Ovarian Tumour in a Child with Vaginal Bleeding: A Rare Case Report
Amit Kumar1, Sambedna2, Rashi3, Amit Kumar Sinha4, Bindey Kumar5
1 Senior Resident, Department of Paediatric Surgery, AIIMS Patna, Patna, Bihar, India.
2 Senior Resident, Department of Obstetrics And Gynaecology, AIIMS Patna, Patna, Bihar, India.
3 Senior Resident, Department of Paediatric Surgery, AIIMS Patna, Patna, Bihar, India.
4 Assistant Professor, Department of Paediatric Surgery, AIIMS Patna, Patna, Bihar, India.
5 Professor and Head, Department of Paediatric Surgery, AIIMS Patna, Patna, Bihar, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sambedna, c/o Dr. Arjun Sharma, Pitrichhaya, Arpana Bank Colony, Ramjapal Road, Baily Road, Patna, Bihar, India.
E-mail: sambedna29@gmail.com
Gynaecological malignancy account for 2% of all kinds of cancer in children and 60-70% of these lesions arise from ovaries. The clinical manifestations and histological types of ovarian tumours in paediatric population are different from those seen in adults. In pre menarche group usually ovarian tumours are of germ cell origin. These germ cell tumours in paediatric age group may present with features of precocious puberty. We report a case of ovarian tumour that presented with features of isosexual precocious puberty in the form of vaginal bleeding, in a four-year-old female child. She underwent surgical exploration and removal of the tumour with an attempt to preserve the reproductive function. She was relieved of the symptoms followed by the tumour removal as evidenced by the regular follow-ups.
Benign mullerian cyst, Mass abdomen, Precocious puberty
Case Report
A four-year-old female child was presented to the Department of Paediatric Surgery, her mother complaint of bleeding per vaginum for four months duration. Bleeding was moderate in amount as her parents changed her diapers 4-5 times per day. Except for vaginal bleeding, there were no other signs suggestive of precocious puberty. There was no history of perineal trauma, meningitis, cranial irradiation, head trauma, seizures, visual disturbances or medication. Her perinatal history was uneventful. Family history was negative for precocious puberty. None of the siblings had suffered from similar illness in past.
On examination the general condition of the child was fair, weight was 14 kg and vitals were stable. On inspection of abdomen there was generalised distension more on the left side. On palpation, a solitary lump measuring approximately 10×8×8 cm was felt in left side of abdomen. Lump was involving the hypogastrium, left iliac fossa, umbilicus, left lumbar and left hypochondrium. Lump was non tender, cystic, with rounded margins and mobile in transverse axis only. The lower border could not be felt as it merged into the pelvis. External genitalia was normal. Patient was admitted and further investigated.
On routine investigations, haemogram showed Hb as 7.2 gm% for which blood transfusion was done. Kidney function test, serum electrolytes, liver function tests were normal. Coagulation profile was within normal limit.
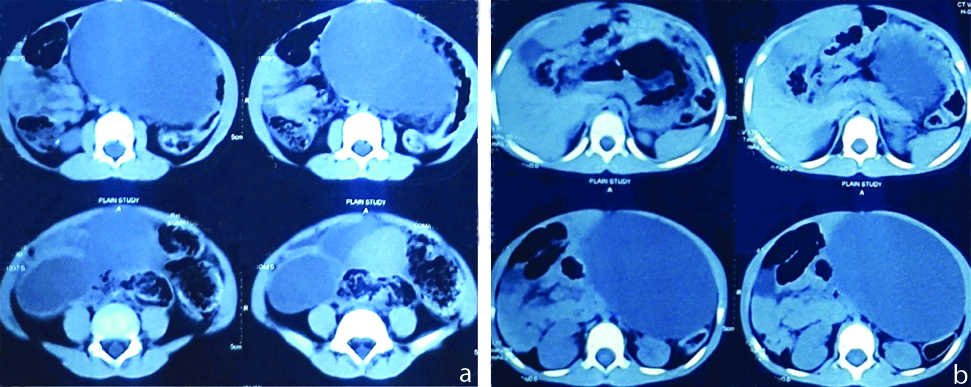
Ultrasound abdomen showed a cystic lesion with septations in both adenexa. Right adenexal cyst size was 41×31.5 mm and left adenexal cyst size 117.3×82.5 mm. Urinary bladder was adequately distended and lumen was echo free. Impression was bilateral ovarian cyst. Contrast enhanced computerised tomography abdomen and pelvis revealed a thin walled, well marginated abdomino-pelvic cystic lesion seen in the left side of the pelvis measuring 11.9×7.9×10.8 cm extending up to the left hypochondrium. Few enhancing thin septations were seen inside. Right ovary was not seen separately. The lesion was abutting and displacing the adjacent bowel loops; superiorly, it was abutting the splenic flexure and stomach; laterally, it was abutting the descending colon; medially, it was abutting the body and tail of pancreas; posteriorly, it was abutting the left kidney, left renal vessels and the aorta. The mass was so large that it was causing divarication of rectii muscles and eversion of umbilicus with minimal ascitis. Impression was ovarian tumour (cystadenoma) [Table/Fig-1].
CECT abdomen showing the ovarian tumours.
Fine Needle Aspiration Cytology (FNAC) revealed mesoepithelial cells with few degenerated cells and inflammatory cells comprising of lymphocytes. No atypical cells were seen. Impression was negative for malignancy.
Hormonal assay-alpha feto protein being 8 ng/mL (normal), CA-125 was 46.8 U/mL (slightly raised) and beta Human Chorionic Gonadotropin (HCG) was 0.01 miu/mL (normal). Serum oestrogen was 40 picograms (less than 20 picograms).
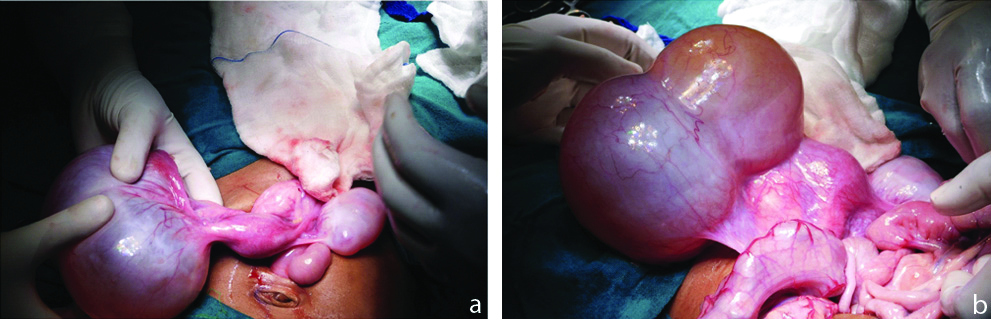
After optimisation of the general condition, the patient was posted for surgery. On exploration, a large left ovarian cyst measuring 12×10×10 cm and a smaller right ovarian cyst measuring 4×3 cm with haemorrhagic peritoneal fluid was observed [Table/Fig-2]. Left sided salphingo-oopherectomy was done with right sided ovarian cystectomy. Specimens were sent for histopathology.
Larger left and smaller right ovarian cyst.
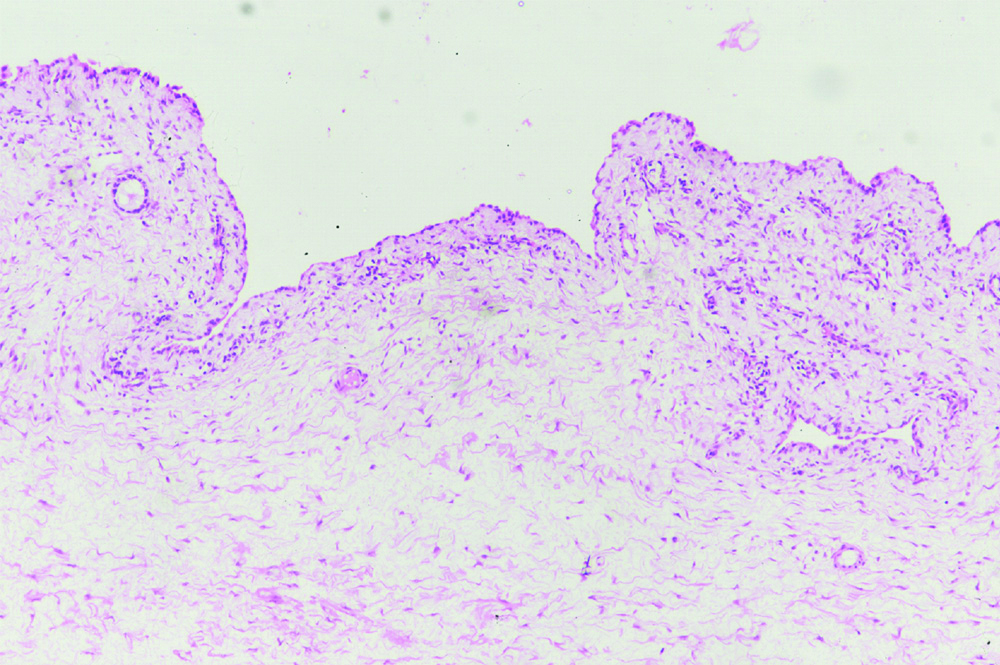
Histopathology revealed a multiloculated cystic lesion with serous fluid within it. Microscopically it contained cuboidal to columnar non ciliated epithelium with a thin layer of smooth muscle wall. Features were suggestive of benign mullerian cyst of bilateral ovaries [Table/Fig-3].
Picture of benign mullerian cyst of ovary (hematoxylin and eosin stain; original magnification x40.
Discussion
Ovarian tumours are usually rare before the age of menarche [1]. The germ cell tumours in paediatric age group may present with features of precocious puberty like vaginal bleeding [2] The estimated incidence of ovarian neoplasm is 2.6 cases per 100,000 girls per year [3].
Precocious puberty and menstrual irregularity related to oestrogen secretion are commonly associated with sexcord stromal tumours and gonadoblastomas; while, isosexual precocity also can be seen in approximately 6% of patients with malignant germ cell tumours [4,5]. Both neoplastic and non neoplastic tumours exhibit endocrine activity in approximately 10% of cases. Ovarian cysts of simple, follicular, and luteal type may secrete oestrogen and can cause isosexual precocious puberty. But the index case was a benign mullerian tumour presenting with isosexual precocious puberty (vaginal bleeding) which is a rare finding. Paraovarian cyst may mimic such presentation. Datti Sujata N et al., reported one such case of paraovarian cyst which turned out to be benign mullerian tumour on histopathology [6]. Gowri V et al., reported a case with Müllerian type cyst presenting with irregular bleeding per vaginum in a peri-menopausal woman [7]. Müllerian cysts are mostly benign but malignant transformation has been reported in a peri menopausal woman who was asymptomatic for 20 years for vaginal mullerian cyst. The histopathology confirmed it to be adenocarcinoma [8].
Conclusion
The diagnosis and management of ovarian tumours in a paediatric patient is a big challenge because of its varied possible pathologies, some of which are extremely rare. Non neoplastic lesions are now-a-days more commonly diagnosed because of better imaging modalities, biochemical, immune-histologic and cytogenetic technology. Preservation of reproductive and endocrine functions is of paramount importance in cases of infants and children. Most of them are non neoplastic ovarian tumours which are adequately managed with conservative surgical approach.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Sep 04, 2019
Manual Googling: Oct 17, 2019
iThenticate Software: Nov 23, 2019 (11%)
[1]. Ki EY, Byun SW, Choi YJ, Clinicopathologic review of ovarian masses in Korean premenarchal girlsInt J Med Sci 2013 10(8):1061-67.10.7150/ijms.621623801894 [Google Scholar] [CrossRef] [PubMed]
[2]. Nomelini R S, Micheletti A M, Adad S J, Androgenic juvenile granulosa cell tumor of the ovary with cystic presentation: A case reportEur J Gynaecol Oncol 2007 28(3):236-38. [Google Scholar]
[3]. Skinner M A, Schlatter M G, Heifetz S A, Grosfeld J L, Ovarian neoplasms in childrenArch Surg 1993 128(8):849-54.10.1001/archsurg.1993.014202000230048343057 [Google Scholar] [CrossRef] [PubMed]
[4]. Young R H, Dickersin G R, Scully R E, Juvenile granulosa cell tumor of the ovary: A clinicopathological analysis of 125 casesAm J Surg Pathol 1984 8(8):575-96.10.1097/00000478-198408000-000026465418 [Google Scholar] [CrossRef] [PubMed]
[5]. De B A, Madern G C, Oosterhuis J W, Hakvoort-Cammel F G, Hazebroek F W, Ovarian germ cell tumors in children: a clinical study of 66 patientsPediatr Blood Cancer 2006 46(4):459-64.10.1002/pbc.2063316206211 [Google Scholar] [CrossRef] [PubMed]
[6]. Datti Sujata N, Ray P, Jayashree AK, Shariff S, An unusual presentation of paraovarian cystJ Clin Biomed Sci 2013 3(4):196-98. [Google Scholar]
[7]. Gowri V, Busaidi FA, Vadakkepat N, Kaur S, Benign mullerian type cyst of the uterus in a perimenopausal womanSaudi Med J 2003 24(12):1400-01. [Google Scholar]
[8]. Lee KS, Park KH, Lee S, Kim JY, Seo SS, Adenocarcinoma arising in a vaginal müllerian cyst: A case reportGynecologic Oncology 2005 99(3):767-69.10.1016/j.ygyno.2005.07.12816169067 [Google Scholar] [CrossRef] [PubMed]