Correspondence: Curious Case of Myocardial Infarction Caused by Lung Abscess- From the Viewpoint of Type 2 Myocardial Infarction by Chest Trauma
Takahiko Nagamine1
1 Department of Emergency Medicine, Sunlight Brain Research Center, Hofu, Yamaguchi, Japan.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Takahiko Nagamine, 4-13-18 Jiyugaoka, Hofu, Yamaguchi, Japan.
E-mail: tnagamine@outlook.com
Dear Editor,
I read with great interest the article by Bajpai J et al., reporting a patient of Myocardial Infarction (MI) caused by lung abscess [1]. They exhibited a curious case of acute MI without obvious atherosclerosis of coronary arteries. Acute MI most commonly occurs due to the occlusion of coronary arteries by an atherosclerotic plaque, but there are other mechanisms for its occurrence. An imbalance between demand and supply of oxygen in the myocardium due to coronary microembolism is another important mechanism of MI [2]. I recently experienced an acute MI patient after rib fracture who did not had obvious atherosclerotic obstruction of coronary arteries.
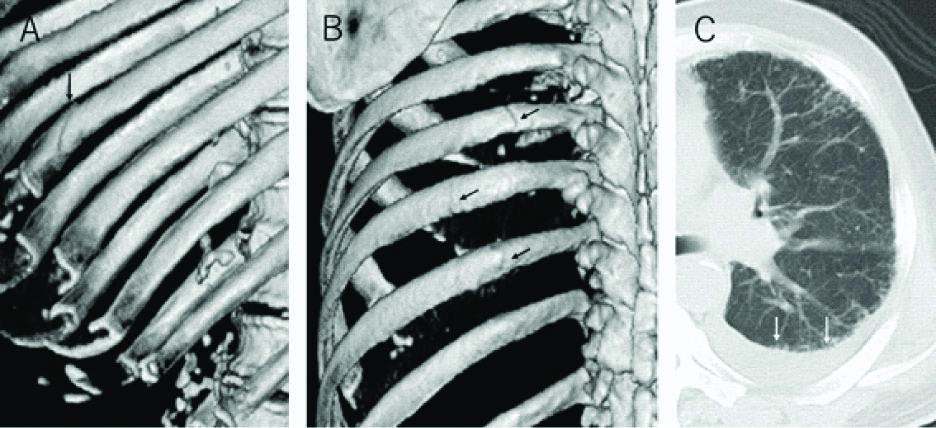
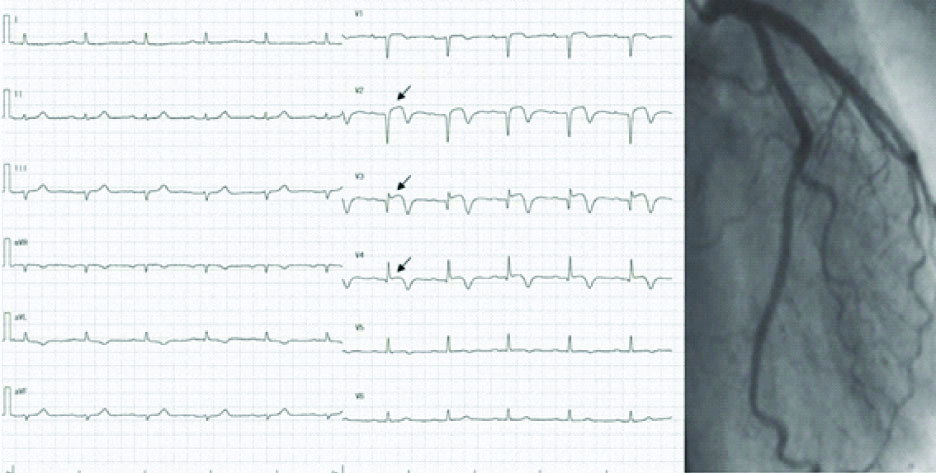
A 76-year-old man presented to the emergency room in the hospital following a fall from a ladder. The patient presented with dull pain on the left chest wall which exacerbated with deep breath and movement. He denied chest pain prior to falling. Computed tomography of the chest revealed left rib fracture and small pleural effusion indicating haemothorax [Table/Fig-1]. He was admitted to the hospital to receive conservative therapy for rib fracture and haemothorax. However, he continued to have chest pain that changed in character to crushing in nature with significant shortness of breath a few hours after admission. Twelve-lead ECG was performed and showed ST segment elevation in the anterior leads. However, left coronary angiography revealed no occlusion [Table/Fig-2]. Troponin-T test turned out to be positive 12 hours after admission. The patient was diagnosed as having Type 2 MI after rib fracture.
Chest CT revealed undisplaced fracture of the eighth, ninth, and tenth ribs (black allows) and small amount of pleural effusion indicative of haemothorax (white allows).
Twelve lead ECG after admission revealed ST segment elevation in the anterior leads (lead V2–V4; black allows). However, left coronary angiogram demonstrating normal coronary arteries.
Type 2 MI denotes myocardial necrosis without obvious coronary artery disease. The main causes were anaemia, followed by sepsis, arrhythmia and postoperation [3]. Both lung abscess in Bajpai J’s report and minor thoracic injury in the index case are rare causes of Type 2 MI, but clinicians need to know the possibility of this rare condition.
A similar mechanism between lung abscess and thoracic injury seems to be microembolism of coronary arteries, resulting in an imbalance between demand and supply of oxygen in the myocardium. However, in this patient, left coronary angiography revealed no occlusion, indicative of Myocardial Infarction with Normal Coronary Arteries (MINOCA) which was probably precipitated by rib fracture. While the eventual etiology remains uncertain in most MINOCA patients, chest trauma might cause cardiac contusion, resulting in ruptured plaque, plaque erosion, and thrombus. Concerning treatment, the use of antiplatelet and anti-thrombotic agents may give rise to serious troubles such as haemoptysis in Bajpai J’s case.
Thus, the patient under anticoagulation therapy should be carefully monitored to avoid fatal bleeding. In case of moderate bleeding, antiplatelet and antithrombotic regimen should be stopped even though putting the patient at higher risk of ischemic events. Use of anti-ischemic therapy enhances the risk of bleeding, while interrupting them to minimise bleeding predisposes to risk of thrombotic events. Primary diseases including pulmonary abscess or thoracic injury present therapeutic challenges in management of Type 2 MI. Fortunately, the index patient was successfully treated with clopidogrel and aspirin without exacerbating haemothorax.
In conclusion, thoracic injury may be one of the causes of Type 2 MI same as pulmonary abscess in Bajpai J’s report. Twelve-lead ECG has to be performed routinely on all patients with chest trauma.
Author Declaration:
Financial or Other Competing Interests: NA
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 02, 2019
Manual Googling: Nov 29, 2019
iThenticate Software: Dec 03, 2019 (11%)
[1]. Bajpai J, Vishwakarma P, Pradhan A, Kant S, Jain A, Curious case of myocardial infarction caused by lung abscessJ Clin Diagn Res 2019 13(1):OD01-03. [Google Scholar]
[2]. Saaby L, Poulsen TS, Hosbond S, Larsen TB, Pyndt Diederichsen AC, Hallas J, Classification of myocardial infarction: frequency and features of type 2 myocardial infarctionAm J Med 2013 126(9):789-97.10.1016/j.amjmed.2013.02.02923856021 [Google Scholar] [CrossRef] [PubMed]
[3]. Stein GY, Herscovici G, Korenfeld R, Matetzky S, Gottlieb S, Alon D, Type 2 myocardial infarction-patient characteristics, management and outcomesPLoS One 2014 9(1):e8428510.1371/journal.pone.008428524392121 [Google Scholar] [CrossRef] [PubMed]