Bilateral Intralobar Pulmonary Sequestration in an Elderly Patient
Askin Gülsen1, Berat Uslu2
1 Respiratory Physician, Department of Pneumology, University of Lübeck, Lübeck, Schleswig-Holstein, Germany.
2 Respiratory Physician, Department of Pneumology, Yedikule Chest Diseases and Thoracic Surgery Training and Research Hospital, Istanbul, Turkey.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Askin Gülsen, Department of Pneumology, University of Lübeck, Ratzeburger Allee 160 (Haus 40), 23538, Lübeck, Schleswig-Holstein, Germany.
E-mail: askingulsen@hotmail.com
Pulmonary Sequestrations (PS) are congenital anomalies resulting from defective pulmonary development. PS consist of abnormal lung tissue that is not associated with the normal airway. They have their own abnormal vascular system consisting of arterial connections (usually from the aorta and its branches) and venous drainage through pulmonary venules. These lung lesions do not contribute to the exchange of oxygen and carbon dioxide. However, intralobar PS is usually seen in childhood, unilaterally in the left lower lobe of the lung. PS is rarely encountered bilaterally or in older patients. Herein, we describe a case of bilateral PS detected by computed tomography angiography in an elderly patient. The patient refused additional interventional examination and operation, so clinical follow-up was continued.
Asymptomatic, Drycough, Lung
Case Report
A 64-year-old female patient was admitted to the university hospital chest disease clinic due to chest pain, following one month history of persistent dry cough and a flu infection. The patient had no chronic complaints other than a dry cough. Otherwise, the patient’s history was not noteworthy. She had no known lung disease, no complaints of chronic cough or sputum production, and no recurrent pulmonary infections.
A physical examination revealed a blood pressure of 130/90 mm Hg; pulse rate: 68 beats/min; respiratory rate: 15 breaths/min; and body temperature: 38°C. On respiratory system examination, the breath sounds were reduced in the lungs in bilateral lower lobes. Complete blood count showed a white blood cell count of 12.500 103 cells/mm3, a C-reactive protein level of 5.4 mg/dL, and D-dimer level of 550 μg/L.
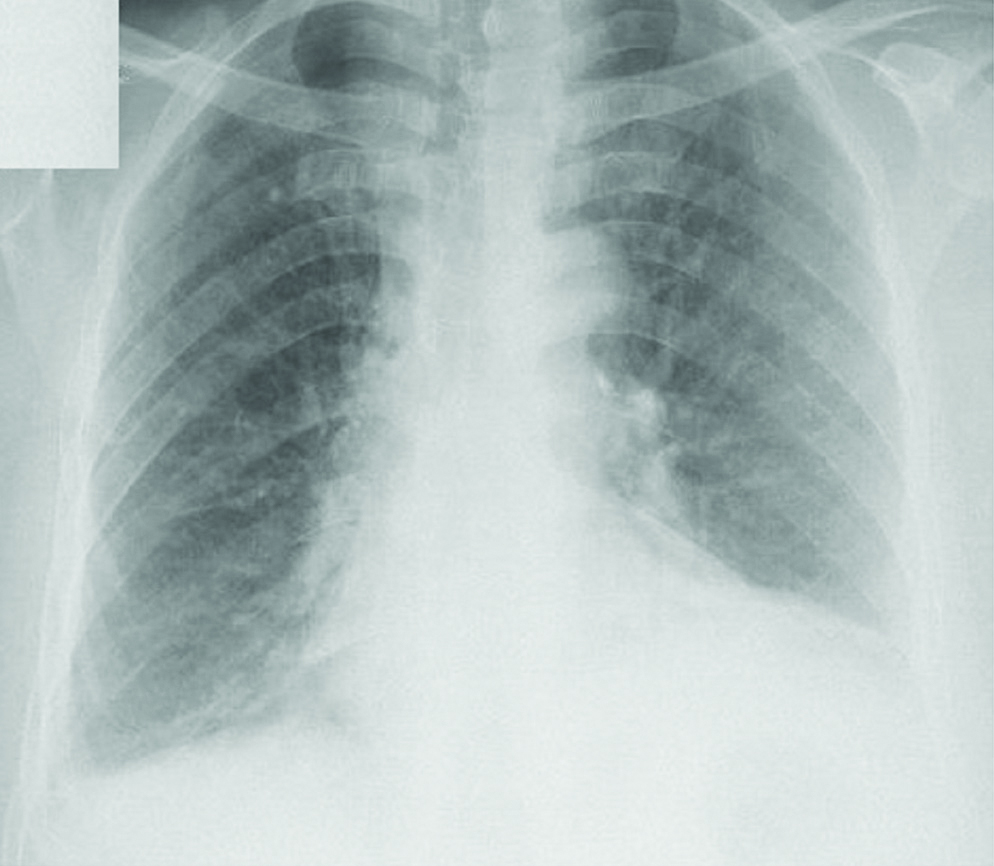
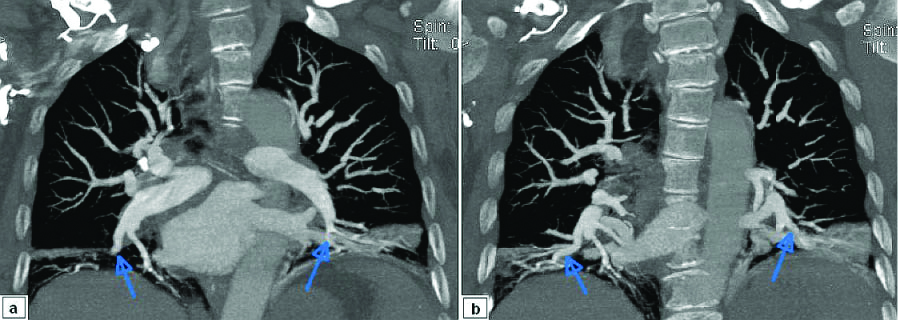
Chest radiograph showed right sinus blunting, increased cardiothoracic ratio, and possible left lower lobe consolidation [Table/Fig-1]. Chest Computed Tomography Angiography (CTA) scan was performed to rule out pulmonary embolism. CTA revealed a bilateral aberrant lung tissue with left and right abnormal systemic arterial supply separated from celiac truncus, and a venous vessels flowing into both lower pulmonary veins [Table/Fig-2a,b]. There was no sign of pulmonary embolism. The lesions in the CTA scan were compatible with bilateral PS. Echocardiographic evaluation showed no abnormal findings.
Chest radiograph showing right sinus blunting, increased cardiothoracic ratio, and possible left lower lobe consolidation.
CT-Angiography showing bilateral aberrant lung tissue with left and right abnormal systemic arterial supply separated from celiac truncus, and a venous vessels flowing into both lower pulmonary veins.
Antibiotic treatment was started because of increased inflammation parameters and mild fever. Cough and chest pain regressed slowly within four weeks. Surgical treatment for bilateral intralobar PS was recommended, but she refused additional interventional examination and operation, so clinical and radiological follow-up was continued.
Discussion
Patients with Pulmonary Sequestration (PS) may present to the clinics with no symptoms, unknown fever, haemoptysis, pulmonary infections, dry cough, dyspnea or progressive respiratory distress [1]. Along with these symptoms, chest radiographic pattern of the patients are usually unilateral nonhomogeneous parenchymal consolidation in the lower lobe [2]. This congenital anomaly results in a non-functional area of the lung following a deterioration in embryogenesis. They have their own abnormal vascular systems (often, arterial feeding through aorta, and venous drainage through pulmonary venules) and are not connected to the bronchial system [Table/Fig-3] [3]. These lung lesions do not contribute to the exchange of oxygen and carbon dioxide [4]. In 1946, Pryce and colleagues used the terms “extralobar” and “intralobar” PS for the first time [5]. PS is more commonly intralobar (75%) than extralobar (25%) [6]. Intralobar PS is usually seen in childhood, unilaterally in the left lower lobe of the lung [7].
Characteristic features of pulmonary sequestration.
| Extralobar | Intralobar |
|---|
| Anatomy | Within lung parenchyma | Separate from lung |
| Localisation | Within basal segments | Below lower lobe |
| Predominant side | Left | Left |
| Age | 60% <1 yr of age | 50% adults; Rare <2 yr of age |
| Male /Female | 4:1 | 1:1 |
| Artery | Systemic | Systemic |
| Vein | Systemic (azygous) | Central (pulmonary vein) |
| Associated anomalies | Frequent (diaphragmatic hernia) | Rare |
| Origin | Congenital | Congenital or acquired |
Quoted from Nicolette LA, et al., [3] with permission
PS is a rare congenital anomaly that accounts for 0.1% to 6.4% of all pulmonary malformations, and rarely encountered bilaterally or in older patients [8]. Wei Y et al., completed the most extensive work on this subject in 2011 [9]. As a result of the analysis of 2625 PS patients, it was reported that only three of them had bilateral PS and two had intralobar PS. In a review of 540 patients by Savic B et al., only two of the patients had bilateral, intralobar PS [8]. Therefore, the index patient is very rare because of the presence of bilateral PS and asymptomatic clinically and he was over 50 years of age. Approximately, half of PS patients are diagnosed before the age of 20 with the first symptom appearing before the age of 10 years in 37.2% of cases [8,10]. PS may lead to various chronic symptoms or may be asymptomatic. It causes complaints such as cough, fever, frequent sputum production, and very rarely chest pain [9]. It is often an incidental finding during chest radiography in patients with frequent, recurrent, or incurable lung infections. Recurrent respiratory tract infections are the most common reason for referral to clinics. In addition, 13.3-15.5% of the cases are reported to be asymptomatic and incidentally diagnosed. This patient was referred because of a persistent dry cough and a new onset chest pain that did not resolve after the flu-infection.
In a recent study, the most common symptoms in patients was cough and sputum (82.6%) [11]. In addition, intermittent fever, chest pain and haemoptysis have also been reported, 17.4%, 13.0% and 4.0%, respectively. The mean age of the patients was 48.3 years, 17.4% were asymptomatic and the diagnosis was made incidentally. CT findings were reported as solid (69.5%), mixed cystic-solid (30.4%) and cystic (4.3%) [11].
Chest CTA examination often reveal mass lesions, cystic lesions, cavitary and pneumonic lesions (49.0%, 28.5%, 11.5% and 7.9%, respectively) [9]. The differential diagnosis of PS are: lung cancer, lung abscess, empyema, congenital cystic malformation, diaphragmatic hernia, bronchiectasis and pneumonia [12]. Multidetector-row CTA is the most commonly used diagnostic test, and surgical procedures including video-assisted thoracoscopic surgery are recommended in symptomatic cases.
However, the surgeries can be performed by thoracotomy or thoracoscopic approach. Lobectomy can generally be performed as sub-lobar resection, segmentectomy or atypical resections [13]. Evaluation of the artery, feeding the PS segment is very important in patients planned for resection. In addition, pre-operative embolization may be required in patients with hemoptysis and artery fed from the abdominal aorta [1]. Coil embolization may be used as an alternative to surgery in patients with intralobar PS [14]. [Table/Fig-4] shows an overview of previous studies [1,8,9,11,15].
Overview of previous published studies [1,8,9,11,15].
| Author | Year | n | IL % | EL % | IL+EL % | Bilateral % | Age | Asymp. % |
|---|
| Schlöricke E et al., [1] | 2016 | 14 | 79.0 | 21.0 | - | - | mean 50 y | 21.4 |
| Savic B et al., [8] | 1979 | 540 | 74.0 | 24.6 | 1.1. | 0.3 | <20-%50 | 15.5 |
| Wei Y et al., [9] | 2011 | 2625 | 83.9 | 16.0 | - | 0.1 | - | 13.3 |
| Dong Q et al., [11] | 2019 | 23 | 100 | - | - | - | mean 48.3 y | 17.3 |
| Alsunraim M et al., [15] | 2018 | 32 | 81.0 | 19.0 | - | - | mean 42 y | 40.0 |
n: Patients; y: Years; IL: Intralobar; EL: Extralobar; Asypm: Asymptomatic
Conclusion
PS is rarely seen in a patient over 60 years of age, but is diagnosed incidentally in symptomatic cases. Present patient is one of the very few cases in the literature due to bilateral, asymptomatic and elderly presentation. We would like to emphasise the need to consider PS as well as other possible causes, in the light of differential diagnoses such as pneumonia, pleural effusion and embolism.
Quoted from Nicolette LA, et al., [
3] with permission
n: Patients; y: Years; IL: Intralobar; EL: Extralobar; Asypm: Asymptomatic
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 08, 2019
Manual Googling: Nov 19, 2019
iThenticate Software: Nov 28, 2019 (10%)
[1]. Schlöricke E, Hoffmann M, Kujath P, Facklam J, Henning M, Wissgott C, Management of the therapy of pulmonary sequestration: A retrospective multicentre studyZentralbl Chir 2016 141:50-57.10.1055/s-0036-1587455 [Google Scholar] [CrossRef]
[2]. Giannotta M, Leone MB, Greco L, Baldazzi M, Zompatori M, Intralobar pulmonary sequestration with bronchial atresia and a systemic artery feeding a normal contralateral lungBJR Case Rep 2015 2(1):20150176 [Google Scholar]
[3]. Nicolette LA, Kosloske AM, Bartow SA, Murphy S, Intralobar pulmonary sequestration: A clinical and pathological spectrumJ Pediatr Surg 1993 28(6):802-05.10.1016/0022-3468(93)90331-E [Google Scholar] [CrossRef]
[4]. Stocker JT, Malczak HT, A study of pulmonary ligament arteries: Relationship to intralobar pulmonary sequestrationChest 1984 86(4):611-15.10.1378/chest.86.4.6116478904 [Google Scholar] [CrossRef] [PubMed]
[5]. Pryce DM, Lower acessory pulmonary artery with intralobar sequestration of lung: A report of seven casesJ Pathol Bacteriol 1946 58(3):457-67.10.1002/path.170058031620283082 [Google Scholar] [CrossRef] [PubMed]
[6]. Gonzalez D, Garcia J, Fieira E, Paradela M, Video-assisted thoracoscopic lobectomy in the treatment of intralobar pulmonary sequestrationInteract Cardiovasc Thorac Surg 2011 12(1):77-79.10.1510/icvts.2010.25417720972207 [Google Scholar] [CrossRef] [PubMed]
[7]. Stern R, Berger S, Casaulta C, Raio L, Abderhalden S, Zachariou Z, Bilateral intralobar pulmonary sequestration in a newborn, case report and review of the literature on bilateral pulmonary sequestrationsJ Pediatr Surg 2007 42(4):19-23.10.1016/j.jpedsurg.2007.01.05417448748 [Google Scholar] [CrossRef] [PubMed]
[8]. Savic B, Birtel FJ, Tholen W, Funke HD, Knoche R, Lung sequestration: report of seven cases and review of 540 published casesThorax 1979 34(1):96-101.10.1136/thx.34.1.96442005 [Google Scholar] [CrossRef] [PubMed]
[9]. Wei Y, Li F, Pulmonary sequestration: a retrospective analysis of 2625 cases in ChinaEur J Cardiothorac Surg 2011 40(1):39-42.10.1016/j.ejcts.2011.01.08021459605 [Google Scholar] [CrossRef] [PubMed]
[10]. Frazier AA, Ryu JH, Pulmonary sequestration in adults: A retrospective review of resected and unresected casesBMC Pulm Med 2018 18(1):9710.1186/s12890-018-0663-z29871620 [Google Scholar] [CrossRef] [PubMed]
[11]. Dong Q, Zhao JP, Zhang L, Morelli J, Zhang ZK, Zhang P, STARD-compliant article: Comparison of pulmonary sequestrations with thoracic and abdominal aortic arterial supplyMedicine (Baltimore) 2019 98(27):e1622010.1097/MD.000000000001622031277133 [Google Scholar] [CrossRef] [PubMed]
[12]. Tsunezuka Y, Sato H, Intralobar pulmonary sequestration with three aberrant arteries in a 75-year-old patientChest 1998 114(3):936-38.10.1378/chest.114.3.9369743189 [Google Scholar] [CrossRef] [PubMed]
[13]. Traibi A, Seguin-Givelet A, Brian E, Grigoroiu M, Gossot D, Pulmonary intralobar sequestration in adults: Evolution of surgical treatmentRev Mal Respir 2019 36(2):129-34.10.1016/j.rmr.2018.10.00830686557 [Google Scholar] [CrossRef] [PubMed]
[14]. Ellis J, Brahmbhatt S, Desmond D, Ching B, Hostler J, Coil embolization of intralobar pulmonary sequestration - an alternative to surgery: a case reportJ Med Case Rep 2018 12(1):37510.1186/s13256-018-1915-530572944 [Google Scholar] [CrossRef] [PubMed]
[15]. Alsumrain M, Ryu JH, Pulmonary sequestration in adults: a retrospective review of resected and unresected casesBMC Pulm Med 2018 18(1):9710.1186/s12890-018-0663-z29871620 [Google Scholar] [CrossRef] [PubMed]