Tunica Vaginalis Flap Repair for Urethrocutaneous Fistulae
Suersh Bhat1, Chandrasenan Nair2, Suyog Shetty3, Fredrick Paul4
1 Professor and Head, Department of Urology, Government Medical College, Kottayam, Kerala, India.
2 Associate Professor, Department of Urology, Government Medical College, Kottayam, Kerala, India.
3 Senior Resident, Department of Urology, Government Medical College, Kottayam, Kerala, India.
4 Associate Professor, Department of Urology, Government Medical College, Kottayam, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Suersh Bhat, Gandhinagar, Kottayam, Kerala, India.
E-mail: drsureshbhat@yahoo.com
Introduction
Hypospadias is a common condition which needs to be repaired within the first few years of life. However, the surgery is usually associated with several complications of which Urethrocutaneous Fistula (UCF) is the most common. Several surgical techniques have been described to correct these UCF. Use of a vascularized flap to repair this fistula is the current standard.
Aim
To assess the feasibility of using tunica vaginalis flap in repair of UCFs.
Materials and Methods
The present study was an observational study where 32 patients with UCF resulting from a previous failed hypospadias repair were subjected to tunica vaginalis flap repair. These patients were followed-up to a mean duration of 18 months to look for recurrence of fistula and other fresh complications.
Results
The study included 32 patients of whom 19 had a fistula after primary surgery, 9 had undergone 2 failed surgeries and 4 had undergone 3 previous attempts at hypospadias repair. Majority (29 patients) had a single UCF. No scrotal haematoma or testicular complications were noted. Penile cosmesis was satisfactory as determined by HOSE scoring system.
Erection seemed to be unaffected but could be a spurious result as majority of the patients were of pre-pubertal age. After median follow-up of 18 months, two cases had recurrence of fistula; both occurred within 1 month of the surgery.
Conclusion
Tunica vaginalis interposition flap repair of urethrocutneous fistula has good outcome.
Dartos flap, Fistula, Hypospadias
Introduction
Hypospadias is a congenital anomaly resulting due to the incomplete fusion of the urethral folds [1]. It is one of the most common congenital anomalies of urethra with a reported incidence of about 1 in 300 live male births. A surgical repair of hypospadias is the only available treatment for this anomaly. As many as 150 different surgical procedures have been described [2]. That in itself is a testimony of the fact that surgical hypospadias repair is fraught with complications and has high failure rates. UCF is the most common complication of hypospadias repair surgery [3].
Urethrocutaneous fistulae almost always requires a repeat and a more demanding surgery. The re-surgery itself is associated with a very high failure rate of about 10-40% [3]. The key factor considered necessary to prevent failure is the separation of the suture lines of skin and urethra with a well-vascularized elastic interposing tissue. Vascularized flaps such as dartos flap and Tunica Vaginalis Flap (TVF) were introduced to serve this purpose [4].
Though there is a large body of literature regarding use of dartos flap, studies regarding use of TVF in the setting of a UCF following hypospadias repair are few and most studies are found lacking in many aspects, sample size was very small in studies by Rouh JC et al., and Kadian YS et al., [5,6] also all the studies measured recurrence rates of fistula as the sole criteria to assess outcome of TVF repair.
Here, the present authors report the experience of using TVF as adjunct to fistula repair with an assessment of fistulae recurrence rates as well as an objective overall outcome assessment based on HOSE scoring system. [Table/Fig-1] a scoring system which was proposed and validated for hypospadias repair [7].
| Parameter | Score |
|---|
| Loction of meatus |
| Distal glans | 4 |
| Proximal glans | 3 |
| Coronal | 2 |
| Penile shaft | 1 |
| Meatus shape |
| Vertical slit | 2 |
| Circular | 1 |
| Stream |
| Single | 2 |
| Spray | 1 |
| Erection |
| Straight | 4 |
| <10 degree deviation | 3 |
| 10 o 45 degree deviation | 2 |
| >45 degree deviation | 1 |
| Fistula |
| No fistula | 4 |
| Single distal fistula | 3 |
| Single proximal fistula | 2 |
| Multiple fistulae | 1 |
Materials and Methods
This was an observational study by design; since such cases are rare, all patients who underwent UCF repair with a TVF between year 2012 and 2018, for a urethocutaneous fistula developing as a result of a failed hypospadias surgery undergoing repeat surgery at a tertiary care centre, were included in the study after obtaining an informed written consent. An ethical committee clearance for the study was obtained for the study from Institutional Review Board Board (No: 1/2017). A total of 32 patients fulfill the criteria. Detail of each case was recorded including the presence of co-morbidities, details of the primary surgery such as type of hypospadias, type of surgical repair done, time of fistula formation after surgery. Any secondary surgeries, number size and location of fistulae.
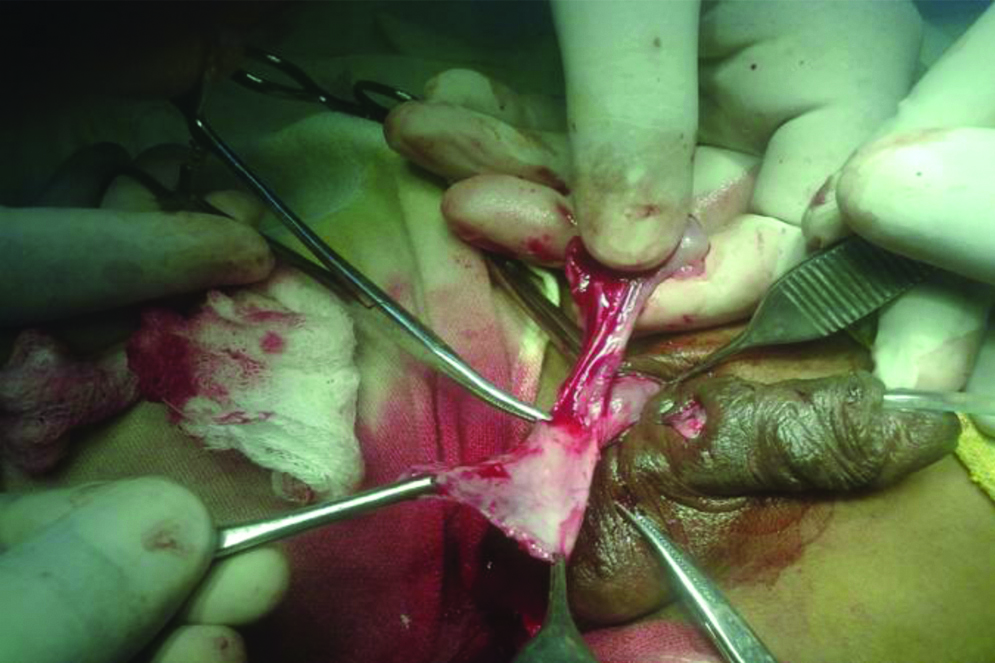
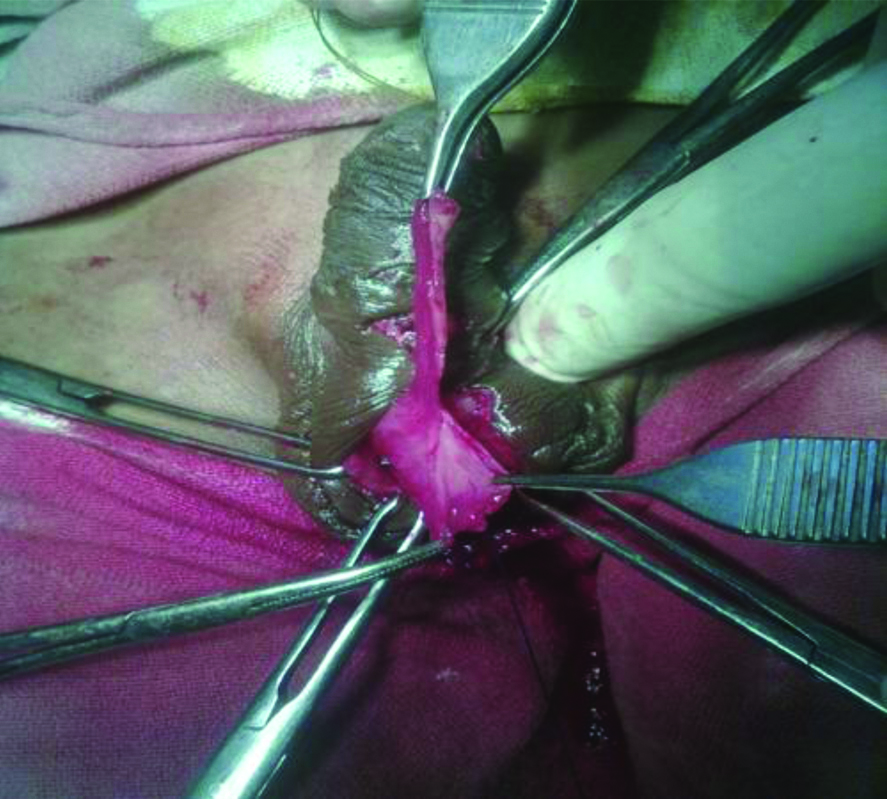
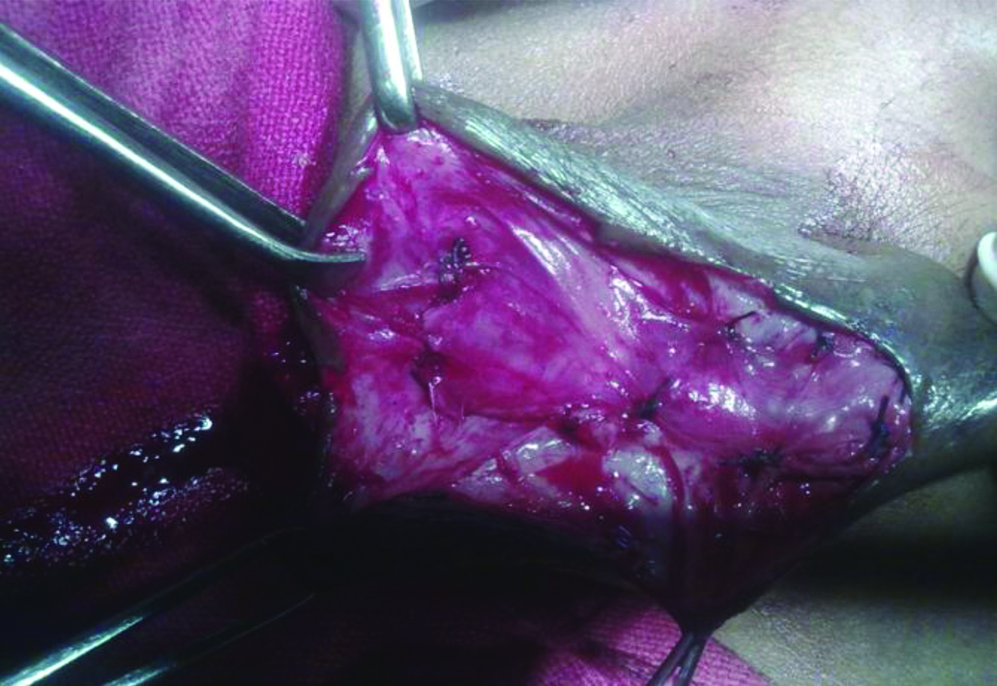
All patients underwent surgical repair. Intraoperatively distal urethral calibration was done. Methylene blue was injected into the urethra through meatus to confirm the exact location and number of UCF. An infant feeding tube or foley catheter of adequate calibre was placed in the bladder. Each UCF tract was excised, and the urethra was primarily closed using 4-0 vicryl suture. Testis was delivered out through a small incision at the root of scrotum and a superiorly based tunica flap was fashioned the TVF was then tunnelled underneath the penile skin and brought out through the most distal UCF and taken beyond UCF site and fixed distally using 4-0 vicryl [Table/Fig-2,3 and 4]. Penile skin was closed with 4-0 vicryl suture [Table/Fig-5]. Infant feeding tube was removed 7-10 days after surgery. Post-surgery patients were followed-up for complications like fistula recurrence, stricture, infections etc., up to 24 months. HOSE score was assessed at the end of 6 months and 1 year and 2 years. A score of 5 to 10 was categorised as poor outcome, 11 to 13 as satisfactory and ≥14 as a good outcome.
Fashioning the tunica vaginalis flap.
Transpositioning the flap onto the repaired urethra.
After completion of the flap interposition.

Results
Mean age of the patients was 11 years (±4.4), with the youngest patient being three and a half-year-old and oldest 22-year-old. Of the 32 patients, 19 had a fistula after primary surgery, 9 had undergone 2 failed surgeries and 4 had undergone 3 previous attempts at hypospadias repair. Majority (29 patients) had a single UCF, however, 3 patients had multiple fistulae. The location of the fistulae (a total of 35 fistulae in 32 patients) were 5 at penoscrotal junction, 22 at mid shaft and 8 subcoronal in location. Minimum time interval after the previous surgery was 12 months.
All the patients were discharged within 2-5 days after surgery. Wound infection was present in seven patients in the immediate post-operative period which was treated with topical and systemic antibiotics, all of them recovered well. No scrotal haematoma or testicular complications were noted. Penile cosmesis and function was good i.e., HOSE score of 14 or greater in 16 (50%) cases and was satisfactory i.e., a HOSE score of 11-13 in 12 (37.5%) cases indicting an acceptable outcome 28 cases (87.5%) and four cases showing poor outcome on HOSE scoring at six months postoperatively. At one year follow-up, the percentage of good outcome improved to 59.3% (19 cases) and 9 (28.1%) cases had a satisfactory outcome. However, the four cases showing poor outcome did not show any improvement [Table/Fig-6]. However, by two years post-surgery nine patients were lost to follow-up but the remaining 23 cases did not show any change in HOSE scores. Two cases had recurrence of fistula, both occurred within one month of the surgery. Among the recurrences, one case was a mid-shaft urethrocutneous fistula undergoing first re-surgery and the second one was a subcoronal fistula which was a second surgical attempt for urethrocutneous fistula repair.
Outcome of UCF repair using TVF.
| 6 months (N 32) | 1 year (N 32) | 2 years (N 23) |
|---|
| Good outcome (HOSE score ≥14) | 16 | 19 | 13 |
| Satisfactory (HOSE score 11-13) | 12 | 9 | 7 |
| Poor outcome (HOSE score ≤10) | 4 | 4 | 3 |
Hence the overall recurrence rate of our TVF flap repair procedure was 6% (2 out of 32 cases). In case of primary repairs it was 5.3% (1 out of 19 cases) whereas repeat procedures had a recurrence rate of 7.7% (1 out of 13 cases).
Discussion
TVF is a well vascularized flap which as seen by the results of this study has the potential to greatly reduce recurrences after UCF repair. Tunica vaginalis as a vascularized flap or graft has been used for correction of various penile pathologies. Peyronie’s disease and chordee correction were the first indications for which TVF was used [8,9]. Hafez AT et al., reported that the use of tunica vaginalis as a vascular flap was better than its use of a free graft in a rabbit model [10], hence paving way for the use of vascularized TV flaps instead of free grafts of tunica vaginalis [11]. The use of TVF as a vascularized flap in hypospadias repair was first thought of by Snow BW et al., [12]. Baskin LS and Ebbers MB, in their study found it better suited in view of its elastic nature, an advantage over lyophilized dura or dermis [13]. It has a dependable blood supply from the cremasteric vessels and its pedicle length could safely be increased up to the external inguinal ring thus providing ample length to repair a UCF anywhere along the length of the urethra. However, one needs to be careful while increasing pedicle length as the tissue becomes more flimsy proximally and at the same time inadequate pedicle length can cause tethering of the testis at a higher level compared to the normal side especially when penis is in an erect position as reported by Das S and Maggio AJ., in experimental animals [14].
The historical data suggests that success rates of UCF repair are about 9% whereas index study had a recurrence rate of 6% showing that tunica vaginalis flap is also better than the recurrence rate of 10% noted in a similar study by Sharma N et al., [15]. Moreover, previous failed UCF repairs did not seem to drastically worsen the success rates of the surgery in the present study as out of the 13 patients who had undergone a previous failed UCF repair only one patient ended up with failure.
It may be better than dartos flap as the skin has a lower healing rates due to hypo vascularity of the overlying skin when dartos is separated from skin.
The study also proved that the cosmetic outcome of the UCF repair using TVF was satisfactory in 87.5% cases, though the studies in the past were also of the same view their mode of assessment was a subjective one [5,16]. This study, on the other hand, proves it beyond doubt by using an objective validated tool in the form of HOSE scoring system.
Limitation
It is only an observational study comparing results with historical data. Longer follow-up untill the subjects attain puberty and become sexually active may be more informative regarding the functional outcome of the surgical procedure.
Conclusion
Tunica vaginalis interposition flap repair of urethrocutneous fistulae following a hypospadias surgery is a good option with very low recurrence rates and good cosmetic and functional outcomes. This is especially true in cases with multiple prior failed repairs as the local tissue is scarred and unsuitable for use. Also, a previous failed TVF repair also doesn’t compromise the repeat surgery chances as the contralateral testis can provide a fresh undisturbed donor site for the second attempt.
Author Declaration:
Financial or Other Competing Interests: No
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Aug 26, 2019
Manual Googling: Oct 21, 2019
iThenticate Software: Nov 23, 2019 (8%)
[1]. Culp OS, Experience with 200 hypospadias: Evolution of a therapeutic planSurg Clin North Am 1959 39:1007-23.10.1016/S0039-6109(16)35840-6 [Google Scholar] [CrossRef]
[2]. Retic AB, Keating M, Mandell J, Complications of hypospadias repairUrol Clin North Am 1988 15:223-35. [Google Scholar]
[3]. Elbakry A, Management of urethrocutaneous fistula after hypospadias repair: 10 years’ experienceBJU Int 2001 88:590-95.10.1046/j.1464-4096.2001.02390.x11678757 [Google Scholar] [CrossRef] [PubMed]
[4]. Yang SS, Chen SC, Hsieh CH, Chen YT, Reoperative Snodgrass procedureJ Urol 2001 166:2342-45.10.1016/S0022-5347(05)65585-1 [Google Scholar] [CrossRef]
[5]. Kadian YS, Rattan KN, Singh J, Singh M, Kajal P, Parihar D, Tunica vaginalis: An aid in hypospadias fistula repair: Our experience of 14 casesAfr J Paediatr Surg 2011 8:164-67.10.4103/0189-6725.8605422005357 [Google Scholar] [CrossRef] [PubMed]
[6]. Routh JC, Wolpert JJ, Reinberg Y, Tunneled tunica vaginalis flap is an effective technique for recurrent urethrocutaneous fistulas following tubularized incised plate urethroplastyJ Urol 2006 176(4 Pt 1):1578-80.10.1016/j.juro.2006.06.03216952688 [Google Scholar] [CrossRef] [PubMed]
[7]. Holland AJ, Smith GH, Ross FI, Cass DT, HOSE: an objective scoring system for evaluating the results of hypospadias surgeryBJU Int 2001 88:255-58.10.1046/j.1464-410x.2001.02280.x11488741 [Google Scholar] [CrossRef] [PubMed]
[8]. Amin M, Broghamer L, Harty JI, Long R, Autogenous tunica vaginalis graft for Peyronie’s disease: an experimental study and its clinical applicationJ Urol 1980 124:815-17.10.1016/S0022-5347(17)55681-5 [Google Scholar] [CrossRef]
[9]. Das S, Peyronie’s disease: excision and autografting with tunica vaginalisJ Urol 1980 124:815-17.10.1016/S0022-5347(17)55681-5 [Google Scholar] [CrossRef]
[10]. Hafez AT, Smith CR, McLorie GA, El-Ghoneimi A, Herz DB, Bägli DJ, Tunica vaginalis for correcting penile chordee in a rabbit model: is there a difference in flap versus graft?J Urol 2001 166:1429-32.10.1016/S0022-5347(05)65802-8 [Google Scholar] [CrossRef]
[11]. Caesar RE, Caldamone AA, The use of free grafts for correcting penile chordeeJ Urol 2000 164:1691-93.10.1016/S0022-5347(05)67084-X [Google Scholar] [CrossRef]
[12]. Snow BW, Cartwright PC, Unger K, Tunica vaginalis blanket wrap to prevent urethra-cutaneous fistulas an eight year experienceJ Urol 1995 153:472-76.10.1097/00005392-199502000-000617815624 [Google Scholar] [CrossRef] [PubMed]
[13]. Baskin LS, Ebbers MB, Hypospadias: anatomy, etiology, and techniqueJ Pediatr Surg 2006 41:463-72.10.1016/j.jpedsurg.2005.11.05916516617 [Google Scholar] [CrossRef] [PubMed]
[14]. Das S, Maggio AJ, Tunica vainalis autografting for Peyronie’s diseaseAn experimental study. Invest Urol 1979 17:186-87. [Google Scholar]
[15]. Sharma N, Bajpai M, Panda SS, Singh A, Tunica vaginalis flap cover in repair of recurrent proximal urethrocutaneous fistula: A final solutionAfr J Paediatr Surg 2013 10:311-14.10.4103/0189-6725.12542124469479 [Google Scholar] [CrossRef] [PubMed]
[16]. Landau EH, Gofrit ON, Meretyk S, Katz G, Golijanin D, Shenfeld OZ, Outcome analysis of tunica vaginalis flap for the correction of recurrent urethrocutaneous fistula in childrenJ Urol 2003 170:1596-99.10.1097/01.ju.0000084661.05347.5814501670 [Google Scholar] [CrossRef] [PubMed]