Delirium, which is an acute condition with fluctuating course, is characterised by disturbances in attention combined with either a change in level of consciousness or disorganised thinking. The aetiology of delirium is multi-factorial and it may be surgery, admission to intensive care unit, primary neurological disorder, psychoactive drug, etc., [1,2]. Post-operative delirium is common in elderly age group and incidence of post-operative delirium ranges from 10% to 61% in elderly age group [3]. The recognition and treatment of post-operative delirium are important because it leads to increased duration of hospital stay and mortality [4].
Melatonin (N-acetal-5-methoxy-traptamine) is a hormone formed from Tryptophan, secreted by pineal gland and it plays an important role in the regulation of sleep wake sleep cycle [5]. A strong correlation has been seen between post-operative delirium and changes in melatonin secretion [6]. Synthetic melatonin supplements when used as premedication found to improve post-operative cognitive profile [7].
Ramelteon, a melatonin agonist was approved by US Food and drug administration for treatment of insomnia and has been suggested for prevention of delirium [8]. Ramelteon is a tricyclic synthetic analog of melatonin with chemical name (S)-N-[2-(1,6,7,8-tetrahydro-2H-indeno{5,4-b}furan-8-71) ethyl] propionamide [9,10]. Ramelteon has more affinity for melatonin receptor MT1 and MT2 compared with melatonin [11,12]. The reason for this is the unique molecular structure of Ramelteon i.e., a propionyl group instead of acetyl group, two hydrocarbon atoms in a furan ring instead of a methoxy group and its lack of nitrogen in 5-atom ring, causing more tissue distribution than melatonin. The effectiveness of Ramelteon has attributed to its higher penetration and half-life of 1-2 hours in comparison to melatonin whose half-life is approximately 30 minutes [13]. Also, one of the Ramelteon’s metabolites MTII have functional half-life of 5 hours thus making Ramelteon superior to melatonin [8]. Consequently, Ramelteon also desensitises MT1 and MT2 receptors more than melatonin itself [14].
To the best of authors’ knowledge, very few studies have been done to assess the role of Ramelteon in prevention of post-operative delirium in elderly patient [15,16]. So this study was done to evaluate the role of Ramelteon in prevention of post-operative delirium in elderly patient.
The primary objective of this study was to compare incidence of post-operative delirium in elderly patients using the CAM between Ramelteon and control group. The secondary objective was to compare the intraoperative haemodynamics, Ramsay Sedation Score (RSS), post-operative Ramsay sedation Score and any complications between ramethe twolteon and control group.
Materials and Methods
This randomised double-blind study was carried out at the Department of Anaesthesiology, King George Medical University, Lucknow, Uttar Pradesh. After approval by the Institutional Ethics Committee (89th ECM II B Thesis/P14), patients age more than 65 years, admitted to Gandhi Memorial and Associate Hospitals, King George’s Medical University, Lucknow, undergoing surgery at various surgical departments were recruited for this study.
Patients belonging to the American society of Anesthesiologists (ASA) physical status Grade 1 and 2 and planned for surgery requiring neuraxial anaesthesia for duration longer than one hour were included. Patients with history of dementia, severe infections, intracranial bleed, having any acute cardiac event and taking any psychiatric medications were excluded from the study. Hundred patients were randomly distributed in two groups with each group containing 50. It was calculated to be 50 in each group on the basis of sensitive and specification of CAM [17] using the formula:
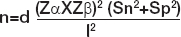
where Sn=0.8 sensitive; Sp=0.959 specificity CAM; d=2, effect for multiple assessment parameters; Type I error α=5%; Type II error β=20% for 80% power of study.
Randomisation was done according to a computer-generated list. Group I (Ramelteon group): Received oral ramelteon; one tablet of ramelteon (8 mg) 12 hours before surgery and 1 tablet of ramelteon (8 mg) 1 hour before surgery.
Group II (Control group): Received placebo tablets; one tablet 12 hours before surgery and 1 tablet 1 hour before surgery [Table/Fig-1].
After obtaining written informed consent from patients, the complete medical history, physical examination and mini-mental examination were done for all patients [Table/Fig-2]. Study drug was given in a sealed envelope to all patients by the anaesthetist who was not involved in the observation of the patients and asked to take 1st dose 12 hours before surgery and 2nd dose 1 hour before surgery. It was a double-blind study as observer was not involved in giving the study drug to patients and patients were also not aware which study drug was given to them. No sedative drug was given to the patient preoperatively. After arrival in an operation theatre, standard monitors were attached which include pulse oximeter (SpO2), ECG, non-invasive blood pressure monitoring. All these parameters were recorded and monitoring continued throughout intraoperatively. On arrival in operation theatre, patients Ramsay sedation score was noted and thereafter every hour till completion of surgery. All patients were given combined spinal and epidural anaesthesia. On the 1st day of surgery, epidural infusion was used for post-operative analgesia. On 2nd day and 3rd day, Inj. Paracetamol 1 gm IV 6 hourly was used for post-operative analgesia.
Mini-mental state examination (MMSE).
| Instructions: Ask the questions in the order listed. Score one point for each correct response within each question or activity. |
|---|
| Maximum score | Patient’s score | Questions |
|---|
| 5 | | “What is the year? Season? Date? Day of the week? Month?” |
| 5 | | Where are we now: State? Country? Town/city? Hospital? Floor?” |
| 3 | | The examiner names three unrelated objects clearly and slowly, then asks the patient to name all three of them. The patient’s response is used for scoring. The examiner repeats them until patient learns all of them, if possible. Number of trials: ___________ |
| 5 | | “I would like you to count backward from 100 by sevens.” (93, 86, 79, 72, 65, …) Stop after five answers. Alternative: “Spell WORLD backwards.” (D-L-R-O-W) |
| 3 | | “Earlier I told you the names of three things. Can you tell me what those were?” |
| 2 | | Show the patient two simple objects, such as a wristwatch and a pencil, and ask the patient to name them. |
| 1 | | “Repeat the phrase: ‘No ifs, ands, or buts.’” |
| 3 | | Take the paper in your right hand, fold it in half, and put it on the floor.” (The examiner gives the patient a piece of blank paper.) |
| 1 | | “Please read this and do what it says.” (Written instruction is “Close your eyes.”) |
| 1 | | “Make up and write a sentence about anything.” (This sentence must contain a noun and a verb.) |
| 1 | | “Please copy this picture.” (The examiner gives the patient a blank piece of paper and asks him/her to draw the symbol below. All 10 angles must be present and two must intersect.) |
| 30 | | Total |
| Interpretation of the MMSE |
| Method | Score | Interpretation |
| Single cut-off | <24 | Abnormal |
| Range | <21 | Increased odds of dementia |
| >25 | Decreased odds of dementia |
| Education | 21 | Abnormal for 8th grade education |
| <23 | Abnormal for high school education |
| <24 | Abnormal for college education |
| Severity | 24-30 | No cognitive impairment |
| 18-23 | Mild cognitive impairment |
| 0-17 | Severe cognitive impairment |
Delirium was assessed by CAM on 1st, 2nd and 3rd day [Table/Fig-3]. Intraoperative Ramsay sedation score [Table/Fig-4] was observed. Intraoperative haemodynamic (BP, Heart Rate, SpO2) were recorded at baseline to 30 minutes at every 5 minutes and subsequently every 15 minutes. Post-operative Ramsay sedation score was observed immediately after surgery, after 6 and 24 hours.
Confusion Assessment Method (CAM).
| The diagnosis of delirium by CAM requires the presence of both features A and B |
|---|
| A. Acute onset and fluctuating course | Is there evidence of an acute change in mental status from patient baseline? Does the abnormal behavior:come and go? fluctuate during the day? increase/decrease in severity?
|
| B. Inattention | Does the patient:have difficulty focusing attention? become easily distracted? have difficulty keeping track of what is said?
|
| And the presence of either feature C or D |
| C. Disorganised thinking | Is the patient’s thinkingDisorganised Incoherent For example does the patient have rambling speech/irrelevant conversation? unpredictable switching of subjects? unclear or illogical flow of ideas?
|
| D. Altered level of consciousness | Overall, what is the patient’s level of consciousness:alert (normal) vigilant (hyper-alert) lethargic (drowsy but easily roused) stuporous (difficult to rouse) comatose (unrousable)
|
| Ramsay 1 | Anxious, agitated, restless |
| Ramsay 2 | Cooperative, oriented, tranquil |
| Ramsay 3 | Responsive to commands only If asleep |
| Ramsay 4 | Brisk response to light glabellar tap or loud auditory stimulus |
| Ramsay 5 | Sluggish response to light glabellar tap or loud auditory stimulus |
| Ramsay 6 | No response to light glabellar tap or loud auditory stimulus |
Statistical Analysis
All the data for continuous variables (age, disease duration, HR, MAP, SpO2 and MMSE) are shown as the mean±standard deviation and the categorical variable (gender) is shown as a percentage. The total scores on the MMSE were calculated as the sum of single items. The Chi-square test was used to compare the categorical variables between the groups. Unpaired t-test was used to compare the continuous variables between the groups. The SPSS Version 21.0 statistical Analysis Software was used for the statistical analyses. p<0.05 was considered to indicate a statistically significant difference.
Results
The demographic variables such as age, gender, ASA grade and baseline hemodynamic parameters were comparable between Group l and Group ll as shown in [Table/Fig-5]. This study included patients of age between 65-82 years. Mean age of patients was comparable in between group I (69.30±4.05 years) and Group II (70.64±3.76 years) and male preponderance was observed. Pre-operative heart rate, systolic BP and diastolic BP of patients were found to be comparable in both groups (p>0.05).
Between group comparison of demographic variables.
| Group I (n=50) | Group II (n=50) | p-value |
|---|
| Age (years) Mean±SD | 69.30±4.05 | 70.64±3.76 | 0.090# |
| Gender |
| Female | 15 (30.0%) | 17 (34.0%) | 0.668# |
| Male | 35 (70.0%) | 33 (66.0%) | |
| ASA grade |
| Grade I | 31 (62.0%) | 31 (62.0%) | |
| Grade II | 19 (38.0%) | 19 (38.0%) | 1.00# |
| Hemodynamic variables |
| Heart rate | 86.98±12.76 | 83.32±9.00 | 0.101# |
| Systolic BP | 132.38±11.90 | 131.78±7.38 | 0.763# |
| Diastolic BP | 77.54±9.17 | 79.30±6.36 | 0.267# |
Data are represented as mean±SD, n (%) and ratio. SD=Standard deviation
#p-value not significant; *p-value significant
At the time of enrolment none of the patients in the study was found to be suffering from dementia, severe infection, intracranial events, MI, CHF, arrhythmias, COPD or Pulmonary embolism. Associated illness in the population was higher in Group II as compared to group I for prevalence of hypertension (22.0% vs. 20.0%) and diabetes (18.0% vs. 16.0%) but these differences were not found to be statistically significant. Whereas prevalence of Asthma was higher in group I as compared to Group II (6.0% vs. 4.0%) but this difference was also not found to be statistically significant.
Mental status of the patients was assessed using Mini-Mental Status examination. MMSE score was found to be higher in group I (27.22±1.33) as compared to that of Group II (27.19±1.82) but this difference was not statistically significant.
Patients were admitted for surgical intervention of different ailments and were admitted in the respective speciality wards. Among patients of Group I admissions to Urology wards were most common followed by Orthopedics while among patients of Group II admissions to Urology and Orthopedics wards were most common. Proportional difference in patients of above two groups admitted to different speciality wards was not found to be statistically significant (p=0.474).
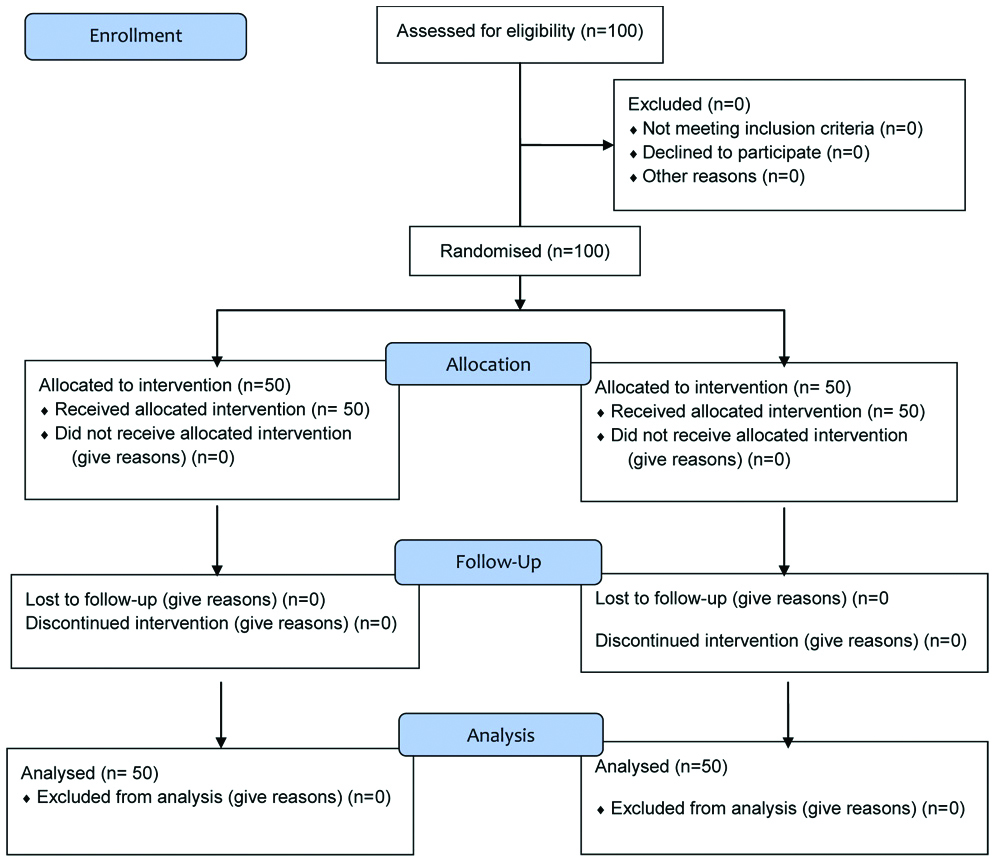
Mean Heart rate of patients of Group I was found to be higher as compared to that of Group II except at 25 minutes and 150 minutes. Difference in mean heart rate of patients of above two groups was not found to be statistically significant at any of the periods of observation [Table/Fig-6].
Comparison of heart rate (Beats/minute).
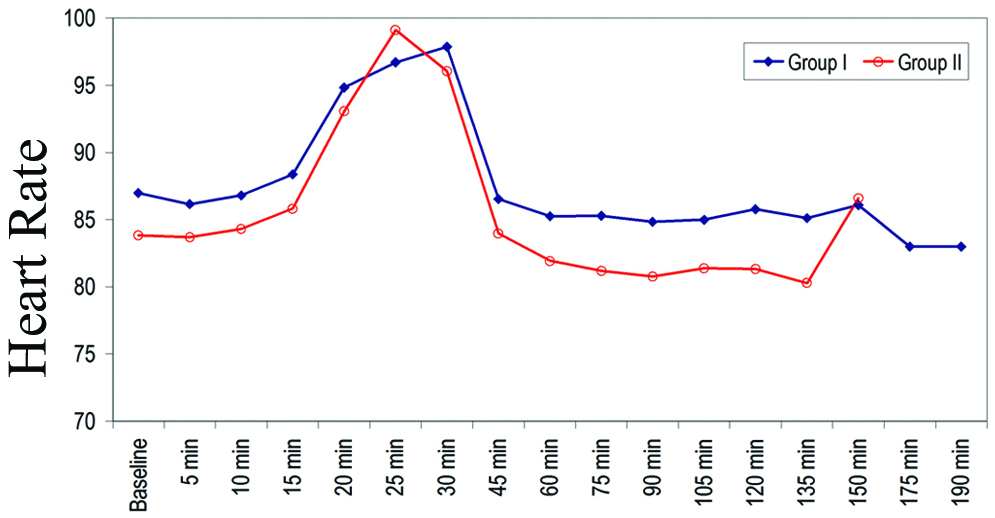
Systolic BP of patients of group I was found to be higher as compared to that of Group II at baseline, 5 minutes, 20 minutes, 25 minutes, 30 minutes while at rest of the periods of observation, SBP of Group II was higher as compared to that of group I, but difference in mean systolic BP of patients of two groups was found to be statistically significant only at 25 minutes (119.46±11.68 vs. 111.92±5.15 mmHg) [Table/Fig-7].
Comparison of Systolic Blood Pressure (mm of Hg).
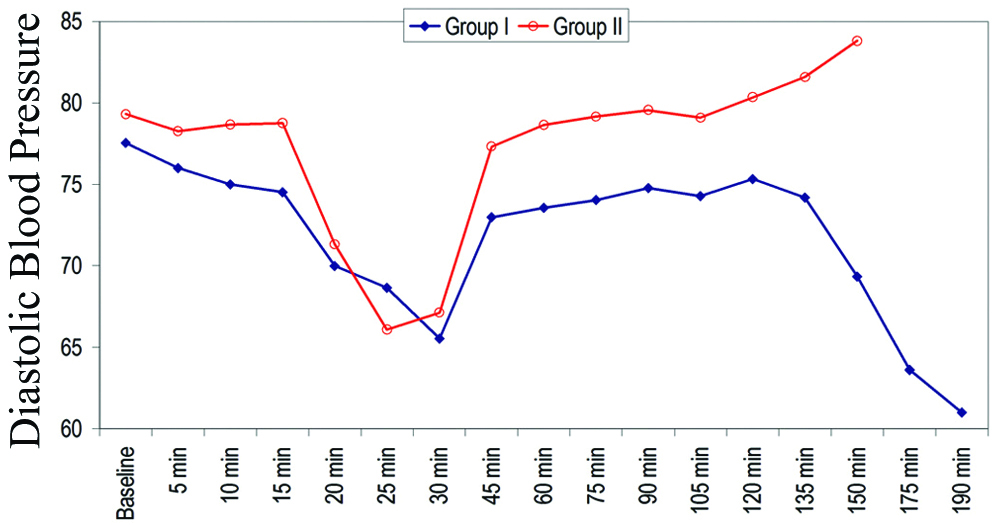
Mean Diastolic BP of patients of Group II was found to be higher as compared to that of Group I at all the periods of observation except at 25 minutes, and differences in mean diastolic BP of patients of above two groups was found to be statistically significant at all the periods of observation except at baseline, 5 minutes, 20 minutes and 30 minutes [Table/Fig-8].
Comparison of Diastolic Blood Pressure (mm of Hg).
Oxygen saturation level of all the patients during the period of observation was maintained above 95% hence this difference has no clinical relevance.
Sedation score of all the patients just before surgery was 2.00. Mean sedation score of patients of group I (2.32±0.62) was found to be higher as compared to that Group II (2.08±0.63). Difference in Ramsay sedation score of patients of above two groups was not found to be statistically significant at any of the period of observation [Table/Fig-9].
Ramsay Sedation Score at different time intervals.
| Time interval | Group I (Mean±SD) | Group II (Mean±SD) | Mann Whitney U test |
|---|
| ‘Z’ | ‘p’ |
|---|
| 0 h | 2.00±0.00 | 2.00±0.00 | 0.000 | 1.000# |
| 1 h | 2.32±0.62 | 2.08±0.63 | 1.893 | 0.058# |
| 2 h | 2.32±0.62 | 2.08±0.63 | 1.893 | 0.058# |
| 3 h | 2.09±0.54 | - | - | - |
| Immediate post-surgery | 2.32±0.62 | 2.08±0.63 | 1.893 | 0.058# |
| 6 h post-operative | 2.32±0.62 | 2.08±0.63 | 1.893 | 0.058# |
| 24 h post-operative | 2.32±0.62 | 2.08±0.63 | 1.893 | 0.058# |
#p-value not significant; *p-value significant
Confusion assessment method was used to assess the post-operative delirium on follow-up at Day 1, Day 2 and Day 3. Total incidence of delirium was 8%; lower in group I as compared to Group II (4% vs 12%). On day 2, one patient developed delirium in group I while 3 patients developed delirium in Group II but difference was not found to be statistically significant. On day 3, one patient developed delirium in group I and 3 patients in Group II but difference was not statically significant. None of the patients, irrespective of any of the groups was positive for CAM on follow-up at Day 1 [Table/Fig-10].
Comparison of positive CAM on follow-up.
| Day of follow-up | Group I (n=50) | Group II (n=50) | p-value |
|---|
| Day 1 | 0 (0.0%) | 0 (0.0%) | - |
| Day 2 | 1 (2.0%) | 3 (6.0%) | 0.307# |
| Day 3 | 1 (2.0%) | 3 (6.0%) | 0.307# |
#p-value not significant; *p-value significant
Discussion
Post-operative delirium is one of post-operative neurological complication, which is seen, in elderly patients who are of age more than 65 years. This leads to prolonged hospital stay and an increasing need for rehabilitation and home care. So, this study was conducted to evaluate the effect of Ramelteon on post-operative delirium as primary objective and its effect on haemodynamic responses and sedation scores in elderly patients as secondary objectives.
Demographic variables were compared between two groups. The aetiology of post-operative is multifactorial and some of the predisposing factors are like pulmonary disease, pre-operative cognitive dysfunction, patient on antiarrhythmic and use of opioids [18,19]. These factors were comparable between two groups in this study. Post-operative delirium was determined using CAM on day 1,2,3. CAM has more than 90% sensitivity and specificity in elderly patients [20,21]. Wei LA et al., found CAM scale to be a reliable tool to evaluate post-operative delirium if used by trained personnel [22].
In this study, it was observed that the incidence of delirium in Ramelteon group was lower in comparison with placebo group but it was not statistically significant; similar to other studies that reported that Ramelteon prolongs the time to development of delirium and decreases the frequency of delirium [12,16]. Hatta K et al., did a multicenter randomised placebo-control trial in ICU and observed that there was decrease in delirium after Ramelteon administration (3% vs 32%, p=0.003) [12]. Miyata R et al., did a retrospective analysis of patients of age 70 years or more undergoing anatomical pulmonary resection for lung cancer and observed that incidence of delirium was lower in the Ramelteon group in comparison to control group (p=0.061) [15]. Similarly, Booka E et al., studied 65 patients who underwent pharyngo-larygectomy with oesophagectomy and observed that Ramelteon was associated with significantly decreased incidence of delirium in post-operative period [16].
In this study, post-operative delirium developed on day second and day third. Whitlock EL et al., also observed that post-operative delirium usually peaks between first and third day [19]. The total incidence of delirium in this study was 8% which is lesser than previously reported studies [15,16]. The difference may be due to inclusion of patients undergoing surgery only under regional anaesthesia. Although perioperative anaesthesia can affect the development of post-operative delirium, all patients in this study received similar perioperative anaesthesia technique and analgesic administration under the same perioperative anaesthetic policy.
Intra-operatively, the haemodynamic variable such as heart rate was comparable in both Ramelteon and placebo groups but there were more changes in placebo group. These findings are supported by other studies, that reported that from the baseline values, the change in heart rate between the study groups were found to be non-significant at any given time interval [23,24]. Although no significant decrease in MAP was noted in the Ramelteon group but melatonin was found to have a mild hypotensive effect due to the direct action on vascular melatonin receptors and the reduction of the adrenergic outflow and catecholamine levels [25]. This property of melatonin was utilised in eye surgeries where 10 mg melatonin given orally 90 minutes before the operation in cataract surgery patients provided significant sedation and lowering of intraocular pressure [26]. In the present study, the overall mean arterial pressures were found to be on higher side in Ramelteon as compared to placebo groups although it was not statistically significant. The difference in SpO2 was not found to be statistically significant among different study groups at any given time intervals. Throughout the intraoperative period, the SpO2 was maintained at 96-100% with no episode of fall in saturation at any point of time.
The difference in Ramsay sedation score of patients of the two groups was not statistically significant at any of the period of observation. Patients in the Ramelteon group had higher sedation scores as compared to placebo group but none had respiratory depression. Mallick S et al., compared the effect of Ramelteon and placebo on perioperative sedation in cases of laparoscopic cholecystectomies and they also reported that the sedation score was significantly higher in Ramelteon groups compared to the placebo group after 30 minutes and 60 minutes of administration of drug [27]. Borazan H et al., and Naguib M et al., also reported that the sedation score was markedly higher in the melatonin group than in control group [28,29]. Various studies suggested that the Ramelteon increased sedation effects in a dose-independent manner [30-32].
Limitation
The main limitation of this study is that it is a single-centre study. Also, all surgical specialties were included, which could have effected the total incidence of delirium so studies focusing on single speciality patients are required.
Conclusion
Ramelteon decreases the incidence of post-operative delirium with higher sedation scores. So Ramelteon can be recommended in patients having high risk of developing post-operative delirium. The scope of further research on Ramelteon includes the use of Ramelteon in higher doses and post-operative continuation of Ramelteon, and its effects on the delirium, sedative effects and hemodynamic variables can be studied.
Data are represented as mean±SD, n (%) and ratio. SD=Standard deviation
#p-value not significant; *p-value significant
#p-value not significant; *p-value significant
#p-value not significant; *p-value significant