Patients on haemodialysis are at risk for contracting BBV infections like HIV, HBV, HCV infections. Longer duration of haemodialysis at more than one centre and not allocating designated dialysis machines for patients positive for BBV can contribute to nosocomial spread of infections. Blood transfusions can also increase the risk of spread of BBV in these susceptible populations [1].
Routine serological tests like Enzyme Linked Immunosorbent Assay (ELISA) or enhanced chemiluminescence tests are usually done before starting maintenance dialysis and at regular intervals to detect the occurrence of BBV in these patients.
The prevalence of HBV DNA in HBV serology negative dialysis patients was 48% in intermediate prevalence zone countries for HBV infections [2]. Kidney Disease: Improving Global Outcomes (KDIGO) guidelines, 2018 emphasises that in areas with high prevalence of HCV infection, initial screening with molecular test should be considered in dialysis units [3]. Polymerase Chain Reaction (PCR) or Transcription mediated amplification based molecular assays can detect viral nucleic acid in seronegative dialysis patients [4,5].
NAT routinely employed in blood donor screening, will be able to detect HCV RNA, HIV RNA, HBV DNA as early as 2.2, 4.9 and 14.9 days, respectively [4]. Hence, NAT can detect these infections earlier than routine serological assays and reduce the transmission of infections among patients in dialysis units.
In India, the prevalence of HCV RNA in Hepatitis C serology negative dialysis patients was between 23 to 50% [1,5]. But only seropositive prevalance of HBsAg and HIV among dialysis patients is available in the literature from India. There is no published data from India with respect to the prevalence of markers such as HBV DNA, HIV RNA in seronegative patients undergoing dialysis. India being an intermediate endemicity zone for HBV infection, the study was done to analyse if the NAT can detect pre-seroconversion and occult infections in dialysis patients who are routinely screened by serological tests.
Materials and Methods
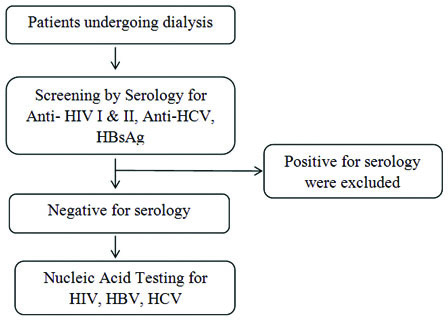
This was a prospective cross-sectional study on chronic kidney disease patients on maintenance dialysis (n=88) at a tertiary care centre in Southern India. Patients undergoing dialysis for atleast six months were included in the study between August 2017 and February 2018. Patients who were known seropositive for the BBV infectious markers at the initiation of study were excluded from the study [Table/Fig-1]. Based on the sensitivity observed in an earlier publication from India, with 10% allowable error and 95% confidence level, minimum sample size was estimated to be 76 and 88 samples were included [1].
Protocol for testing patients undergoing dialysis during the study.
The risk factors for BBV infection like dialysis at multiple centers, history of blood transfusions, frequency of dialysis and Hepatitis B vaccination titer levels were also collected from the medical records. Institutional ethics committee approval was obtained (IEC Number: IEC-AIMS-2017-BLOODB-149 date 29-4-17) before the initiation of the study. Informed consents were obtained from all the patients and samples were collected in vials with EDTA anticoagulant.
Serology Testing
The serology tests for dialysis patients includes HBsAg, Anti HIV I and II, Anti HCV were performed using Chemiluminescence Microparticle Immunoassay (CMIA) in the ARCHITECT i1000SR (Abott Laboratories, North Chicago, IL, USA). All patient’s in whom serology test results were negative, were included for Nucleic Acid Testing (NAT) to identify window period infections. Patient sample positive for serology or were not confirmed were excluded from the study.
NAT Testing
Two mL EDTA sample was collected from the 88 patients negative for serology and tested for HIV I RNA, HCV RNA, HBV DNA by NAT using Individual Donor Procleix Ultrio Plus Assay (Grifols Diagnostic Solution, USA). The NAT assay is based on Transcription Mediated Amplification (TMA) in which the assay amplifies portion of RNA or DNA using reverse transcriptase, RNA polymerase and T7 promoter. More than 1000 amplification products are produced in one cycle. Acridinium ester labelled probes were used for detecting amplified products.
Blood Transfusion
Blood components transfused throughout the study period were tested negative for serology and NAT.
Statistical Analysis
Standard statistical tests were performed using SPSS, version 20; descriptive statistics were used to determine frequency. Median with IQR was used to determine frequency. Pearson correlation was used to analyse the duration of dialysis and the volume of RBC transfusion.
Results
Eighty eight patients (62.5% male and 37.5% female) were included in the study after they were tested non-reactive for Anti HIV, Anti HCV and HBsAg by serology. Median age was 65 (IQR 49-70) years [Table/Fig-2]. Median duration of dialysis was 30 (IQR: 5-57) months. Dialysis was performed three times a week in 57% (n=50) and two times a week in 43% (n=38) patients. There were 12.5% (n=11) patients who had undergone dialysis at more than one centre. Median number of Packed Red Blood Cells (PRBC) components transfused per patient was 5 (1-10) units. The duration of dialysis had a low positive correlation with the volume of PRBC transfused among the patients (r=0.346, p=0.001).
Characteristics of patients undergoing dialysis at tertiary care centre in Southern India.
| Parameter | Median | IQR |
|---|
| Age (years) | 65 | (49-70) |
| Serum alanine aminotransferase (IU/mL) | 10 | (6-13) |
| Serum albumin (g/dL) | 3.7 | (3.1-4.1) |
| Serum urea (mg/dL) | 93 | (68-123) |
| Serum creatinine (mg/dL) | 7.8 | (5.9-11) |
| Duration of dialysis (months) | 30 | (5-57) |
| Blood transfusion (units) | 5 | (1-10) |
Anti HBs level >10 IU/mL was observed in 88% of patients and the rest were revaccinated for Hepatitis B. Biochemical marker ALT, serum urea and serum creatinine for patients enrolled was shown in [Table/Fig-2]. NAT test for all three markers HBV, HCV and HIV were non-reactive for all 88 patients.
Discussion
Patients who are on maintenance dialysis are considered for risk of infection with HCV, HBV, HIV. Risk for HCV infection is 100-1000 times higher than normal population [6]. Forty percent had atleast one of the three viral markers [7]. High frequency of these infections were reported in serology negative patients who were further tested using molecular assays. Hence dialysis patients have to be monitored closely to detect any such infections so that they can be given early treatment and prevent further spread of infections through dialysis units. The advanced BBV screening like NAT assay can detect infections which are not picked up by serological assay in an early stage of infection or in occult infection. The prevalence of infection among dialysis patients varies between dialysis units [2]. We did not encounter any occult infection or window period infection in the NAT assay performed in patients on maintenance haemodialysis. The adherence to robust infection control practices can reduce the occurrence of these nosocomial infections.
Longer the duration of dialysis, the patient is exposed to greater risk of contracting the blood borne infections. Jasuja S et al., has reported that there is a higher risk of infection after 16 months of dialysis [1]. We did not observe this in the index patient group who were on dialysis for up to 151 months. Patients who were on chronic dialysis (≥10 dialysis sessions) were significantly more likely to be infected compared to those who underwent lesser dialysis procedures [8].
We found that Anti-HBs level was more than 10 IU/mL in 88% of patients and the rest were revaccinated for Hepatitis B. Seroconversion after Hep B Vaccine (anti-HBs titre of >10 IU/L) was observed in 64% after primary immunisation as reported by Bel’eed K et al., [9]. Booster doses were intended to be given every three months to patients not attaining anti-HBs titre of >100 IU/L. The risk of HBV infection after exposure is the least when the titre attained >100 IU/L. Booster doses caused significant improvement in seroconversion in dialysis patients [9]. Even a double dose vaccination is recommended in CKD patients due to the inadequate response and rapid decline in antibody levels [10,11].
In the present study, median value of serum albumin (3.7 g/dL) and serum alanine aminotransferase (10 IU/mL) were within normal range. Liver biochemical parameters are often silent in end stage renal disease because of the immune suppression in them due to dialysis [12].
Transaminases levels are poor predictors of hepatocellular damage in uremic patients as it is often lower than normal patients due to multiple reasons like suppression of ALT synthesis, reduction in pyridoxal phosphate which is a coenzyme for transaminases and its accelerated clearance from serum [13]. The normal range of ALT for uremic patients is redefined to lower value (Upper limit of ALT 30 and 19 IU/dL for males and females respectively) for more accurate assessment [14].
In a multicentre study at Belgium, incidence of HCV seroconversion fell to zero with the improved enforcement of universal precautions. They reused the dialysers and did not isolate the HCV seropositive patients [15]. KDIGO guidelines, 2018 also states that separate HCV positive dialysers are not required if standard infection control practices are adhered [3]. Eventhough there is no consensus whether to isolate seropositive patients, it is widely agreed upon that highly trained staff was associated with decreased risk of seroconversion [16]. Failure in application of universal and/or dialysis-specific infection control measures have been reported to contribute to transmission of infection in dialysis units. HIV seroconversion rates were higher in centres where seropositives were dialysed and low level disinfectants were used for dialysers in reprocessing. The DNA sequencing of HIV strains from the seroconverters from a single dialysis centre were similar to each other which evidenced the cross contamination [8]. Our dialysis unit practices the reuse of dialysers after formaldehyde sterilisation. Reuse of dialysers is more economic and leads to less biomedical solid waste [17]. Infection control and hand hygiene practices are strictly followed. Regular observational audits on infection control procedures is performed in the haemodialysis units at our centre. This helps to maintain the ongoing training and implementation of corrective procedures. We did not find any BBV infections in patients (12.5%) who had undergone dialysis at other centres also. This can be attributed to the good infection control practices followed in those centres.
Detection of occult HBV infecton is dependent on the sensitvity of the molecular technique used, the presence of low viral loads, and the size of the populaton sample studied [18]. Molecular assay could detect 4 to 5 times more infection than the routine HbsAg tests in a North American urban dialysis centre. Only a highly sensitive molecular assay can detect low viral load infection. The mutations like type sG145R causes modificaton to antigenic determinant a and hence anti-HBs is unable to neutralise the virus. In a brazilian haemodialysis centre, prevalence of occult HBV was also low at 0.39% [19].
Absence of NAT positivity in the present study population could be due to the low prevalence of these infections in the population. The prevalence of HBV among blood donors in Southern India is very low (0.19%) classifying it as an area with low endemicity and the prevalence of occult hepatitis B Infection was also found to be very low at 0.017% [20]. The low sero-prevalence of HCV (0.01 to 1.4% [21,22] and HIV (0.2%-0.38%) [22] could have contributed to the all negative viral NAT result. Also, screening of blood products by NAT has reduced the transmission of infection through blood components.
Hence, a sensitive chemiluminescence assay can be continued as the screening test; negating the need to perform costly molecular tests like nucleic acid amplification testing before starting dialysis as well as at regular intervals in India.
Limitation
The study did not find any case of occult or window period infection for HIV, HBV or HCV as the sample size was small. Larger study is required to determine the utility of NAT as a screening assay for dialysis patients in low prevalence population.
Conclusion
Not a single case of occult or window period infection for BBV was identified in dialysis patients using NAT. Proper sterilisation protocols, separate machines for BBV positive patients, routine baseline tests, use of NAT screened blood components for transfusion, less percentage of patients undergoing dialysis outside the centre and low prevalence of infection are responsible for NAT negative test results. Chemiluminescence assay was found to be equally good as NAT in ruling out BBV infection in dialysis patients and is a cheaper alternative to NAT in preventing BBV transmission in this group of patients.
Author contributions: All the authors have accepted responsibility for the entire content of this submitted manuscript and approved submission.
Research funding: Intramural fund from Amrita Institute of Medical Sciences and Research Centre, Kochi, Kerala, India.