A Rare Case of Actinomycotic Mycetoma of Wrist
Pratibha Shamanna1, MS Nawaz Basha2, KN Nagegowda3, V Punith4, KN Shwetha5
1 Assistant Professor, Department of Microbiology, Sanjay Gandhi Institute of Trauma and Orthopaedics, Bangalore, Karnataka, India.
2 Postgraduate Student, Department of Orthopaedics, Sanjay Gandhi Institute of Trauma and Orthopaedics, Bangalore, Karnataka, India.
3 Postgraduate Student, Department of Orthopaedics, Sanjay Gandhi Institute of Trauma and Orthopaedics, Bangalore, Karnataka, India.
4 Technician, Department of Microbiology, Sanjay Gandhi Institute of Trauma and Orthopaedics, Bangalore, Karnataka, India.
5 Technician, Department of Microbiology, Sanjay Gandhi Institute of Trauma and Orthopaedics, Bangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: MS Nawaz Basha, Byrasandra, Jayanagara, Bangalore, Karnataka, India.
E-mail: nawazbashams@gmail.com
Mycetoma is a chronic, slowly progressing granulomatous subcutaneous infection caused by true fungi (eumycetoma) or filamentous bacteria (actinomycetoma). The present case report is a rare case of Actinomycotic Mycetoma involving wrist due to Streptomyces species. A 53-year-old male presented with multiple swellings over the right wrist and forearm with sinuses discharging sero-purulent pus since 3 years. Patient underwent incision and drainage and appropriate antibiotic course after the complete diagnosis. This case report emphasises the role of meticulous clinical examination assisted by microbiological cultures and histopathological studies which are mandatory in the diagnosis, management and assessment of the prognosis of such unusual cases.
Eumycetoma, Granulomatous, Madura foot, Streptomyces, Subcutaneous
Case Report
A 53-year-old male farmer presented with multiple boggy swellings in the right wrist and forearm since 3 years [Table/Fig-1]. Initially, he had developed two nodules following which there was a gradual increase in size and the number of swellings. The patient gave history of suppuration in the swellings, vesicles formation with sero-purulent discharge (pus) exuding from multiple sites. The patient had taken treatment at various places for the same but symptoms did not subside. There was no history of fever. He was diabetic, hypertensive, had ischemic heart disease and asthma. He was on medication for the comorbidities since 10 years. The patient was treated with several oral and injectable antibiotics in the past 3 years before presenting to us.
Multiple swellings on right wrist and forearm.

On examination there were multiple swellings (abscesses) measuring 2×2 cm, 2×3 cm with pus pointing, over the right wrist and forearm. The swellings were tender, hard in consistency and fixed to underlying tissues. There were tiny ulcerated areas with yellowish discolouration. He had restriction of wrist movements due to painful nodules and swellings. A provisional diagnosis of chronic fungal infection was made. Conditions like tuberculosis, sporotrichosis and chronic bacterial osteomyelitis were kept as differential diagnosis for this case.
Pus aspirated from the wrist and forearm area was sent to microbiology laboratory for Grams staining, Ziehl Neelsen’s stain, and aerobic, anaerobic and fungal culture. Gram’s stain revealed numerous polymorphonuclear neutrophils and no organisms. Ziehl Neelsen’s stain was negative for acid fast bacilli. The specimen was inoculated on Blood agar (BA), Mac Conkey agar and Thioglycollate broth and kept for incubation at 37°C. The specimen was also inoculated onto Blood agar and Robertson’s cooked meat media and kept in McIntosh Filde’s anaerobic jar for anaerobic culture. The specimen was also inoculated onto Sabouraud’s Dextrose Agar (SDA) for fungal culture, one kept at incubation temperature (37°C) and the other kept at room temperature (25°C).
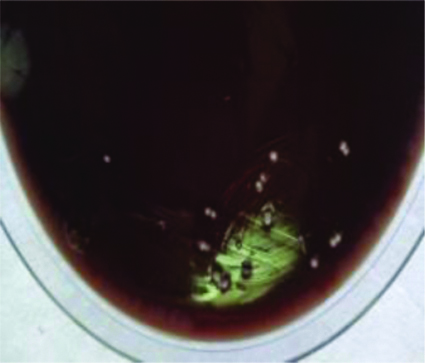
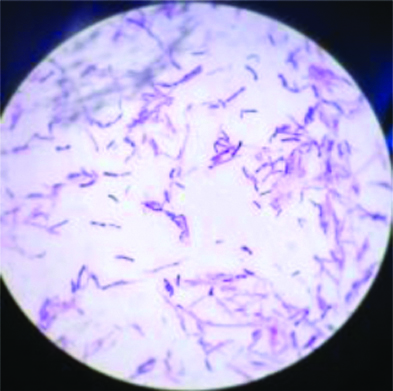
Aerobic culture yielded the growth of chalky white granular pitted colonies after 1 week of incubation on blood agar [Table/Fig-2]. There was no growth on Mac Conkey agar. Gram’s stain from the growth showed gram positive branching filaments [Table/Fig-3] which did not break up into bacillary forms (not fragmenting) and it was non-acid fast. Modified Kinyoun’s stain with 1% sulphuric acid was negative. Catalase test was positive. The colony morphology was consistent with that of Streptomyces species since colonies were powdery, white and demonstrated an earthy odour with aerial mycelium. Other biochemical tests like hydrolysis of casein, tyrosine, xanthine, gelatine and starch could not be performed for speciating the organism. The organism did not grow on SDA and also in anaerobic environment. The organism was identified as Streptomyces species based on the morphological appearance on gram’s stain, negative Modified ZN stain, growth on BA and other reactions. Antibiotic susceptibility was not performed due to poor growth on BA.
Growth of chalky white granular pitted colonies on Blood agar.
Gram stain showing gram positive branching filaments. (100X oil immersion objective)
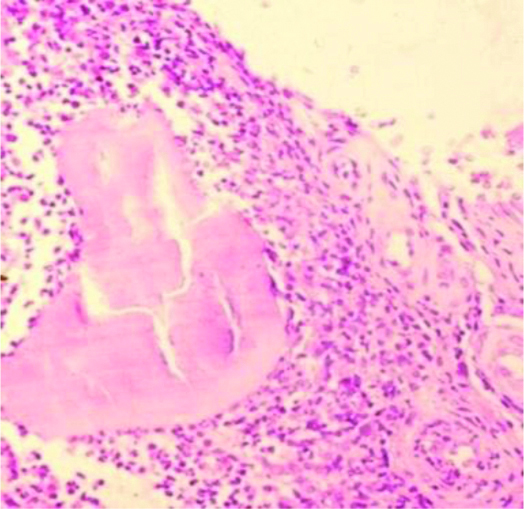
Montoux test was negative. X-ray of right wrist and forearm revealed soft tissue swelling with sclerosis of bone, focal lucencies and osteoporosis [Table/Fig-4]. Biopsy taken from the nodule including subcutaneous tissue on Haematoxylin and Eosin stain showed suppurative granulomas composed of neutrophils surrounding characteristic grains. Surrounding neutrophilic infiltrate was a layer of histiocytes, lymphocytes, plasma cells and macrophages. The outermost layer contained fibrous tissue and layers of fibrin [Table/Fig-5].
Wrist radiographs showing sclerosis of bone with focal radiolucency.

Suppurative granuloma surrounded by mixed inflammatory infiltrate comprising of lymphocytes, plasma cells, eosinophils, macrophages surrounding the granule. (H&E stain 40x magnification).
In present case, the patient underwent incision and drainage of the abscesses and was administered Inj. Cefperazone+Sulbactam 1.5 gm BD for 5 days. Later once the culture yielded Streptomyces spp., the patient was administered trimethoprim and sulphamethoxazole (cotrimoxazole) 80/400 mg along with doxycycline 100 mg BD for two months. Following which all the lesions flattened and symptoms subsided [Table/Fig-6].
Healed wound with scarring after two months.

Discussion
Mycetoma, synonym for “Madura foot” is a chronic, localised, slowly progressive granulomatous subcutaneous infection characterised by classical triad of subcutaneous swellings, formation of sinuses and discharge containing grains. Nearly, 20 members of the filamentous bacteria and filamentous fungi are the causative agents [1].
Mycetoma mainly occurs in the tropics and subtropics commonly among males (3:1 male to female ratio) aged 20-50 years old who are involved in agricultural work. Majority of patients have disease duration of less than 5 years at presentation. There are no health conditions which favour mycetoma. Local injury to bare skin by plant or soil saprophytes is the usual mode of entry. Common sites affected are feet, hands or back [1]. Hand mycetoma is not well described, causing deformity and disability that interfere with daily activities unlike foot mycetoma. Mycetoma is either Eumycotic or Actinomycotic in aetiology. Important species causing Actinomycotic mycetoma belong to the genus Actinomadura, Nocardia and Streptomyces species It was reported that more than 3100 species have been described in the genus Streptomyces of which Streptomyces somaliensis has been the most widespread etiologic agent causing human infections. Streptomyces somaliensis is one of the important aetiologic agents of actinomycetoma in countries like South America, Africa, India, Mexico, Malaysia and USA [2]. Medical treatment shows a favourable outcome in actinomycetoma than eumycetoma with available current therapies [3]. Here we report a case of Mycetoma of wrist caused by Streptomyces species for its rare occurrence.
Streptomyces species is an aerobic actinomycete that commonly occurs in the soil as a saprophyte. It is a gram positive bacterium which is an important cause of actinomycetoma. Actinomycetomas are chronic infections that can spread to affect deeper tissue and are characterised by the formation of tissue masses which may result in tissue destruction, deformity and sometimes may be fatal without intervention [4].
In 70% of the cases, myectoma affects the foot explaining the synonym Madura foot. The next most common site is hand [5-8] followed by the scalp [9] Ozden R et al., reported a of actinomycetoma of extremity caused by Streptomyces species [10]. Dogra A et al., reported a case of actinomycetoma in a 25-year-old female involving left foot. Diagnosis was made by gram’s stain and confirmed by histopathological examination [11]. Tilak R et al., has reported a case of actinomycotic mycetoma involving the right foot in a 45 years old male with history of multiple swellings over right foot with sinuses discharging sero-purulent pus. It was also seen that Actinomadura madurae was identified by microbiological culture from the pus obtained directly from lesion [12]. Diagnosis of Mycetomas is usually established on combination of clinical features, cytological/histopathological examination, culture, serological tests and radiodiagnosis. In the present study, diagnosis was made by gram’s stain, culture and histopathological examination. The Actinomycetales include Streptomyces, Actinomycetes and Nocardia. Streptomyces are differentiated from Actinomycetes by being aerobic and from Nocardia by being non-acid fast organisms that do not fragment into bacillary forms. Streptomyces species are characterised by formation of long, filamentous extensively branched gram positive bacilli, with irregular staining [2]. Branched morphology on grams stain along with culture, help to differentiate Streptomyces from Nocardia species. To date, culture remains the gold standard for etiological diagnosis. On Blood agar, Streptomyces produces dry, chalky, grey white colonies with earthy odour and aerial mycelium [2]. Joseph MN et al., reported a case of Streptomyces bacteremia in a patient with actinomycotic mycetoma [13]. Case reports of peritonitis [14], pericarditis [15], brain abscess [16] and endocarditis of prostetic aortic valve [17] caused by Streptomyces spp. have also been described in literature. Kapadia M et al., have described 6 cases of invasive Streptomyces infections [18]. Chander J et al., has described a case of human cervico-facial actinomycetoma caused by Streptomyces gresius [2].
Differentiation between Actinomycetoma and Eumycetoma is important as treatment options for both of them differ. These organism produces antibiotics used to treat bacterial, mycobacterial, fungal and parasitic infections. In mycetomas due to Streptomyces, streptomycin used in combination with dapsone or sulfamethoxazole has a better outcome. A two-step regime proposed by Welsh O et al., in the treatment of actinomycotic mycetomas consists of four injections of penicillin and two of gentamycin daily, in the intensive phase of 5-7 weeks followed by maintenance phase with amoxicillin/doxycycline and cotrimoxazole till 2-5 months [19]. Another study suggested a modified two step treatment for actinomycetoma consisting of an intensive phase in which a combined treatment of intravenous gentamicin with oral cotrimoxazole twice daily is given for a period of 4 weeks followed by maintainance phase with cotrimoxazole and doxycycline given twice daily for 5-6 months [20]. Combination therapy is usually recommended for treatment of mycetomas. It is preferable to monotherapy because of its synergistic effects and decreased likelihood of development of resistance and also to eradicate residual infection [21]. Early diagnosis and treatment is important to avoid amputations. Continuous clinical follow-up is needed to detect recurrence which is common.
Conclusion
An unusual case report of mycetoma of the hand caused by Streptomyces species has been reported which emphasises the need for multidisciplinary approach by clinical examination, microbiological culture and stains and histopathological examination which is mandatory in prompting proper therapy.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jul 24, 2019
Manual Googling: Oct 22, 2019
iThenticate Software: Nov 19, 2019 (15%)
[1]. Mohammad N, Arif C, Rukhsana P, Rokon U, Abdur R, Moydul H, Robert The Madura Foot- A Case ReportN Dermatol Online 2011 2(2):70-73. [Google Scholar]
[2]. Chander J, Singla N, Handa U, Human cervicofacial mycetoma caused by Streptomyces gresius: First case reportJournal of Microbiology, Immunology and Infection 2015 48:703-05.10.1016/j.jmii.2012.12.00223465713 [Google Scholar] [CrossRef] [PubMed]
[3]. Jahromi BS, Mycetoma in Iran: Causative agents and geographic distributionIndian J Dermatol 2014 59(5):52910.4103/0019-5154.13988925284877 [Google Scholar] [CrossRef] [PubMed]
[4]. Kirby R, Sangal V, Tucker PN, Czerwinska ZJ, Wierzbicka K, Herron RP, Chu JC, Draft Genome Sequence of the Human Pathogen Streptomyces somaliensis, a Significant Cause of ActinomycetomaJournal of Bacteriology 2012 194(13):3544-45.10.1128/JB.00534-1222689234 [Google Scholar] [CrossRef] [PubMed]
[5]. Pratibha S, Arundathi S, Lakshmi KS, Praveen Kumar R, Primary actinomycosis of the right upper extremity- an unusual presentationTropical J Path Micro 2018 4(1):59-62. [Google Scholar]
[6]. Balakrishna M, Nallaiah R, Sridevi V, Vijayalakshmi CS, Primary actinomycotic mycetoma of the hand and wrist- A case reportJournal of Medical Science and Clinical Research 2014 2(9):2266-69.Available at: https://jmscr.igmpublication.org/v2-i9/22%20jmscr.pdf [Google Scholar]
[7]. Kundu ZS, Singh R, Rana P, Bala R, Sangwan SS, Walecha P, Actinomycosis of hand and wrist: A case reportThe Internet J Orthop Surg 2007 5(1)10.5580/151e [Google Scholar] [CrossRef]
[8]. Padhi S, Dash M, Turuk J, Sahu R, Panda P, Primary actinomycosis of handAdvanced Biomedical Research 2014 3:22510.4103/2277-9175.14570025538911 [Google Scholar] [CrossRef] [PubMed]
[9]. Arora V, Handa B, Actinomycetoma of temporal bone: A rare case reportIndian J Otol 2015 21:298-302.10.4103/0971-7749.164548 [Google Scholar] [CrossRef]
[10]. Ozden R, Hakverdi S, Uruc V, Dogramaci Y, Kalaci A, Mycetoma of the upper extremity; A reason for above elbow amputationVan Tip Dergis 2014 21(3):179-81. [Google Scholar]
[11]. Dogra A, Minocha YC, Gupta M, Khurana S, Actinomycotic MycetomaIndian J Dermatol Venereol Leprol 2000 66(6):318-19. [Google Scholar]
[12]. Tilak R, Singh S, Garg A, Bassi J, Tilak J, Gulati AK, A case of Actinomycotic Mycetoma involving the right footJ Infect Developing Countries 2009 3(1):71-73.10.3855/jidc.10819749452 [Google Scholar] [CrossRef] [PubMed]
[13]. Joseph MN, Harish NB, Sistla S, Thappa MD, Parija CS, Streptomyces bacteremia in a patient with actinomycotic mycetomaJ Infect Dev Ctries 2011 4(4):249-52.10.3855/jidc.64520440064 [Google Scholar] [CrossRef] [PubMed]
[14]. Gruet ML, Maydat L, Ferro R, Peritonitis a Streptomyces somaliensisBull Soc Med AfrNoire Lang. Fr 1970 15:609-10. [Google Scholar]
[15]. Shanley JD, Snyder K, Child JS, Chronic pericarditis due to Streptomyces speciesAm J Clin Pathol 1979 72:107-10.10.1093/ajcp/72.1.107453096 [Google Scholar] [CrossRef] [PubMed]
[16]. Clark PRP, Warnock GBR, Blowers R, Wilkinson M, Brain abscess due to Streptomyces griseusJ Neurol Neurosurg Psychiatry 1964 27:553-55.10.1136/jnnp.27.6.55314249398 [Google Scholar] [CrossRef] [PubMed]
[17]. Mossad BS, Tomford WJ, Stewart R, Ratliff BN, Hall SG, Case report of Streptomyces Endocarditis of a Prosthetic aortic valveJournal of Clinical Microbiology 1995 33(12):3335-37. [Google Scholar]
[18]. Kapadia M, Rolston KVI, Han XY, Invasive Streptomyces Infections. Six cases and literature reviewAm J Clin Pathol 2007 127:619-24.10.1309/QJEBXP0BCGR54L1517369139 [Google Scholar] [CrossRef] [PubMed]
[19]. Welsh O, Vera-Cabrera L, Welsh E, Salinas MC, Actinomycetoma and advances in its treatmentClin Dermatol 2012 30:372-81.10.1016/j.clindermatol.2011.06.02722682184 [Google Scholar] [CrossRef] [PubMed]
[20]. Ramam M, Bhat R, Garg T, Sharma VK, Ray R, Singh MK, A modified two step treatment for actinomycetomaIndian J Dermatol Venereol Leprol 2007 73:235-39.10.4103/0378-6323.3288817675730 [Google Scholar] [CrossRef] [PubMed]
[21]. Rai VM, Balachandran C, Actinomycotic mycetoma of the hand: A rare occurrenceIndian J Dermatol Venereol Leprol 2006 72:17810.4103/0378-6323.2566116707839 [Google Scholar] [CrossRef] [PubMed]