Superior Vena Cava (SVC) syndrome can arise due to obstruction of blood flow in the SVC. Haemodialysis (HD) catheter is very commonly inserted into the SVC, and can lead to thrombotic complications, thereby resulting in signs and symptoms of SVC syndrome. We hereby report a case of a 59-year-old male patient from Western Orissa (India) who was diagnosed with end-stage renal disease and was maintained on regular haemodialysis via right jugular vein dual lumen cuffed tunnelled (Permcath) catheter for five months and presented with signs and symptoms suggestive of SVC obstruction. His symptoms worsened, for which, he was taken for percutaneous transluminal angioplasty to SVC followed by stenting of right brachiocephalic vein and SVC. The SVC syndrome can be a potential consequence of HD catheter-related thrombosis. In view of frequency of HD catheter placement, nephrologists should be aware of these potential complications in any patient with HD catheter-related thrombosis and appropriate therapeutic intervention including stenting when required.
Case Report
A 59-year-old male patient from Western Orissa (India), presented in February 2017 with accelerated hypertension and impaired renal function. His evaluation was suggestive of bilateral small kidneys with features of chronic kidney disease. He was started on emergency dialysis via right femoral double lumen temporary dialysis catheter. The need of long-term renal replacement therapy was discussed. At this point of time, in view of swelling in both upper extremities, an Arteriovenous Fistula (AVF) could not be created. Therefore, as a mode of dialysis access for a longer duration, Permcath insertion was planned. In February 2017, he was given a dual lumen tunnelled catheter (Permcath) into right Internal Jugular Vein (IJV) in the Cath lab under fluoroscopic guidance. His haemodialysis was continued via this permcath three times a week.
In the meantime, a left brachiocephalic AVF was successfully created in May 2017. After AVF maturation in June 2017, we started using this access for haemodialysis. After a few sessions of haemodialysis via AVF were done successfully, his Permcath was removed in last week of July 2017.
However, after a few more successful sessions of dialysis his left brachiocephalic AVF stopped working. And he was given a temporary non-cuffed haemodialysis catheter into right IJV.
While he was undergoing dialysis via this access, the patient started to complain of dyspnoea, facial swelling, and visible dilated engorged neck veins and collateral veins over the chest wall. In view of the clinical picture suggestive of central venous catheter stenosis, he was shifted to Intensive Care Unit (ICU) for further evaluation and management.
Chest and neck imaging were performed on the day of admission. Interventional cardiology consultation was taken and patient was planned for angiography.
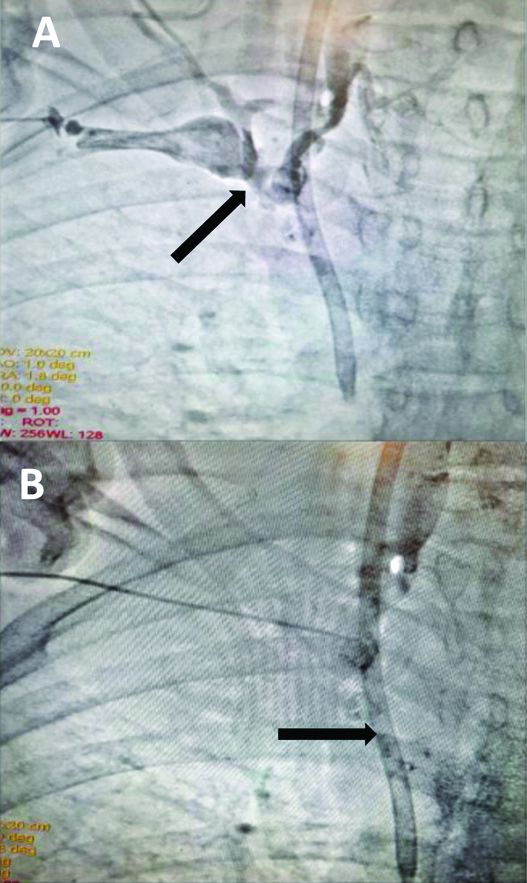
Angiography was suggestive of right brachiocephalic vein thrombus causing nearly 100% occlusion extending into SVC [Table/Fig-1a,b]. In the setting of SVC thrombus, he was initiated on a continuous Intravenous (IV) heparin infusion. The dialysis catheter in IJV was also removed. He was continued on haemodialysis via left femoral access.
Thrombosis of right brachiocephalic vein extending in to SVC with dialysis catheter in situ.
His blood pressure was 156/84 mmHg, pulse rate: 88 b/m with tachypnoea: 30 b/m. Mild peripheral cyanosis, neck and facial swelling, and visible dilated collateral veins over the chest wall were observed. Laboratory investigations showed haemoglobin: 11.3 g/dL, total leucocytes count: 11600/mm3. A hypercoagulable status work up was negative as the coagulation study showed anti-thrombin III activity at 90% (normal levels being 80%-120%), protein C activity at 120% (normal levels being 70%-140%) and protein S activity at 96% (normal levels being 60%-140%).
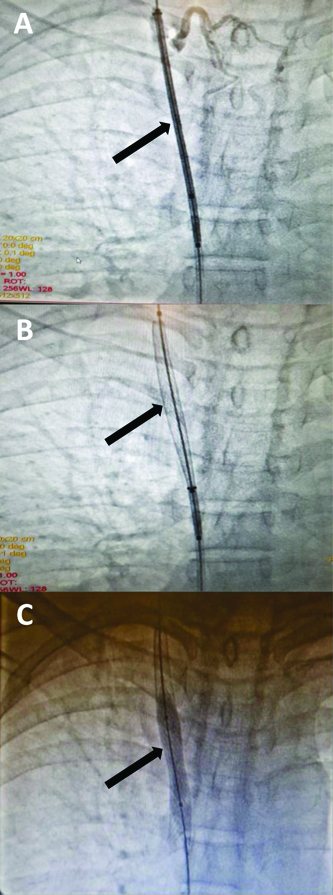
After three days of hospitalisation, the symptoms of SVC syndrome persisted despite continuous IV heparin, with worsening of dyspnoea, facial swelling, and engorgement of neck veins. Repeat imaging of the chest demonstrated unchanged adherent, near-occlusive thrombus in the right brachiocephalic vein, extending through to the SVC. In view of this and significant clinical condition deterioration of the patient, he was taken for percutaneous transluminal balloon angioplasty with stenting of right brachiocephalic vein and SVC [Table/Fig-2a-c]. Post procedure, the flow was good with restored patency and there was marked improvement in clinical condition of the patient. In view of the coexisting coronary artery disease, CAG was done and for the 80% stenosis of Right Coronary Artery (RCA), he underwent stenting to RCA in the same sitting. The patient continued dialysis at our centre for two weeks and subsequently lost to follow-up.
Balloon angioplasty with stenting of right brachiocephalic vein and SVC.
Discussion
Superior vena cava syndrome occurs when there is obstruction to the SVC from reasons within or outside the SVC. This obstruction is usually associated with neoplastic conditions such as lung cancer, non-Hodgkin lymphoma, breast cancer, enlarged lymph nodes caused due to metastasis of cancer leading to compression of SVC. Amongst the other causes is a blood clot due to a pacemaker wire or an intravenous catheter. In the present case the left brachiocephalic AVF stopped working but the cause of failure of AVF was not very clear, it could be possibly due to one episode of hypotension during dialysis.
It is observed that 40-45% of cases of SVC obstruction are due to non-malignant causes and out of that 70% cases are on haemodialysis [1]. According to a survey SVC syndrome is seen in around 15,000 patients in United States every year [2]. The process is usually gradual with no clinical manifestations until major obstructions of the SVC occurs due to reasons within or outside the vein. The majority of the cases are secondary to malignancies [3]. But thrombus formations either due to haemodialysis or a pacemaker wire may also cause SVC syndrome.
In haemodialysis (HD) patients there is narrowing of the central vein and higher chances of thrombus formation. The insertion of the HD catheter in the lumen of SVC is known to cause thrombosis, SVC syndrome, bacteraemia and embolus formation. The patients with arteriovenous grafts or fistulas have 29% higher chances of stenosis of central vein [4]. The exact mechanism of thrombus formation is not clear. But the flow across the fistula is turbulent causing injury to the endothelial structure which might release factors responsible for thrombus formation in future [5].
The clinical presentation of SVC syndrome depends on the degree of obstruction of the SVC and the progress of the causative mechanism [6]. The onset is usually gradual with complaints of swelling of face, neck, hands; dyspnoea with non-productive cough. The patient might also complaint of dysphasia, chest pain, and head heaviness [6]. Later on, the condition might end up in respiratory distress with complaints of orthopnoea, syncope which might be life threatening [6].
Even the index patient complained of dyspnoea, swelling of face, engorged neck veins suggestive of SVC syndrome but it did not improve to IV heparin and the condition progressed to worsening the case. As the condition progresses the gradual onset symptoms might end up being life threatening for the patient. The gradual pathogenesis gives enough time for the collateral vessels such as mediastinal, oesophageal and cutaneous varices to form which bypass the SVC occlusion. Thus, 30% of patients with SVC obstruction show oesophageal varices and out of which 60% are on HD for End Stage Renal Disease (ESRD) [7]. The SVC syndrome can be diagnosed clinically but Computed Tomography (CT) and venography tests are used to confirm the diagnosis.
The chances of complications due to HD catheter are more than other types of central venous catheter. Several factors are proposed in the formation of thrombus such as recurrent vascular flow, clotting abnormalities, platelet dysfunction [8].
But in this patient the coagulation study revealed no abnormality, making the exact pathogenesis even more difficult. Even the type of catheter makes a difference on the thrombogenicity such as polyvinyl chloride, polyethylene catheters have higher chances of thrombus formation as compared to silicone rubber ones [9]. In the above case a dual lumen polyurethane Permcath was used.
The treatment options depend on the causative mechanism, if SVC syndrome is cancer related, chemotherapy and radiation might help in reducing the size of the tumour so as to reduce the obstruction of the SVC. Whereas, if the cause for SVC syndrome is thrombus, thrombolysis and anticoagulation therapy are the treatment options. Depending on the degree of obstruction, stenting of SVC is done to relieve the compression [10]. According to the American College of Chest Physicians (ACCP), for cases with catheter associated upper limb Deep Vein Thrombosis (DVT), if the catheter is not required it should be removed while catheters that are functional should be in place and patient should be continued on anticoagulation therapy till the catheter is functioning [11]. In this case, no data regarding upper extremity DVT was available.
In a previous case, HD catheter-associated SVC syndrome with pulmonary embolism was successfully managed with anticoagulation and stenting [6]. In this case despite anticoagulation therapy with IV heparin the clinical symptoms worsened requiring immediate imaging which revealed occlusive thrombus formation in the right brachiocephalic vein. For management, percutaneous transluminal balloon angioplasty with stenting of brachiocephalic vein and SVC was done. This restored adequate flow and symptoms subsided.
Conclusion
The SVC syndrome can be a life-threatening consequence of haemodialysis dependent catheter thrombosis. Physicians should carefully monitor the case in order to avoid any risks and to promptly manage the complications that might follow due to SVC syndrome. In such cases intravascular stents are safe and effective mode of treatment.
[1]. Siegel Y, Schallert E, Prevalence and etiology of focal liver opacification in patients with superior vena cava obstructionJ Comput Assist Tomogr 2013 37(5):805-08.10.1097/RCT.0b013e31829950a124045260 [Google Scholar] [CrossRef] [PubMed]
[2]. Higdon ML, Higdon JA, Treatment of oncologic emergenciesAm Fam Physician 2006 74(11):1873-80. [Google Scholar]
[3]. Lepper PM, Ott SR, Hoppe H, Schumann C, Stammberger U, Bugalho A, Superior vena cava syndrome in thoracic malignanciesRespir Care 2011 56(5):653-66.10.4187/respcare.0094721276318 [Google Scholar] [CrossRef] [PubMed]
[4]. Lumsden AB, MacDonald MJ, Isiklar H, Martin LG, Kikeri D, Harker LA, Central venous stenosis in the hemodialysis patient: incidence and efficacy of endovascular treatmentCardiovasc Surg 1997 5(5):504-09.10.1016/S0967-2109(97)00043-4 [Google Scholar] [CrossRef]
[5]. Agarwal AK, Patel BM, Haddad NJ, Central vein stenosis: A nephrologist’s perspectiveSemin Dial 2007 20(1):53-62.10.1111/j.1525-139X.2007.00242.x17244123 [Google Scholar] [CrossRef] [PubMed]
[6]. Molhem A, Sabry A, Bawadekji H, Al Saran K, Superior vena cava syndrome in hemodialysis patientSaudi J Kidney Dis Transpl 2011 22(2):381-86. [Google Scholar]
[7]. Siegel Y, Schallert E, Kuker R, Downhill esophageal varices: A prevalent complication of superior vena cava obstruction from benign and malignant causesJ Comput Assist Tomogr 2015 39(2):149-52.10.1097/RCT.000000000000018325474143 [Google Scholar] [CrossRef] [PubMed]
[8]. Akoglu H, Yilmaz R, Peynircioglu B, Arici M, Kirkpantur A, Cil B, A rare complication of hemodialysis catheters: Superior vena cava syndromeHemodial Int 2007 11(4):385-91.10.1111/j.1542-4758.2007.00205.x17922732 [Google Scholar] [CrossRef] [PubMed]
[9]. Khanna S, Sniderman K, Simons M, Besley M, Uldall R, Superior vena cava stenosis associated with hemodiaysis cathetersAm J Kidney Dis 1993 21(3):278-81.10.1016/S0272-6386(12)80746-3 [Google Scholar] [CrossRef]
[10]. Baltayiannis N, Magoulas D, Anagnostopoulos D, Bolanos N, Sfyridis P, Georgiannakis E, Percutaneous stent placement in malignant cases of superior vena cava syndromeJ BUON 2005 10(3):377-80. [Google Scholar]
[11]. Kearon C, Akl EA, Comerota AJ, Prandoni P, Bounameaux H, Goldhaber SZ, Antithrombotic therapy for VTE disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice GuidelinesChest 2012 141(2 Suppl):e419S-e496S.10.1378/chest.11-230122315268 [Google Scholar] [CrossRef] [PubMed]