Now-a-days laparoscopy is widely used for various surgeries like appendicectomy, cholecystectomy, hernia, etc [1]. Laparoscopic surgery offers various advantages over the conventional open surgery such as less incisional pain, lesser incidence of ileus leading to rapid return to normal activity and shorter hospital stay [2].
The newer anaesthetic agents like sevoflurane and desflurane help in quick recovery following cessation of surgery [3]. Propofol is a highly lipid soluble agent and allows rapid induction of anaesthesia with rapid and clear- headed recovery, due to which it has become the preferred Intravenous (IV) anaesthetic agent for surgeries of short duration [4-7].
Sevoflurane is a sweet smelling newer halogenated volatile anaesthetic, with relatively low blood-gas partition coefficient of 0.69, which results in faster induction and emergence [8]. Both anaesthetic agents, propofol and sevoflurane are known to have minimal effects on haemodynamic parameters [9-13].
Various anaesthetic agents like propofol, sevoflurane, nitrous oxide, fentanyl and midazolam can lead to the development of post-operative cognitive dysfunction by acting on various receptors in the brain [14,15].
The reason for prolonged recovery after laparoscopic cholecystectomy can also be pain, nausea and vomiting. According to studies done by Cheng SS et al., Li M et al., Tan T et al., propofol based anaesthesia is associated with reduced post-operative pain compared with that associated with volatile agent based anaesthesia [16-18].
Recovery with respect to cognitive functions might be early after sevoflurane anaesthesia as compared to propofol in day care surgeries [19,20]. Though the clinical effects like Post-Operative Nausea Vomiting (PONV) and the recovery profile after administering propofol and sevoflurane have been studied in various outpatient operations but have not been much evaluated or studied in patients undergoing short day care procedures like laparoscopic cholecystectomy.
So, this study was conducted to compare propofol and sevoflurane for maintenance of anaesthesia with regard to recovery characteristics, cognitive functions as primary outcome and haemodynamics and PONV as secondary outcome.
Materials and Methods
The present, randomised prospective study was conducted on 80 patients of ASA physical status I-II, aged 18-60 years of either sex, who were operated for laparoscopic cholecystectomy under general anaesthesia from April 2017 to December 2017. Consort Flowchart is shown in [Table/Fig-1]. Institutional ethics committee approval (No.Trg.8(109)16/5831 dated 22/3/17) was taken prior to starting the study. Written informed consent was obtained from all the patients. Patients who belonged to ASA physical status III or more or those who have known allergy from study drugs, patients with psychiatric illness or history of previous cerebrovascular accident, alzheimer’s disease or presenile dementia and patients concomitantly taking anti-anxiety, anti-convulsant and anti-psychotic drugs were excluded from study.
Sample size was estimated based on pilot study, that mean difference in time to eye opening in two groups was 2.24 min with SD of 2.9. With this, the sample size was n=36 per group, at a power of 90% and confidence interval 95%. For possible dropouts, it was decided to include 40 patients per group.
The selected patients were randomly divided into two groups by computer generated randomised number and then by picking sealed envelope and divided into two groups of 40 patients each to receive propofol infusion (Group A) or sevoflurane inhalation (Group B) for maintenance of anaesthesia.
A thorough pre-operative check-up, general and systemic examination and routine investigations were done. All the patients were kept nil by mouth after the previous midnight of surgery. Cognitive functions were assessed preoperatively (1 hour prior) by Rivermead behavioural memory test, California verbal learning test and by asking name of surgeon and anaesthesiologist. In the operating room, baseline heart rate (HR), electrocardiography (ECG), non-invasive blood pressure (NIBP) and pulse oximetry (SpO2) were recorded in all patients.
All patients were given injection glycopyrrolate 4 μg/kg and injection midazolam 0.025 mg/kg via intravenous route. Injection fentanyl 2 μg/kg IV was given to all patients just before induction. In both the groups, induction was done with the injection propofol 2-2.5 mg/kg of body weight till initial loss of verbal contact and after checking for ventilation injection vecuronium 0.1 mg/kg IV was administered. Endotracheal intubation was done after 3 mins of intermittent positive pressure ventilation with an appropriate sized cuffed endotracheal tube.
Group A patients were maintained on N2O/O2 /(60/40%) and propofol infusion at the rate 50-100 μg/kg/min titrated so as to maintain adequate depth of anaesthesia.
Group B patients were maintained on N2O/O2 (60/40%) and sevoflurane 2-2.5% to achieve adequate depth of anaesthesia. In addition, 25-100 μg of fentanyl was given when Mean Arterial Pressure (MAP) and HR was 20% higher than baseline.
At the end of surgery, all patients received injection ketorolac 30 mg IV after stopping Injection Propofol or sevoflurane. Injection neostigmine 0.05 mg/kg IV and injection glycopyrrolate 0.008 mg/kg IV was used for reversal of neuromuscular blockade. Extubation was done after return of spontaneous breathing and adequate motor recovery. In the post-operative period, the observations were recorded by a separate anaesthetist who was blinded to the agent used during anaesthesia. The primary end point was to compare the recovery characteristics between the two groups.
Haemodynamic parameters ((HR, SBP, DBP and MAP) were recorded and compared at every 5 mins till the completion of surgery.
Recovery characteristics were recorded as:
a) Time from discontinuation of anaesthetic agents to spontaneous breathing and eye opening i.e., Emergence.
b) Time from discontinuation of anaesthetic agents to adequate response to verbal commands.
c) Time to extubation after discontinuation of anaesthetic agents.
d) Time from discontinuation of anaesthetic agents to orientation (to time, place and person).
e) Modified Aldrete scoring was recorded at every 15 minutes for one hour postoperatively. Patients required nine or more points for eligibility to discharge from the recovery room.
f) VAS score for post-operative pain was recorded every 30 mins for two hours in the recovery room.
Cognitive functions were assessed both preoperatively (1 hour prior) and postoperatively (after 2 hours) as:
Rivermead Behavioural Memory Test (RBMT): An animal was shown preoperatively to all patients and patients were asked to identify this animal postoperatively. The recall of location of this animal was also assessed.
California Verbal Learning Test (CVLT): In order to check verbal memory, patients were checked whether they could rename five fruits postoperatively which they themselves told preoperatively.
Patients were asked to recall the names of anaesthesiologist and surgeon both preoperatively and postoperatively.
Frequency of PONV was evaluated for first two hours in the recovery room by an independent observer. Any adverse effects like PONV fever, hypotension, bradycardia, hypertension, tachycardia, hypoxia was noted for first two hours after surgery.
Statistical Analysis
Descriptive statistics were done for all data and suitable statistical tests of comparison were done. Continuous variables were analysed with t-test and Mann Whitney U-test. Categorical variables were analysed with Chi-square test. Statistical significance was taken as p-value <0.05. Statistical highly significant was taken as p-value <0.001. Statistically non-significant was taken as p-value >0.05. The observations were depicted in tables. The data was analysed using IBMM SPSS statistics (22.00 version) and Microsoft Excel 2007.
Results
The two study groups were comparable with respect to the number of participants, age, weight, gender, ASA physical status (p>0.05) [Table/Fig-2].
| Group A | Group B | p-value |
|---|
| Number (n) | 40 | 40 | |
| Mean age (years) | 42.02±11.01 | 45.07±11.58 | 0.228 |
| Weight (kgs) | 63.95±8.59 | 63.85±6.76 | 0.954 |
| Gender (M/F) | 14/26 | 9/31 | 0.217 |
| ASA physical status (I/II) | 27/13 | 25/15 | 0.639 |
As shown in [Table/Fig-3], the time from cessation of sevoflurane to spontaneous breathing and eye opening, response to verbal commands, time to extubation, orientation were significantly shorter as compared to propofol group. Modified aldrete scoring was also compared every 15 mins postoperatively and the difference was significant just after extubation and at 15 mins.
Recovery characteristics in time intervals (in minutes) in both groups.
| Mean time (mins) | Group A | Group B | p-value |
|---|
| Time to spontaneous breathing | 4.37±0.77 | 2.32±0.79 | <0.001 |
| Time to eye opening | 6.42±0.78 | 4.12±0.68 | <0.001 |
| Time to response to commands | 8.02±0.73 | 6.15±0.73 | <0.001 |
| Time to extubation | 10.20±0.88 | 7.97±0.80 | <0.001 |
| Orientation(time to stating name) | 12.42±0.95 | 10.00±0.78 | <0.001 |
The mean heart rate was comparable in both the groups throughout surgery with lower readings at some points in the propofol group [Table/Fig-4].
Showing HR in both the groups.
| HR in bpm | Group A (bpm) | Group B (bpm) | p-value |
|---|
| Mean±SD | Mean±SD |
|---|
| Baseline | 77.45±6.20 | 78.37±9.13 | 0.598 |
| Preop | 76.85±6.30 | 78.62±7.92 | 0.271 |
| 5 min | 77.00±5.62 | 78.47±6.95 | 0.300 |
| 10 min | 77.00±7.14 | 78.57±7.27 | 0.332 |
| 15 min | 76.82±6.80 | 79.22±8.23 | 0.159 |
| 20 min | 76.35±6.54 | 79.37±8.05 | 0.069 |
| 25 min | 75.60±6.66 | 79.17±7.88 | 0.032 |
| 30 min | 76.17±6.51 | 78.77±8.16 | 0.120 |
| 35 min | 76.70±6.70 | 78.82±7.63 | 0.190 |
| 40 min | 76.67±6.26 | 79.00±7.88 | 0.148 |
| 45 min | 76.75±5.96 | 79.10±8.08 | 0.143 |
| 50 min | 77.10±5.82 | 79.70±8.06 | 0.102 |
| 55 min | 76.89±5.49 | 79.87±8.05 | 0.061 |
| 60 min | 76.85±5.44 | 80.23±7.69 | 0.040 |
| 65 min | 77.14±6.15 | 81.96±7.64 | 0.023 |
| 70 min | 78.75±5.73 | 84.13±7.38 | 0.049 |
| 75 min | 79.50±5.50 | 83.20±8.10 | 0.463 |
| 80 min | | 87.00±15.55 | - |
There was fall in MAP from baseline at all the time intervals. The MAP was significantly lower in propofol group at some points [Table/Fig-5]. Clinically all patients were haemodynamically stable but statistically it was significant with p-value<0.05. Propofol is direct arterial vasodilator, so there is fall in MAP in propofol group. Sevoflurane maintains cardiovascular stability better than propofol.
Showing MAP in both the groups.
| MAP (mm Hg) | Group A (mm Hg) | Group B (mm Hg) | p-value |
|---|
| Mean | SD | Mean | SD |
|---|
| Baseline | 95.42±9.97 | 96.05±9.90 | 0.779 |
| Preop | 93.25±8.97 | 94.25±9.34 | 0.627 |
| 5 min | 91.00±8.68 | 93.75±9.07 | 0.170 |
| 10 min | 90.55±8.87 | 93.77±8.86 | 0.108 |
| 15 min | 90.50±8.70 | 93.77±8.46 | 0.092 |
| 20 min | 90.20±8.82 | 93.57±8.48 | 0.085 |
| 25 min | 89.90±8.65 | 93.32±8.56 | 0.079 |
| 30 min | 89.52±8.00 | 93.75±8.31 | 0.023 |
| 35 min | 90.12±8.01 | 93.82±8.41 | 0.047 |
| 40 min | 89.75±7.13 | 93.35±8.40 | 0.042 |
| 45 min | 90.22±7.21 | 93.57±8.09 | 0.054 |
| 50 min | 90.00±7.44 | 93.37±8.15 | 0.057 |
| 55 min | 89.66±7.28 | 93.97±8.23 | 0.017 |
| 60 min | 90.52±6.70 | 94.29±8.28 | 0.043 |
| 65 min | 91.19±8.11 | 94.37±7.80 | 0.175 |
| 70 min | 91.91±7.94 | 95.60±6.52 | 0.198 |
| 75 min | 90.00±5.71 | 94.20±2.16 | 0.169 |
| 80 min | | 94.00±1.41 | |
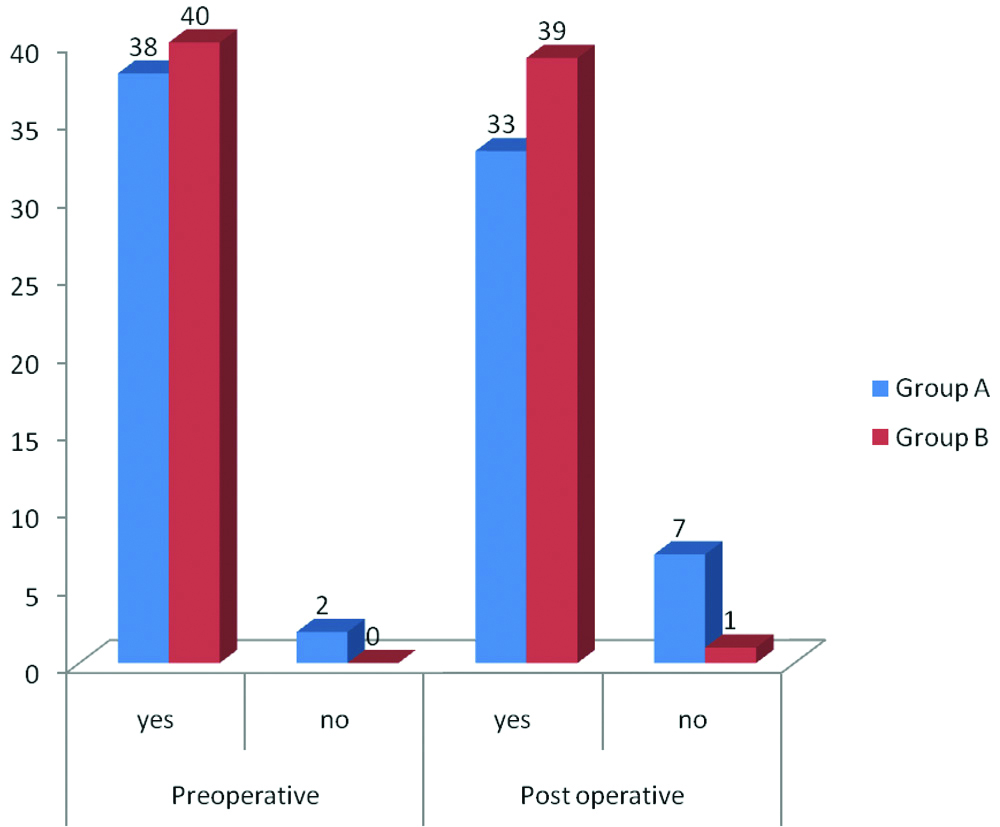
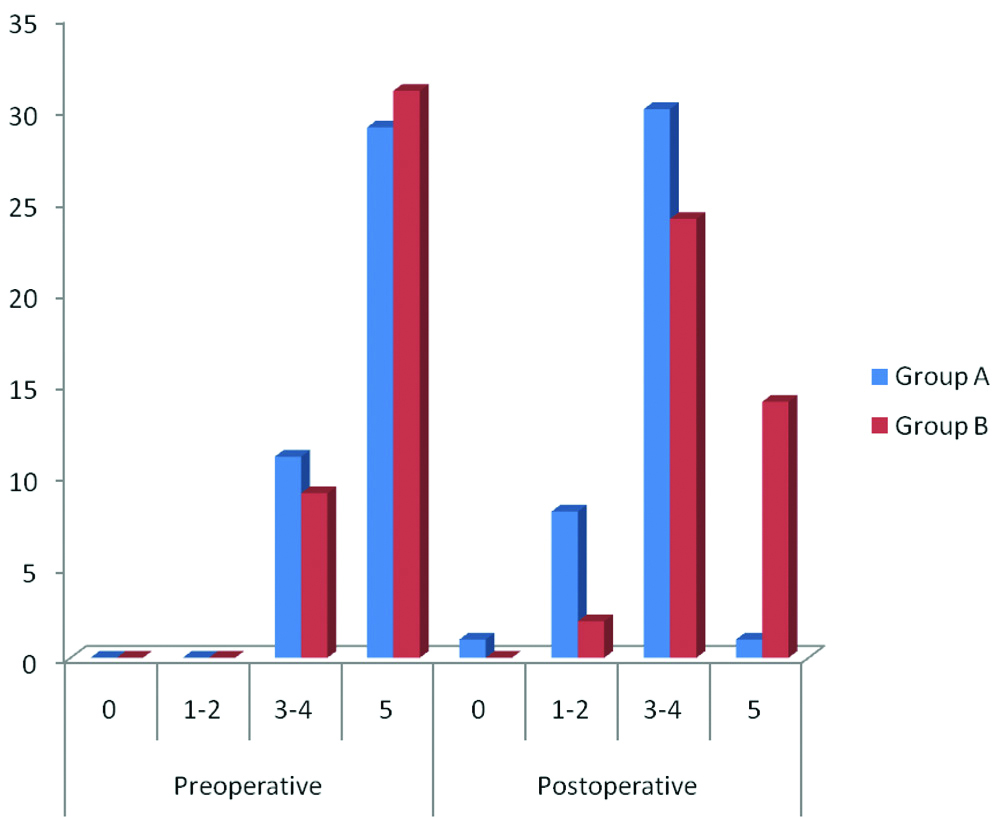
The results of cognitive tests and memory were comparable preoperatively. The difference was statistically significant postoperatively in RBMT, [Table/Fig-6] and CVLT, [Table/Fig-7].
Comparison of RBMT test in both the groups.
Number of fruits that patient could recall in propofol and sevoflurane group (CVLT).
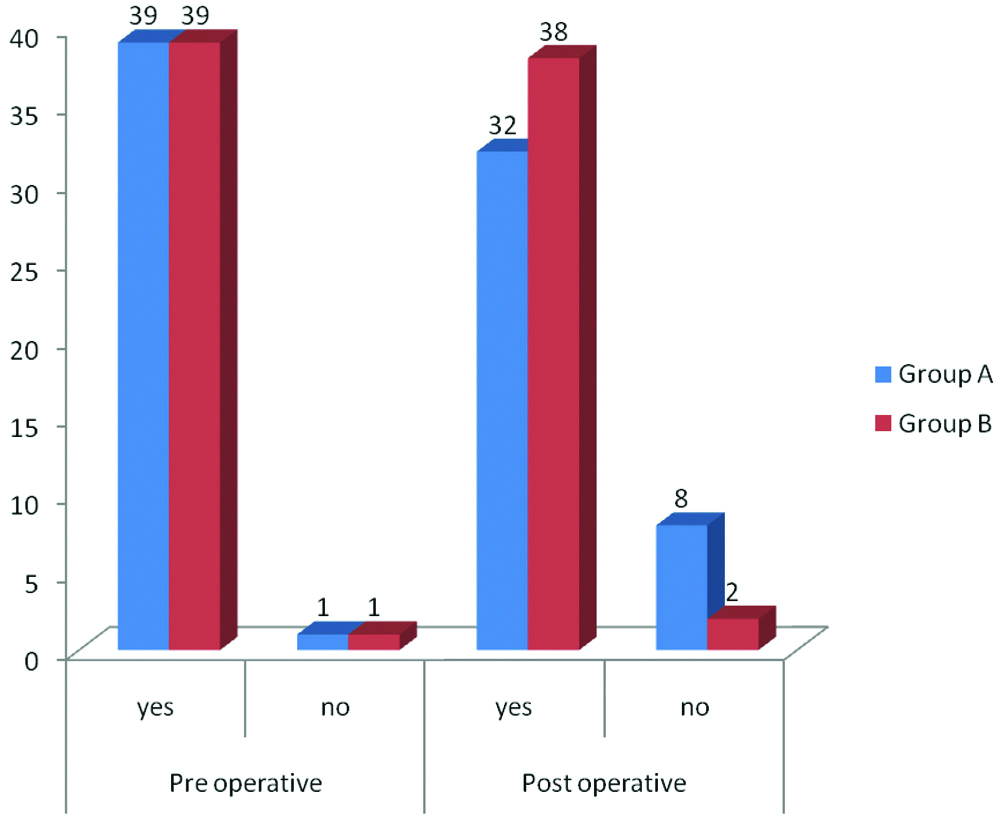
In regard to recall of surgeon’s name, difference between the groups was found to be statistically non-significant whereas it was significant in regard to recall of anaesthesiologist’s name [Table/Fig-8].
Number of patients who recalled the name of anaesthesiologist in group A and group B.
There was no significant difference between VAS score and other adverse effects like hypertension, bradycardia, hypotension, fever, hypoxia and tachycardia. But there was significant difference between incidence of nausea and vomiting being less in the propofol group [Table/Fig-9,10].
Showing VAS in both the groups.
| VAS | Group A | Group B | p-value |
|---|
| 30 min | 0 | 0 | 0 | 0.456 |
| 1-3 | 37 | 35 |
| 3-6 | 3 | 5 |
| 7-10 | 0 | 0 |
| 1 Hour | 0 | 0 | 0 | - |
| 1-3 | 0 | 0 |
| 3-6 | 40 | 40 |
| 7-10 | 0 | 0 |
| 90 min | 0 | 1 | 1 | - |
| 1-3 | 39 | 39 |
| 3-6 | 0 | 0 |
| 7-10 | 0 | 0 |
| 2 Hour | 0 | 38 | 36 | 0.396 |
| 1-3 | 2 | 4 |
| 3-6 | 0 | 0 |
| 7-10 | 0 | 0 |
Showing PONV in both the groups.
| Group A | Group B | p-Value |
|---|
| Nausea | 3 | 11 | 0.019 |
| Vomiting | 3 | 11 | 0.019 |
Discussion
In the present study, the time from cessation of anaesthetic agent to spontaneous breathing and eye opening, response to verbal commands, time to extubation and orientation were significantly shorter in sevoflurane group as compared to propofol group. Modified aldrete scoring was also significant after extubation and at 15 mins post-extubation. A statistically significant difference was also found postoperatively in RBMT and CVLT. Significant difference was also found with regard to recall of anaesthesiologist’s name. However, the incidence of nausea and vomiting was less in the propofol group.
Orhon ZN et al., also found early recovery times (Time to spontaneous respiration, eye opening obeying verbal commands and extubating the patient) were significantly longer in propofol group and they concluded that maintenance of anaesthesia with sevoflurane was associated with faster recovery than anaesthesia with propofol [21]. Wandel C et al., observed that patients who received sevoflurane were extubated at an earlier stage than those receiving propofol, and the times to eye opening and hand squeezing were also shorter [22]. Similarly, Singh SK et al., observed that sevoflurane group had better recovery profile with better cognitive function as compared to propofol group [4]. According to Khare A et al., the emergence time from discontinuation of the primary maintenance anaesthesia to spontaneous eye opening, response to verbal commands like squeezing hands, extubating patient and stating names were significantly lower in propofol group than sevoflurane group [23].
Larsen B et al., [15] and Robinson BJ et al., [24] found that patients in propofol group performed better with regards to their recovery profile and cognitive function as compared to sevoflurane group. Hocker J et al., however observed a shorter extubation time with propofol when compared to sevoflurane [25]. These observation could be attributed to a different patient population of a different ethnic group and difference in duration of surgical procedure. Few other studies, like the one by Arar C et al., extubation time and emergence characteristrics were similar in sevoflurane and propofol groups [26]. The patient population was different in this study also. Elderly patients were included in the study which could have resulted in present study results.
Post-Operative Cognitive Dysfunction (POCD) is characterised by new cognitive impairment with deteriorated emotional or social behaviour after a surgical procedure. In the index study, short-term POCD was evaluated. To check the cognitive functions, we performed RBMT and CVLT preoperatively (1 hour prior to surgery) and 2 hours postoperatively in both the groups. Both the groups were comparable preoperatively while the difference was significant postoperatively (2 hours). Name of the surgeon and anaesthesiologist were asked preoperatively (1 hour prior) and postoperatively (2 hours). There was statistical difference with regard to recall of anaesthetist’s name (p<0.05). Thus, post-operative cognition was better with sevoflurane than propofol.
Similar studies by Flouda L et al., [14], Samantaray A et al., [27], Schoen J et al., [11] and Magni G et al., [28] have shown that sevoflurane affects the cognition of adequately anaesthetised subjects less than propofol.
Emergence was faster and return of cognitive function were better in propofol group compared to sevoflurane group in study done by Larsen B et al., [15] and Shen Y et al., [29]. Thus inferences of different studies have been different.
In the present study, propofol has been shown to affect cognitive functions more in the immediate post-operative period. Sevoflurane may be a better agent as it preserves cognitive function, so it is a better option in day care surgery.
Modified Aldrete score was lower till 15 minutes after surgery in the propofol group. Similarly Goswami U et al., found significant difference till 5 minutes postoperatively [19] Bharti N et al., found the recovery time to achieve the aldrete score of 9 was same among groups [30].
Post-operative pain was assessed using VAS score postoperatively and there was no difference in the pain scores of both groups. Similarly according to Ortiz J et al., and Peng K et al., found no difference of pain scores in both groups [31,32]. PONV was significantly less in patients who received propofol infusion. Due to anti-emetic properties of propofol, there is lower incidence of PONV in propofol group, however Shah A et al., did not found significant difference in propofol and sevoflurane groups [1].
Limitation
All patients were induced with propofol, although maintenance was with one of the two agents i.e., propofol or sevoflurane 2%. This could have affected the study results. Another limitation could have been that the patients belonging to all age groups were selected, although the ages were comparable in the two groups. It would have been better if we would have selected a particular patient population like geriatric age group. Due to the low incidence of POCD, we decided to go ahead with the present study protocol.
Conclusion
Patients were haemodynamically stable throughout the surgery in both the groups but the emergence and recovery was significantly faster with better post-operative cognitive functions in the sevoflurane group. Therefore, sevoflurane might be considered as a useful alternative to propofol for maintenance of anaesthesia in laparoscopic cholecystectomies, especially in patients where rapid emergence and recovery of cognitive function is very much desired.