Leprosy is a chronic granulomatous infection as well as least pathogenic disease caused by Mycobacteriumleprae, having very prolonged incubation period, averaging 2 to 5 years (may range from 3 months to 40 years) with a prolonged germination time of 11 to 13 days. It primarily affects the peripheral nerves and secondarily involves the skin and some organ (Eyes, testes, joints, RE system, etc.,). According to World Health Organisation (WHO) leprosy has been eliminated (reported prevalence less than one case per 10,000 populations) from most of the 122 countries where it was considered a public health problem in 1985 [1]. However, pockets of high endemicity still persist in some regions of these countries. Bangladesh achieved elimination of leprosy at national and sub-national level in year 1998 and 2003 respectively. Although elimination level in many districts has been achieved, still significant number of new cases has been detected in many areas of the country including Chattogram and Dhaka Metropolitan area.
A case of leprosy is defined as an individual with one or more of the three cardinal signs, hypo-pigmented or erythematous skin lesions with definite loss or impairment of sensation, definite thickening of peripheral nerves with sensory impairment and Slit Skin Smear (SSS) positive for Acid Fast Bacilli (AFB) [2]. PB leprosy is defined as patients who are slit skin smear negative and having five or less than five skin lesions with at least one cardinal sign of leprosy. MB leprosy is defined as patients who are slit skin smear positive and having six or more skin lesions or more than one thickened peripheral nerve [3,4].
Materials and Methods
This was a retrospective study of all leprosy cases registered at the leprosy clinic, which is run by The Leprosy Mission International-Bangladesh (TLMI-B)-Chattogram programme, at Chattogram Medical College Hospital (CMCH), from January 2014 to December 2018. This institution is a tertiary care teaching hospital catering to a large population of Chattogram district including the native population as well as a large number of migrants from adjoining area of Feni, Noakhali, Cumilla, Chandpur, Cox’s Bazar, etc.,
A total of 161 newly detected leprosy patients, of both sexes, confirmed both clinically and bacteriologically, between 8 to 65 years of age, attending the leprosy outpatient clinic of Dermatology and Venereology Department of Chattogram Medical College Hospital (CMCH) between 2014-2018 were included in the study.
The number of skin lesions, neuritis, lepra reaction episode (Type I and Type II), deformity status (Grade-1 and Grade-2) in each patient was recorded on a body chart. Slit skin smear examination is performed at the time of registration as a protocol.
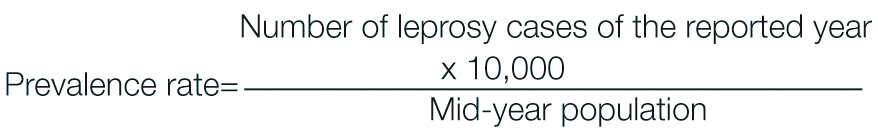
As per the policy, all patients are administered WHO-MDT PB (Dapsone 100 mg daily and Rifampicin 600 mg once a month) for 6 months and WHO-MDT MB (supervised dose of Dapsone 100 mg, Clofazimine 300 mg and Rifampicin 600 mg once a month plus Dapsone 100 mg and Clofazimine 50 mg daily) for 12 months. The prevalence rate was calculated using formula.
Statistical Analysis
Data were pooled and analysed. Continuous variables are expressed in Mean±SD and categorical variables in terms of numbers and percentage.
Results
From the [Table/Fig-1] it can be clearly seen that the total number of new patients have increased in 2018. Among the total 161 patients, majority had MB leprosy.
New Leprosy patients at CMCH.
| Year | 2014 | 2015 | 2016 | 2017 | 2018 | Total | Percent (%) |
|---|
| Population (panchlaish) | 442593 | 448877 | 458475 | 468278 | 474693 | | |
| New patient | 25 | 22 | 36 | 29 | 49 | 161 | 100 |
| PB | 5 | 3 | 8 | 4 | 14 | 34 | 21.12 |
| MB | 20 | 19 | 28 | 25 | 35 | 127 | 78.88 |
[Table/Fig-2] shows that the males predominated and the ratio of male to female was 2.66:1.
| Year | 2014 | 2015 | 2016 | 2017 | 2018 | Total | Percent (%) |
|---|
| Male | 18 | 17 | 26 | 25 | 31 | 117 | 72.67 |
| Female | 7 | 5 | 10 | 4 | 18 | 44 | 27.33 |
| Total | 25 | 22 | 36 | 29 | 49 | 161 | 100 |
[Table/Fig-3] shows that the highest number of patients were between 26-40 years of age (67/41.61%); the least being less than 14 years of age (11/6.83) from the year 2014 till 2018.
| Year | 2014 | 2015 | 2016 | 2017 | 2018 | Total | Percentage |
|---|
| <14 yrs | 3 | 1 | 3 | 1 | 3 | 11 | 6.83 |
| 15-25 yrs | 3 | 2 | 8 | 2 | 7 | 22 | 13.66 |
| 26-40 yrs | 9 | 7 | 13 | 17 | 21 | 67 | 41.61 |
| >40 yrs | 10 | 12 | 12 | 9 | 18 | 61 | 37.89 |
| Total | 25 | 22 | 36 | 29 | 49 | 161 | 100 |
From the [Table/Fig-4] it can be observed that most of the patients were detected passively (147,91.3%).
| Year | 2014 | 2015 | 2016 | 2017 | 2018 | Total | Percentage (%) |
|---|
| Active | 4 | 1 | 5 | 1 | 3 | 14 | 8.70 |
| Passive | 21 | 21 | 31 | 28 | 46 | 147 | 91.30 |
| Total | 26 | 23 | 36 | 29 | 47 | 161 | 100 |
From the [Table/Fig-5] it can be seen that out of 161 patients Type 1 reactions was seen in 48 (29.81%) patients and out of which 28 (17.39%) patients developed neuritis and Type 2 reaction was seen in 39 (24.22%) patients.
| Year | 2014 | 2015 | 2016 | 2017 | 2018 | Total | Percentage |
|---|
| Type 1 Reaction (Neuritis) | 12/25(8) | 9/22(9) | 9/36(5) | 9/29(4) | 9/49(2) | 48/161(28) | 29.81(17.39) |
| Type 2 reaction | 12/25 | 5/22 | 11/36 | 5/29 | 6/49 | 39/161 | 24.22 |
| Total | 24/25 | 14/22 | 20/36 | 14/29 | 15/49 | 87/161 | 54.04/100 |
From the [Table/Fig-6] it can be concluded that out of the 161 patients, most of the patients (31) had Grade 1 deformity. Twenty three patients had Grade 2 deformity. Highest number of deformities (18 cases) was found in 2018.
Disability/Deformity status.
| Year | 2014 | 2015 | 2016 | 2017 | 2018 | Total 161 |
|---|
| New pt | 25 | 22 | 36 | 29 | 49 |
|---|
| Gr-1 | 3 | 12% | 4 | 18.18% | 10 | 27.78% | 6 | 20.69% | 8 | 16.33% | 31 | 19.25% |
| Gr-2 | 4 | 16% | 4 | 18.18% | 3 | 8.33% | 2 | 6.90% | 10 | 20.41% | 23 | 14.29% |
| Total | 7 | 28% | 8 | 36.36% | 13 | 36.11% | 8 | 27.59% | 18 | 36.74% | 54 | 33.54% |
From the [Table/Fig-7] it can be observed that patients with slit skin smear positive was highest during year 2018 (20/ 54.14%) and was least during year 2015 (7/36.84%).
Slit skin smear findings in MB and PB patients.
| MB | PB |
|---|
| Year | Total | SSS positive | Percent % | Total | SSS positive | Percent % |
|---|
| 2014 | 20 | 12 | 60 | 5 | | |
| 2015 | 19 | 7 | 36.84 | 3 | | |
| 2016 | 28 | 18 | 64.29 | 8 | | |
| 2017 | 25 | 10 | 40 | 4 | | |
| 2018 | 35 | 20 | 54.14 | 14 | | |
| Conclusion | | |
[Table/Fig-8] shows that the prevalence rate, according to CMCH, gradually increased from 2016 (0.75) to 2018 (0.97). However, the national prevalence rate had decreased over the course of 5 years to 0.23.
Under Treatment Patients and Prevalence Rate (PR), 2014-2018.
| Year | 2014 | 2015 | 2016 | 2017 | 2018 |
|---|
| Population (panchlaish) | 442593 | 448877 | 458475 | 468278 | 474693 |
| Under Treatment Pt. 31st Dec (CMCH) | 42 | 35 | 34 | 36 | 46 |
| PR 31st Dec (CMCH) | 0.95 | 0.78 | 0.75 | 0.77 | 0.97 |
| National PR 31st Dec | 0.30 | 0.30 | 0.25 | 0.24 | 0.23 |
Hypopigmented anaesthetic patch, Claw hand deformity and Multiple hypopigmented anaesthetic patches seen in [Table/Fig-9].
a) Hypopigmented anesthetic patch in 25 years old male; b) Claw hand deformity (Grade 2); c) Multiple hypopigmented anesthetic patches in 8 years old boy.

Discussion
It was found that the number of patients increased in 2018 in comparison to 2014 and the number of MB patients is markedly higher than the number of PB patients. The increase in total number of leprosy patients is due to increased awareness of the disease, increased number of camps and surveys done at grass root level as well as more number of patients being referred by doctors. In comparison to a study done by Chhabra N et al., in Delhi showed out of 849 patients, 738 (86.9%) patients had MB leprosy and only 111 (13.1%) patients had PB leprosy which resembled the present study [5]. A further study carried out in Indonesia found that out of 94 patients, 51 patients (54.3%) had PB leprosy and 43 patients (45.7%) had MB leprosy which showed significant difference from the present study [6]. Another study carried out in Hyderabad, India showed that out of 295 patients, there were 256 (86.8%) PB patients and 39 (13.2%) MB patients which also differed from the present study [7].
In [Table/Fig-2], it can be observed that the total male patient (117/72.67%) is more than the female (44/27.33%) and the ratio of male to female is 2.66:1. Religious and social barriers exist among females which prevent them from active participation in camps and surveys and thus less female participants are screened every year. The low proportion of females in new cases may indicate differential access to diagnosis and treatment. Therefore, needs more careful consideration and more systematic collection of information.
Another study in Bangladesh showed that out of 670 patients, 488 (73.38%) were male and 182 (27.37%) were female which is almost remarkably close to the present study [8]. A study carried out in Indonesia found that out of 94 patients, female patients were 53 (56.4%) and male patients were 41 (43.6%) [6]. This significantly differed from the present study. Moreover, a study done in United Kingdom by Lockwood DNJ et al., showed that out of 28 patients, 19 were male and 9 were female [9].
In [Table/Fig-3], it can be concluded that the highest number of patients were between 26-40 years (67/41.61%) and above 40 years of age (61/37.89%). The least being less than 14 years of age (11/6.83%). The largest group of patients were from age group of 26-40 years because of the social pressure, they had to confront as well as greater concerns about their appearance. Greater mobility of this working age group are more exposed to infection. Least number of patients were found in less than 14 years of age group as case detection activities such as school surveys are not carried out regularly.
A study done in Indonesia showed that out of 94 patients most of the patients (34/36.2%) were between the age of 15-29 years and least (7/7.4%) were between 60-75 years of age. This resembled the present study i.e., there was higher number of prevalence in working age group [6]. Another study done on childhood leprosy in Hyderabad showed that out of 306 patients, almost equal number of cases were distributed between the age groups 6-10 years and 11-14 years, 142 (46.4%) and 146 (47.7%) respectively [7]. A further study done by Chen XS et al., in China showed that among the 1028 cases, most of the cases (484/ 47.08%) were between the age of 13-14 years and least (12/1.16%) were between 0-4 years [10]. However, this differed from the present study.
The profile and magnitude among paediatric population reflects epidemiology and the level of control of the disease in a community. A high child proportion signifies active and recent transmission of the disease.
In [Table/Fig-4], it can be observed that most of the patients were detected passively (147/91.3%) and only 14 (8.70%) patients were detected by active method. Active detections of patients were remarkably less due to less case detection activity (such as house to house survey, contact survey) due to less manpower in Government and Non-government organisations. Passive detection of patients is notably high as majority of the patients were referred by dermatologists and also doctors from other departments of chattogram medical college hospital.
In a study done by Lockwood DNJ et al., in United Kingdom revealed that among the 28 patients referred to the leprologist, 20 patients had seen a dermatologist, 9 patients had seen neurologist, 5 patients had seen an orthopaedic surgeon and 2 patients had seen a rheumatologist [9]. This showed that most of the cases were detected passively and is similar to the present findings.
The current detection of patients already with disabilities and the high proportion of Multibacillary (MB) cases indicate delay in detection in the community. Stigma surrounding leprosy and discrimination against persons affected by the disease continues to challenge early detection and successful completion of treatment. Many patients continue to experience social exclusion, depression and loss of income. Their families often also suffer due to stigma.
In [Table/Fig-5], it was observed that out of 161 patients Type 1 reactions was seen in 48 (29.81%) patients and out of which 28 (17.34%) patients developed neuritis and Type 2 reaction was seen in 39 (24.22%) patients. The rate of reaction is high due to delay in diagnosis and treatment as well as poor level of awareness.
A study done in Hyderabad, India by Jain S et al., showed that out of 306 cases, 91 (29.7%) developed reactions; 5 went into Type II and 86 into Type I reaction. Among the Type I reactions, 12 had Reversal Reaction (RR) alone, 15 had RR with neuritis and 59 had neurtitis alone. One child had both Type I and Type II reaction [7]. The rate of reaction found in the study was relatively less compared to the present study. Another study done in China showed that out of 1028 cases of leprosy 968(94.16%) didn’t develop any reactions, 35 (3.40%) developed Type I reaction and 25 (2.43%) developed Type II reaction [10]. As compared to the present study, their reaction rate was very low. An additional study done by Chhabra et al., in India showed that out of 849 patients, 258 (30.4%) developed Type I reaction and 60 (7.1%) developed Type II reaction [5]. In comparison to the present study, the rate of reaction was about 17% less than the present study. One more study carried out by Ghunawat S et al., in Delhi, India showed that out of 113 cases, 17 (15%) cases presented with reaction, which was remarkably lower than the present findings. Among them, 14 had Type I reaction and 3 had Type II reaction. There were 2 cases of neuritis [11].
In [Table/Fig-6], it can be concluded that out of the 161 patients most of the patients had Grade 1 deformity, 31 (19.26%). Twenty three (14.29%) patients had Grade 2 deformity. Highest number of deformities was found in 2018, 18 cases. This proves that such complications are common in leprosy. Though ratio of Grade 1 deformity increased from year 2014 to 2016, it decreased from year 2016 to 2018. However Grade 2 deformity increased in 2018. Delay in diagnosis and treatment, negligence in physiotherapy and rehabilitation are the major reasons for increased deformity among the leprosy patients.
A study done by Lockwood DNJ et al., in United Kingdom showed that out of 28 patients, 7(25%) patients had Grade 1 disability and 10 (36%) patients had Grade 2 disability. 2 patients (7%) showed both Grade 1 and Grade 2 disabilities [9]. This study showed higher number of disabilities and deformities as compared to the present study. Another study done by Chen XS et al., in China showed that out of 1028 patients, 771 (75%) showed no forms of disability, 125 (12.16%) had Grade I disability and 132 (12.84%) had Grade II disability [10]. The percentage of Grade 1 and Grade 2 deformity of this study was similar to the present study. A seperate study carried out by Ghunawat S et al., in Delhi, India, showed that out of 113 cases of leprosy, disability was noted in 28 (24.8%) cases, majority of the cases (21/18.6%) had Grade II disability while 7 (6.2%) were found to have Grade I disability. Among the total children suffering from disability, 18 (64.3%) had hand deformities, while the rest (35.7%) reported deformities of feet. None of the cases were found to have ocular deformities [11]. The percentage of Grade 2 disability was almost similar to the present study but Grade 1 disability was about 13% less as compared to the present study. Some other study done by Peters ES and Eshiet AL in South Eastern Nigeria reported that out of 2309 patients, 135 (5.2%) had Claw hand, 168 (6.4%) had Claw toes, 127 (4.9%) had Plantar ulcer, 117 (4.5%) had Palmar ulcer, 24 (0.9%) had Lagopthalmos, 98 (3.6%) had Ear and nose ulceration, 171 (6.6%) had Palmar insensitivity and 203 (7.8%) had Plantar insensitivity [12].
In [Table/Fig-7], it can be observed that patients with slit skin smear positive was found highest during year 2018 (20/ 54.14%) and was least during year 2015 (7/36.84%). According to the national guideline on Leprosy, PB patients doesn’t need to take SSS examination and thus smear was not taken. Although the ratio of smear positive MB patients fluctuated from year 2014 to 2018, it ranged from 35% to 65%.
A study done carried out by Chen XS et al., in China showed that out of 1028 cases reported, 482 (46.89%) were slit skin smear positive and 546 (53.11%) were slit skin smear negative [10].
In [Table/Fig-8], it can be seen that the prevalence rate, according to CMCH, gradually increased from 2016 (0.75) to 2018 (0.97). However, the national prevalence rate had decreased over the course of 5 years to 0.23. The present study was confined to a small area of Chattogram city which included remote hilly areas where carrying out surveys and providing health care is difficult. Thus the prevalence rate is found higher in this area. However the overall prevalence rate at national level had decreased.
In a study carried out by Chhabra N et al., in Delhi, India reported that national prevalence rate of India 0.68/10,000 population in March, 2012 and thus had achieved leprosy elimination at national Level [5]. Another study carried out by Sachdeva S et al., showed that prevalence rate in 0-5 years age group among males and females were (8.4% PB and 5.9% MB) and (7.7% PB and 3.8% MB) respectively [13]. The prevalence rate of Bangladesh nationally was 0.23 and at Panchlaish thana of Chattogram district was 0.97 in 2018, both of which (national and local) were below 1/10,000 population.
Future Recommendation
Prevention and care for disabilities is a challenge in most areas of the country, especially in the context of care after treatment to prevent and manage residual post-treatment disabilities.
It is recommended to revise primary health care system (grass root level) by including leprosy as a part and parcel started from community clinic.
Awareness for the general population through mass media television and newspaper is necessary. Training and resources for self-care should be provided to leprosy affected people, as well as monitoring of their condition and motivation. Training of medical officers, RMPs, religious leaders, social leaders, health care workers, teachers as well as patients is also required.
Limitation
As the data were collected from the small area of Chattogram city, it does not reflect the picture of whole country. This was a retrospective data analysis based on departmental records, hence bias in reporting may have occured.
Conclusion
Though a lot has been achieved at National level, much needs to be done in pockets of high prevalence area in terms of case detection, patient education and counseling, health awareness, rehabilitation, in addition to MDT coverage. To sustain elimination, current leprosy control activities should be continued with full force even in a low prevalence area that caters to a significant number of leprosy cases which ultimately helps to achieve the following targets:
Zero Gr-2 Disabilities (G2D) among paediatric leprosy patients; Reduction of new leprosy cases with G2D to less than 1 case per million populations; Zero countries with legislation allowing discrimination on basis of leprosy.
Declaration
Although we have permission from The Leprosy Mission International, Bangladesh (TLMI, B)-Chattogram program for data collection on research purpose, however, they didn’t have any ethical review committee and hence didn’t provide us with IEC approval number.