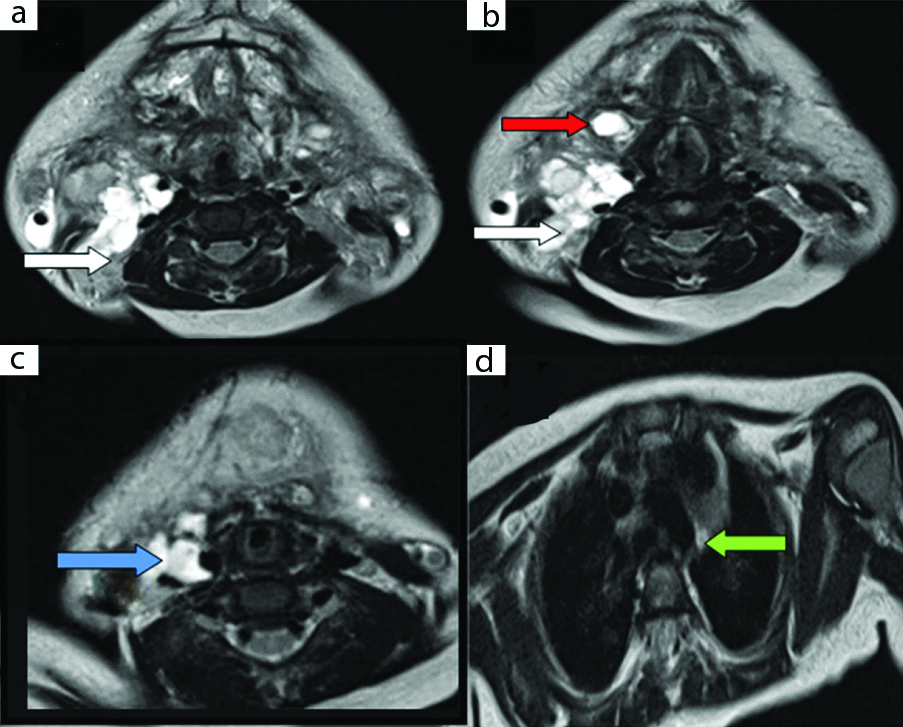
MRI of neck showed bilaterally enlarged parotid glands showing multilocular cystic lesions of variable sizes appearing hypointense on T1W1 and hyperintense on T2W1 and STIR without restriction on DWI [Table/Fig-5,6,7,8 and 9]. It involved posterior portion of left masseter muscle. Anteriorly, it was extending in bilateral masticator and submandibular spaces. Superiorly, it was extending in right temporal region. Inferiorly, it was extending in superior mediastinum in prevascular space where it measured approximately 27mm × 5mm. Posteriorly, it was extending in bilateral parapharyngeal and carotid spaces, posterior triangles, bilateral tonsillar fossa and prevertebral space. Medially, it was extending in base of tongue and pre-epiglottic space. Laterally, on right side, it was extending between Common Carotid Artery (CCA) and Internal Jugular Vein (IJV) side which was splayed in lower neck. It appeared to be encasing right CCA, Internal Carotid Artery (ICA), External Carotid Artery (ECA) and retromandibular vein. Laterally on left side, it was extending between left sternomastoid and platysma. Both submandibular and salivary glands were distinctly not seen. Diagnosis of residual or recurrence of cystic hygroma in various neck spaces, bilateral parotid glands and small cystic hygroma in superior mediastinum was made. Histopathological report showed large irregular shaped vascular spaces lined by flattened epithelial cells with fibroblastic stroma showing lymphocytes suggestive of cystic hygroma. Surgical intervention was advised, but parents were not willing for the same.
Plain axial MRI scan of neck (axial T1) showing bilateral enlarged parotids due to multilocular hypointense cystic lesions (a, b: white arrows) extending in bilateral parapharyngeal spaces, bilateral posterior triangles (d: blue arrow).
Plain axial MRI scan of neck (axial T2) showing bilateral enlarged parotids due to multilocular hyperintense cystic lesions extending in right temporal region (a: white arrow); prevertebral space, bilateral parapharyngeal spaces (b: green arrow), bilateral posterior triangles, bilateral submandibular regions (d: red arrow) and carotid spaces (d: blue arrow).
Plain axial MRI scan of neck (axial T2) showing multilocular hyperintense cystic lesions in bilateral posterior triangles (a, b: white arrow), bilateral submandibular regions (b: red arrow); right carotid space (c: blue arrow) and superior mediastinum in prevascular space (d: green arrow).
Plain axial MRI scan of neck (axial STIR) showing multilocular hyperintense cystic lesions in bilateral parotids (a: white arrow), extending in prevertebral space, left masseter, bilateral parapharyngeal space (a: red arrow); bilateral posterior triangles (c: blue arrow), carotid spaces (d: green arrows).
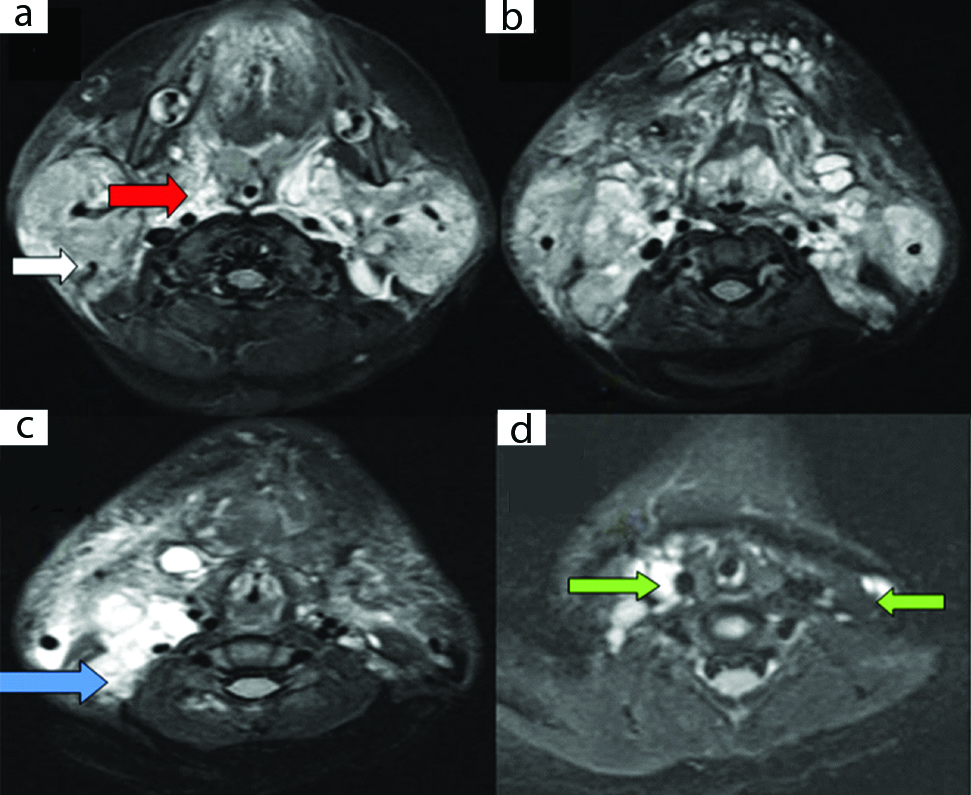
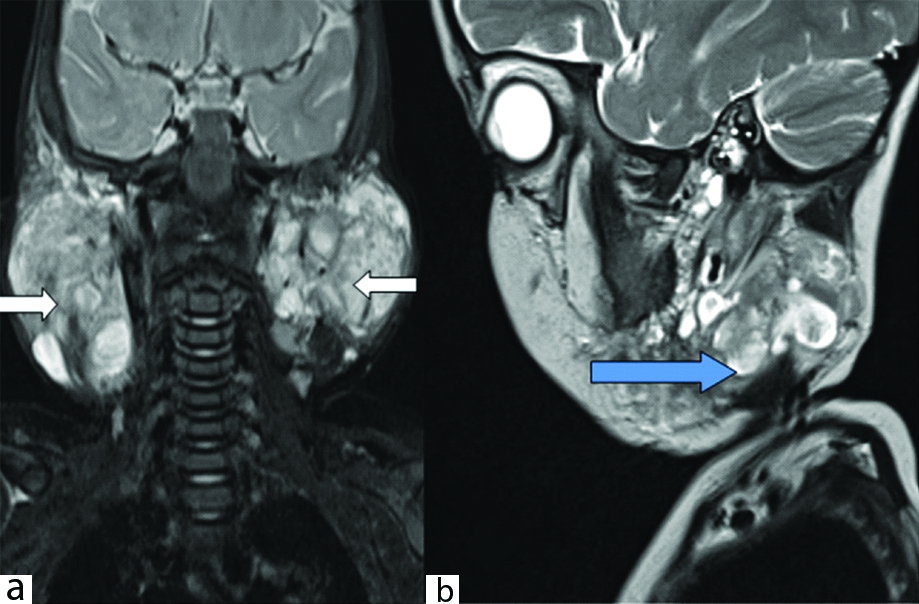
Plain MRI scan of neck showing multilocular hyperintense cystic lesions in bilateral parotids (a: coronal STIR white arrows) and in left parotid (b: sagittal T2 blue arrow).
Discussion
Lymphangiomas are congenital malformations of lymphatic system. Most of the lymphangiomas appear before the age of 2 years [1]. Most children with lymphatic malformations have a normal karyotype however, increased incidence is found in trisomy 18 and 13, Downs, Turners, Roberts and Noonan’s syndrome. They are slow growing with no malignant potential [2]. It is estimated 75-80% of cystic hygromas occur in neck and face, 20% occur in axilla and 5% occur in mediastinum, abdominal cavity (liver, spleen, colon), retroperitoneum, kidney, scrotum and skeletal system. About 50-60% of hygromas appear before the end of 1st year of life, while 80-90% occur before the 2nd year. Rarely, they appear in adults [3].
The etiopathogenesis of Lymphangiomatosis is not clearly understood. The accepted theory is sequestration of dysplastic lymphatic tissue in a target tissue during the fetal development. Lymphangiomas can be acquired after trauma, surgery, infection and chronic inflammation. Cystic hygromas usually show extensive infiltration in surrounding tissues and post-surgical difficulties. Clinically, lymphangiomas appear as compressible, non-tender and trans illuminant mass. Overlying skin is usually normal [1]. Cystic hygromas of the parotid gland are rare. Parotid gland is usually secondarily involved by cystic hygroma of neck. Haemorrhage into the cyst and upper respiratory tract infection cause increase in size of the mass. Involution of lymphangiomas occur in 15-70% of cases during the first 20 years of life. Even after involution, they may re-fill with fluid and subsequently enlarge. Untreated cystic hygromas can cause mass effect on trachea or oesophagus. Malignant transformation to lymphangiosarcoma has never been reported. Recurrence rate is 10-15% within 1 year after excision. Residual lymphangiomas can become atrophic, remain static or fibrose. They can recur if incompletely excised [4].
A few cases of cystic hygroma in parotid gland have been reported [1]. Two cases of cystic hygroma of parotid glands were reported in adults by Berri T et al., and Kandhasamy SC et al., [1,4]. One case of cystic hygroma in parotid was reported by Stenson RN et al., [5]. Another case was reported by Goshen S and Ophir D, [6]. Both the cases were unilateral and left. The present authors extensively searched the English literature and found that this is the first case of bilateral parotid cystic hygroma. Comparison of the index case with previous case reports is shown in [Table/Fig-10].
Comparison of the index case findings with published literature [1,4,5,6,8].
| Previous cases | Age group involved | Unilateral/bilateral | Unilocular/Multilocular | Superficial, deep lobe of parotid involvement | Extension into neck | Recurrence during follow-up |
|---|
| Stenson KN et al., [5] | Paediatric (9 years) | Unilateral (left parotid) | multilocular | Both superficial and deep lobes of parotid involved | Not seen | No recurrence after 12 months |
| Berri T et al., [1] | Adults (66 years) | Unilateral (right parotid) | unilocular | Superficial lobe involved | Not seen | Not available |
| Goshen S Ophir D, [6] | Paediatric (10 years) | Unilateral (left parotid) | multilocular | Superficial and deep lobes involved | seen | No recurrence after 18 months follow-up. |
| Tsui SC et al., [8] | Paediatric (10 years) | Unilateral (left parotid) | unilocular | Superficial and deep lobes involved | Seen, involved parapharyngeal space. | Refused surgical treatment. |
| Kandhasamy SC et al., [4] | Adults (80 years) | Unilateral (right parotid) | unilocular | Superficial lobe involved | Not seen | No recurrence in 6 months period |
| Present case | Paediatric (16 months) | bilateral | multilocular | Both superficial and deep lobes of parotid involved | Extensive involvement of neck spaces on either side with extension in superior mediastinum in prevascular space | This was a case of recurrence.Patient refused surgical intervention. |
Lymphangiomas can be simple, cavernous and cystic [7]. The mass can invade the cervical muscles and infiltrate between the great blood vessels throughout the parapharyngeal space [6]. On USG, cystic hygromas are multilocular, multicystic, multiseptate lesion with surrounding irregular walls. No vascularity is detected on doppler ultrasound. On CT, it appears as a multilocular, multicystic thin walled lesion with septa in parotid gland. Contrast study shows enhancement in 80% of cases. On MRI, it appears hypointense on T1W1 and hyperintense on T2W1 and STIR with well demarcated margins. Both CT and MRI are useful in evaluating the extent of cystic hygroma and effect on adjacent structures. MRI is the imaging method of choice due to multiplanar imaging and superior soft tissue discrimination, lack of radiation and no need of contrast [1]. Fine Needle Aspiration Cytology (FNAC) shows yellow or serosanguineous fluid showing mature lymphocytes and histiocytes. Evolution of lymphangiomas occur in three ways: a) Spontaneous regression; b) Slow progression; c) Spontaneous or traumatic haemorrhage or infection in the cyst causing its rapid enlargement. Ulceration or rupture of cyst and compression of adjacent nerve may occur. It can also infiltrate in adjoining bone and cause its osteolysis-(Gorham’s stout syndrome) [1].
Differential diagnosis of parotid lesions are lymphoepithelial cysts, hemangioma, dermoid cyst, adenoma, neurofibroma or schwannoma arising from intraparotid facial nerve and lymphomas [1].
Intraparotid schwannomas, neurofibromas and lymphomas are solid. Intraparotid dermoid cyst is cystic and shows lipid content appearing hyperintense on T1WI. Parotid hemangioma can be differentiated by identification of feeding artery and draining vein and presence of vascularity.
Various treatment options are available like Aspiration of the cyst in emergency to decompress the cyst, however, recurrence usually occurs. Symptomatic cysts are excised surgically with complete excision to reduce the risk of recurrence and enucleation of superficial or total parotidectomy can also be considered [6].
Percutaneous sclerotherapy can be done with sclerosing agent bleomycin, alcohol, Picibanil (OK-432), triamcinolone and fibrin sealant. It is useful when surgery is difficult or when there is recurrence. The sclerosing agent provokes a local inflammation with resultant retraction of the lesion. OK-432 gives good results in microcystic lesions. Laser excision is not useful due to high rate of recurrence. Radiotherapy is not useful due to risk of malignant transformation [1].
Conclusion(s)
Cystic hygromas of the parotid gland are rare. It is more common for cystic hygromas of neck to secondarily involve the parotid gland. Imaging with CT or MRI pre-operatively is mandatory to detect its extent due to its infiltrative nature to adjacent structures as chances of reoccurrence are high. Surgery is the treatment of choice. However, it is not possible to obtain complete surgical resection hence sclerotherapy after partial excision of the lesion is the other alternative.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Sep 30, 2019
Manual Googling: Nov 29, 2019
iThenticate Software: Dec 12, 2019 (12%)
[1]. Berri T, Azizi S, Large cystic lymphangioma of the parotid gland in the adultEgyptian Journal of Ear, Nose, Throat and Allied Sciences 2014 15(3):259-61.10.1016/j.ejenta.2014.07.003 [Google Scholar] [CrossRef]
[2]. Serafino MD, Mercogliano C, Severino R, Lisanti F, Esposito F, Rocca R, Cystic Hygroma of the Neck: Ultrasound FindingsOpen Journal of Radiology 2016 6(2):121-24.10.4236/ojrad.2016.62018 [Google Scholar] [CrossRef]
[3]. Mansingani S, Desai N, Pancholi A, Parajapati A, Vohra P A, Raniga S, A case of axillary cystic hygromaIndian J Radiol Imaging 2005 15:517-19.10.4103/0971-3026.28786 [Google Scholar] [CrossRef]
[4]. Kandhasamy SC, Raju TR, Sahoo AK, Gunasekaran G, Adult Cystic Lymphangioma of the Parotid Gland: An Unwonted PresentationCureus 2018 10(5):e2644 [Google Scholar]
[5]. Stenson KM, Mishelle J, Toriumi DM, Cystic hygroma of the parotid glandAnn Otol Rhinol Laryngol 1991 100(6):518-20.10.1177/0003489491100006172058995 [Google Scholar] [CrossRef] [PubMed]
[6]. Goshen S, Ophir D, Cystic hygroma of the parotid glandJLaryngol Otol 1993 107(9):855-57.10.1017/S00222151001246368228610 [Google Scholar] [CrossRef] [PubMed]
[7]. Sheth S, Nussbaum AR, Hutchins GM, Sanders RC, Cystichygromas in children: sonographic-pathologic correlationRadiology 1987 162(3):821-24.10.1148/radiology.162.3.35440383544038 [Google Scholar] [CrossRef] [PubMed]
[8]. Tsui SC, Huang JL, Parotidlymphangioma. A case reportInt J Pediatr Otorhinolaryngol 1996 34(3):273-78.10.1016/0165-5876(95)01274-5 [Google Scholar] [CrossRef]