Benign Prostatic Hyperplasia (BPH) is one of the most common disorders affecting elderly men aged more than 50 years. Patients with BPH can have a significant impact on QoL as patients may have LUTS and majority may also have sexual dysfunction. The incidence of LUTS also increases with age. Around 30% of patients with age >65 years can have bothersome LUTS [1]; however, LUTS increases with age with 50-79 years, 80-89 years, and >90 years having around 56%, 70%, and 90%, respectively [2]. Several treatment modalities are used for the management of BPH; however, TURP is one of the most common surgical procedure performed in BPH.
Uroflowmetry is a simple urodynamic investigation used to measure the maximum flow rate (Qmax) for a given volume of voided urine. Being non-invasive it has been widely used in patients with LUTS. However, the value of uroflowmetry in the assessment of men presenting with LUTS thought to be secondary to bladder outlet obstruction is still unanswered. Among, Qmax and Qavg, the Qmax is more specific in identifying patients with BPH than Qavg. It has been well known that flow rate measurement is a reproducible technique that quantifies the strength of the urinary stream and when used with symptom scores have a greater probability of correctly characterising bladder outlet obstruction. It is also well known that Qmax has better association with the presence or absence of obstruction than symptoms.
The present study was performed to assess the role of uroflowmetry in LUTS evaluation due to BPH and use of uroflowmetry before and after TURP for BPH. Additionally, IPSS was also evaluated.
Materials and Methods
This was a prospective single centre study conducted between November 2016 and May 2018 at Department of Urology, Mysore Medical College and Research Institute, Mysore, Karnataka, India. Patients aged more than 40 years who presented with LUTS due to BPH and were recommended to undergo TURP were eligible for participation in this study. Patients with urethral stricture, bladder neck stricture, catheterised patients, and patients with acute urinary retention on indwelling periurethral catheter were excluded from the study.
The study protocol was approved by the Ethical Committee of Mysore Medical College and Research Institute. The study was conducted in accordance with the ethical principles that have their origin in the Declaration of Helsinki. Each study participant provided written informed consent for participation in the study. Participation in the study had no effect on the treatment in any way.
Eligible patients were included and a careful history especially about the symptoms was taken. A thorough physical, digital rectal examination of the prostate was done. All the necessary investigations including ultrasound Kidney, Ureter and Bladder (KUB), X-ray KUB, blood chemistry panel and group, urine routine, urine culture and sensitivity, liver function test, blood sugar were done. In selected cases if needed Prostatic Specific Antigen (PSA) was also done. Preoperative data was collected to note age, IPSS score, average flow rate (Qavg), Qmax, Post Void Residual Urine (PVRU), QoL and prostatic size. All these parameters were again recorded on Day 7, Day 30 and Day 90 postoperatively (TURP).
Statistical Analysis
Statistical analysis were done using SPSS Statistical Software (version 23, IBM, Chicago). Data was presented with summary statistics and Chi-Square, crosstabs, paired-t, repeated measure ANOVA, and Pearson’s correlation coefficient tests were used as appropriate. The level of significance for all tests was p<0.05.
Results
A total of 50 patients were included and evaluated in this study. The mean age was 67.62 (8.63) years and ranged from 42 to 83 years. A total of 20 (40%) patients were aged between 61 to 70 years, followed by 19 (38%) patients aged >71 years, three (6%) and eight (16%) patients were aged <50 years and between 61 to 60 years.
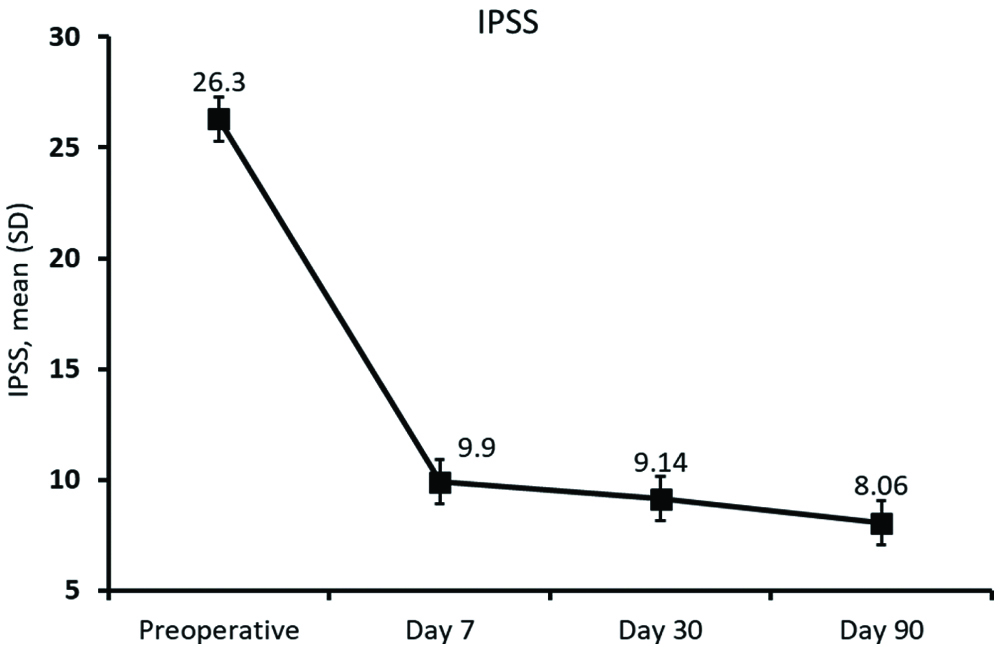
Preoperatively, no patients had IPSS score of <8, 5 (10%) patients had values between 9-19 and 45 (90%) patients had IPSS values >20. Postoperatively, significant (p<0.0001) improvement was observed in the IPSS score with 3 (6%) patients having values <8, 47 (94%) patients having values between 9-19 and none had above 20 [Table/Fig-1]. The mean (SD) IPSS score was 26.30 (4.03) which significantly improved (p<0.0001) postoperatively with 9.90 (0.79), 9.14 (0.90), and 8.06 (0.87) at Day 7, 30 and 90, respectively [Table/Fig-2].
Distribution of pre and postoperative IPSS and uroflowmetry values.
| Parameters | Preoperative n=50 | Postoperative n=50 | p-value |
|---|
| IPSS |
| 0-8 | 0 | 3 (6) | <0.0001 |
| 9-19 | 5 | 47 (94) |
| >20 | 45 (90) | 0 |
| Qmax (mL/seconds) |
| <10 | 50 (100) | 0 | <0.0001 |
| 10-15 | 0 | 4 (8) |
| >15 | 0 | 46 (92) |
| Qavg (mL/seconds) |
| <10 | 50 (100) | 36 (72) | <0.0001 |
| 10-15 | 0 | 14 (28) |
| Tmax (seconds) |
| <10 | 0 | 50 (100) | <0.0001 |
| 10-15 | 36 (72) | 0 |
| >15 | 14 (28) | 0 |
Data presented as n (%)
IPSS: International prostate symptomatic scoring; Qavg: Average flow rate; Qmax: Peak flow rate; Tmax: Time taken for voiding maximum volume/second
IPSS: pre and postoperatively at different timepoints.
IPSS: International prostate symptomatic scoring; SD: Standard deviation
Uroflowmetry study showed that preoperatively all 50 patients had Qmax <10 mL/seconds; however, postoperatively, 4 (8%) patients had Qmax between 10 to 15 mL/seconds, and 46 (92%) patients had >15 mL/seconds (p<0.0001). Preoperatively all 50 patients had Qavg <10 mL/seconds; however, postoperatively, 36 (72%) patients had Qavg <10 mL/seconds and 14 (28%) patients had between 10 and 15 mL/seconds (p<0.0001). The uroflowmetry mean time taken for voiding maximum volume in seconds (Tmax) values were between 10 and 15 mL/sec in 36 (72%) patients and >15 in 14 (28%) patients; however, postoperatively, all 50 (100%) patients had Tmax <10 mL/sec (p<0.0001).
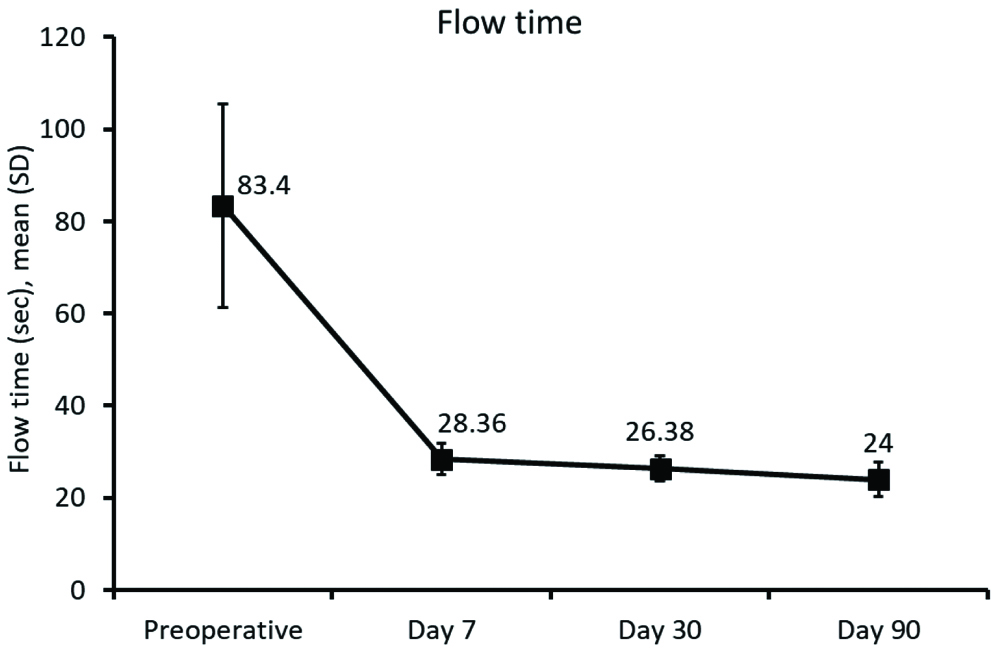
The uroflowmetry flow time (time taken for complete emptying of bladder i.e.,: F-tm) improved significantly (p<0.0001) after TURP with mean (SD) 83.40 (22.10) seconds preoperatively to 28.36 (3.42) seconds at Day 7 and 24.00 (3.71) seconds at Day 90 [Table/Fig-3].
Flow rate (F-tm): pre and post operatively at different timepoints.
F-tm: Flow time (time taken to complete emptying of bladder) in second; SD: Standard deviation
[Table/Fig-4] summarises the IPSS QoL parameters and shows that the greatest improvement was found for incomplete emptying, intermittency, weak stream, and straining. Of the symptom scores, highest mean scores were for frequency, weak stream and straining preoperatively and for nocturia and frequency postoperatively. The change in IPSS symptom score from preoperative to postoperative was found statistically significant with p<0.0001. Overall, the mean (SD) QoL due to urinary symptoms was 4.98 (0.43) preoperatively and was improved to 2.28 (0.45) postoperatively [Table/Fig-4].
| Parameters | Preoperative n=50 | Postoperative n=50 |
|---|
| QoL due to urinary symptoms | 4.98 (0.43) | 2.28 (0.45) |
| Incomplete emptying | 3.30 (0.65) | 0.74 (0.44) |
| Frequency | 3.96 (0.40) | 2.00 (0.00) |
| Intermittency | 3.34 (0.66) | 0.52 (0.50) |
| Urgency | 3.52 (0.65) | 1.02 (0.14) |
| Weak stream | 3.88 (0.56) | 0.98 (0.14) |
| Straining | 4.08 (0.83) | 0.78 (0.51) |
| Nocturia | 3.98 (0.47) | 2.00 (0.00) |
Data presented as mean (SD)
IPSS: International prostate symptomatic scoring; QoL: Quality of life; SD: Standard deviation
p<0.0001
[Table/Fig-5] summarises the comparison of IPSS and uroflowmetric parameters using paired sample statistics and showed significant improvement from pre to postoperative in all parameters. Patients had preoperative mean IPSS score of 26.30 and improved to 9.03; similarly, Qmax (6.90 to 16.77 mL/seconds), Qavg (3.14 to 9.51 mL/sec), Tmax (14.66 to 6.21 mL/seconds), and F-tm (83.40 to 26.25 seconds) were also improved.
Comparison of pre and post TURP.
| Parameters | Preoperative mean (SD) | Postoperative mean (SD) | p-value |
|---|
| IPSS | 26.30 (4.03) | 9.03 (0.73) | <0.0001 |
| Qmax | 6.90 (0.99) | 16.77 (1.06) | <0.0001 |
| Qavg | 3.14 (0.76) | 9.51 (0.95) | <0.0001 |
| Tmax | 14.66 (1.84) | 6.21 (0.52) | <0.0001 |
| F-tm | 83.40 (22.10) | 26.25 (2.36) | <0.0001 |
Data presented as mean (SD)
F-tm: Flow time (time taken to complete emptying of bladder) in second; IPSS: International prostate symptomatic scoring; Qavg: Average flow rate; Qmax: Peak flow rate; Tmax: Time taken for voiding maximum volume/second; TURP: Transurethral resection of the prostate
Discussion
Benign prostatic hyperplasia is a disease of old men, which lead to troublesome LUTS, has significant impact on QoL, social functioning, embarrassment, and anxiety. The clinical signs and symptoms that point to bladder outlet obstruction may be difficult to identify without specialised studies. Hence, it is important to have a protocol where the routine investigations and relevant examination will identify potential patients that may benefit from TURP.
In a recent study by Türk H and Ün S, which included 238 patients over 40 years with clinical BPH, LUTS and/or prostate volumes more than 25 mL showed that symptom scores increase from mild to severe; however, Qmax values decrease whereas prostate volume, PSA and postvoid residue increased [3].
Siroky MB et al., reported that uroflowmetry can separate physiologically unobstructed and obstructed bladder patients [4]. Gleason DM et al., found that peak flow rate can distinguish between normal men and patients with BPH, urethral stricture, or prostatitis [5]. However, peak flow rate alone may not be able to distinguish between patients with obstructed and patients with a decompensated detrusor muscle.
In the present study which included 50 patients with LUTS due to BPH who had underwent TURP, the mean age of the study population was 67.63 years and the most of the patients (40%) were aged between 61-70 years. Singla S et al., in their study showed almost similar results with patients mean age of 67.7 years [6]. Similarly, Jalbani MH et al., and Bar K reported patients with mean age 63.62 years and 68 years, respectively [7,8].
In the present study, preoperative Qmax was found to be 6.90 mL/seconds, which was consistent with previous reports where it was 7.6 mL/seconds and 7.1 mL/seconds reported by Jalbani MH et al., and Nielsen KT et al., respectively [7,9]. In the study by Nielsen KT et al., after TURP, Qmax at three months follow-up was 17 mL/seconds [9]. In another study by Songra MS and Rajiv Kumar, the preoperative Qmax value was 9.59 mL/seconds and which was improved to 17.33 mL/seconds postoperatively [10]. The average of first three months after postoperative follow-up of our patients (16.77 mL/seconds) was significantly improved similar to other previous reports.
In the present study, the preoperative Qavg was found 3.14 mL/seconds and the average of first three months of postoperative follow-up was 9.51 mL/seconds. However, in previous studies the Qavg was slightly higher than in the present study with Qavg increasing from 4.44 mL/seconds to 13.48 mL/seconds and from 5.18 mL/seconds to 11.92 mL/seconds [7,10]. Overall, it was noted that there is a significant improvement in Qavg after TURP in comparison with the preoperative Qavg.
In the present study, the preoperative Tmax was found to be 14.66 seconds and the average of first three months of postoperative Tmax was significantly improved with reduction in time to 6.21 seconds. Similarly, in the present study, the preoperative mean time taken for complete emptying of bladder in seconds (F-tm) was 83.40 seconds and the average first three months of postoperative follow-up was also significantly improved with reduction in time to 26.25 seconds. The IPSS in the present study showed a significant mean decrease (improvement) for all questions (p<0.005 for all symptoms). Overall, the results are similar to previous reports by Chuang FP, et al., and Porru D, et al., [Table/Fig-6] [11,12]. Another study, correlated the IPSS and uroflowmetry parameters in 51 patients who presented with LUTS-BPH and the mean Qmax was 15.6 mL/seconds and the mean voided volume was 193.0 mL. The correlation was not significant between IPSS and voiding time, flow time, and time to maximum flow; however, IPSS showed a negative correlation with maximum flow rate, average flow rate, and voided volume [13].
Comparison of IPSS with previous studies.
| Parameters | Present study | Chuang FP et al., [11] | Porru D et al., [12] |
|---|
| QoL due to urinary symptoms | Preoperative | 4.98 | 5.0 | 4.0 |
| Postoperative | 2.28 | 2.0 | 2.2 |
| Incomplete emptying | Preoperative | 3.30 | 3.5 | 2.7 |
| Postoperative | 0.74 | 0.6 | 0.6 |
| Frequency | Preoperative | 3.96 | 3.6 | 2.3 |
| Postoperative | 2.00 | 1.5 | 1.3 |
| Intermittency | Preoperative | 3.34 | 3.1 | 2.0 |
| Postoperative | 0.52 | 0.3 | 0.3 |
| Urgency | Preoperative | 3.52 | 2.4 | 1.7 |
| Postoperative | 1.02 | 0.4 | 0.7 |
| Weak stream | Preoperative | 3.88 | 3.6 | 3.0 |
| Postoperative | 0.98 | 0.5 | 0.2 |
| Straining | Preoperative | 4.08 | 2.6 | 2.4 |
| Postoperative | 0.78 | 0.3 | 0.1 |
| Nocturia | Preoperative | 3.98 | 3.2 | 2.8 |
| Postoperative | 2.00 | 2.1 | 0.8 |
IPSS: International prostate symptomatic scoring; QoL: Quality of life
Limitation
First, this was a single centre study, and second, the sample size was comparatively smaller, hence care must be taken when generalising the results.
Conclusion
Uroflowmetry parameters can be used to assess the symptoms as well as to predict the outcome of TURP. The IPSS is valuable in assessing the symptom complex of LUTS with BPH. TURP is still gold standard in improving the obstructive symptoms of BPH.
Data presented as n (%)
IPSS: International prostate symptomatic scoring; Qavg: Average flow rate; Qmax: Peak flow rate; Tmax: Time taken for voiding maximum volume/second
Data presented as mean (SD)
IPSS: International prostate symptomatic scoring; QoL: Quality of life; SD: Standard deviation
p<0.0001
Data presented as mean (SD)
F-tm: Flow time (time taken to complete emptying of bladder) in second; IPSS: International prostate symptomatic scoring; Qavg: Average flow rate; Qmax: Peak flow rate; Tmax: Time taken for voiding maximum volume/second; TURP: Transurethral resection of the prostate
IPSS: International prostate symptomatic scoring; QoL: Quality of life