Insertion of NGT is a vital procedure for many surgeries related with abdomen and thorax. Although apparently a simple procedure, it turns into a challenging job when performed in the unconscious and paralysed patients because they cannot cooperate with the operator [1]. The distal portion with multiple apertures is the weakest part of the NGT. Thus, it is susceptible to kink or coil, mostly in the anatomical recesses such as pyriform sinus or oropharynx when it encounters some resistance in its journey through nasopharynx and laryngopharynx [1]. Consequently, the failure rate with conventional blind method of NGT insertion (head in neutral position, no external laryngeal manipulation) is nearly 50% on first attempt [2].
To overcome the difficulties of blind method mentioned above, many people have adopted different techniques such as ‘neck flexion with lateral pressure’ [3,4], ‘reverse Sellick’s manoeuvre’ [3,5], and ‘frozen NGT’ technique [6]- all of which achieved a success rate of above 80%. The use of GlideScope [7] or ‘King Vision’ video laryngoscope [8] was found to increase the success rate of correct NGT placement.
The flooding of literature with so many methods, modification of previous technique, frequent arrival of new technique- all suggest that none of the method is universally acceptable with high success rate and the quest for the best is still on. In paediatric patients, often anaesthesiologists are compelled to use uncuffed Endotracheal Tubes (ETT) owing to local unavailability of respective cuffed tube or for smooth insertion. In such case, throat pack (pharyngeal pack) is required to make a proper seal. Conventionally, NGT is inserted prior to placement of the throat pack with the belief that the NGT would be difficult to be placed after throat pack application.
In recent past, Walker R et al., is the first to mention that NGT insertion is possible even with prior presence of a throat pack which rather facilitates the process by preventing coiling of NGT in oropharynx [9]. But, there exists no further mention about the success rate of this method of NGT insertion. Hence, the present study was designed to evaluate primarily the success rates for NGT insertion using ‘throat pack in-situ’ technique in comparison with the conventional blind method in anaesthetised, intubated paediatric patients. In addition, the procedure time and incidence of adverse events were also observed.
Materials and Methods
After obtaining permission from Institute’s Ethics Committee, (Letter no. NMC/55, dated 05.01.2018, issued from IEC of NRS Medical College, West Bengal) this single-blind interventional study was carried out in the paediatric surgery operating room of a tertiary care centre (Government Medical College). It spanned over approximately one year, from July 2018 to June 2019.
A total of 140 children of American Society of Anesthesiologists (ASA) physical status I or II, aged 3-12 years, posted for elective abdominal surgeries under general anaesthesia and requiring NGT placement intraoperatively, were included for this interventional study. Children having nasal mass, significant deviated nasal septum, or adenoid were excluded from the study. Similarly, children having cleft lip, cleft palate, trachea-oesophageal fistula, oesophageal stricture or those having bleeding diatheses were excluded. Also, any children requiring NGT insertion in the pre-induction phase were excluded.
The legal guardian(s) were explained about the proposed procedure, the risk as well as the benefit associated with it in their own language and then written informed consents were obtained. They were also informed about their right to put out from the study at any time during the study.
In the operating room, an intravenous (iv) line was established with a 22-G or 24-G cannula. The children were anaesthetised and intubated as per standard protocol. For intubation uncuffed Polyvinyl Chloride (PVC) ETT (STERIMED® Medical Devices Pvt., Ltd., Bahadurgarh, Haryana, India) of appropriate size as per calculated tube size was used. Group allocation was performed after induction of anaesthesia and intubation. It was performed each time by opening the sequentially numbered and sealed opaque envelopes. There were 140 sealed envelopes each containing one piece of paper marked either ‘A or ‘B’ (70 papers marked as ‘A’ and another 70 papers marked as ‘B’). After the tracheal intubation an envelope was randomly selected and opened. The alphabet displayed (‘A’ or ‘B’) corresponded to the group allocation of the child. The children received their NGT placement either using conventional blind method (Group A, n=70) or ‘throat pack in-situ’ technique (Group B, n=70).
It was not possible to conceal the specific method to the anaesthesiologist who was performing the procedure. One senior anaesthesiologist performed all the procedures to minimise inter-personal variability of efficiency. Only the anaesthetised child was unaware of the particular method employed for the NGT placement. Thus, the study was a single-blind design. One dedicated anaesthesiologist acted as observer and data-keeper who was not involved otherwise with the procedure.
For both the groups the same brand of PVC made NGT (Size 10-12-French Gauge, length 105 cm, FLO-ON® Bhagawati Medicare Devices, Ahmedabad, Gujarat, India) was used. The tip of NGT was lubricated with lignocaine jelly. The specific method of NGT insertion (manipulation or movement) remained same in both the groups. The NGT was inserted through nasal route with head in neutral position without any external laryngeal manipulation or any instrumental assistance. No change of head position was allowed. The only difference between the methods of two groups was regarding the temporal sequence of NGT insertion in relation with throat pack application. In other words, whether the NGT placement was before (group A) or after (group B) the throat pack placement.
In Group A (applying conventional blind method), after endotracheal intubation as per standard protocol, the NGT was inserted. After confirmation of successful placement of NGT, the pharyngeal pack was applied.
In Group B (applying ‘throat pack in-situ’ technique), after endotracheal intubation, the throat-pack (pharyngeal pack) was applied in a non-tight condition so that it allowed a ‘palpable and audible leak’ at conventional inflation pressure of ventilation (20 cm H2O of inflation pressure). Then the NGT placement was done in the same manner as in the conventional group.
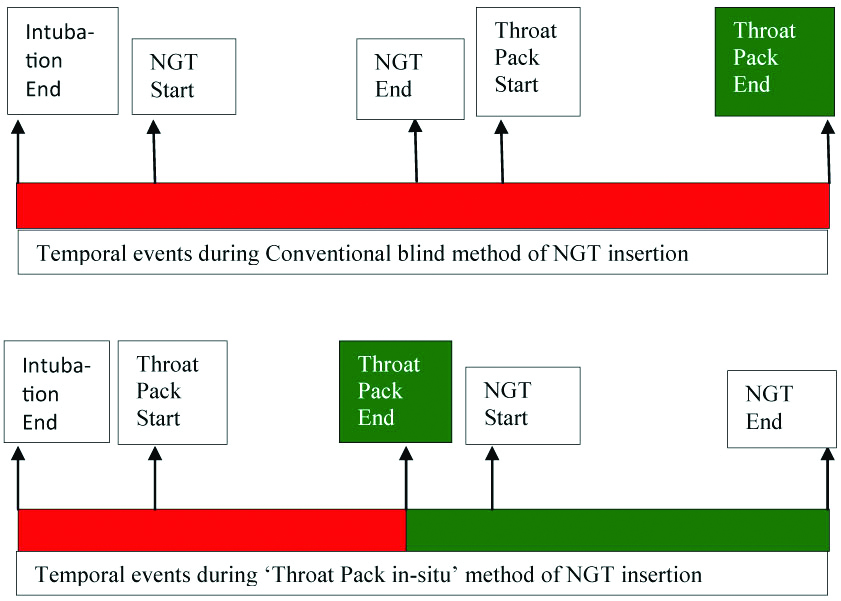
In both the groups, the NGT was held in such a way to maintain its curvature while being inserted into the nose, which curves inward the nasal passage. The appropriate length of NGT insertion was determined by measuring the distance from the selected nostril to ipsilateral tragus and then to the mid-point between xiphoid process and umbilicus [10]. It was gently advanced. If resistance was felt during first attempt, the NGT was withdrawn and reinserted. A finger was swapped inside the oral cavity, post-NGT insertion, to exclude any coiling of the tube. If the NGT was found to be coiled it was withdrawn to nasal cavity under gentle laryngoscopy and attempted once more. Correct NGT placement within two attempts was considered as ‘successful’ insertion. The procedure time was defined as the time from the start of NGT placement through the selected nostril up to the successful placement of the tube within two attempts. Confirmation of correct position was done by auscultation of a ‘whooshing’ sound over the epigastrium while injecting air through NGT with a 10-ml syringe. If both attempts were unsuccessful, it was considered as a failure. If the procedure failed, the anaesthesiologist was allowed to change the insertion technique to any at which he/she is comfortable with. The throat pack placement time was noted as the time from the start of pack placement and the completion of the pack application. The duration of major leak in fresh gas flow was calculated in each group according to the time gap from completion of intubation and completion of pack application [Table/Fig-1].
Comparative temporal view of different procedures in two groups.
The figure is not to the scale regarding time. The red colour indicates the time period of major (considerable) leakage of fresh gas in each group. The green colour indicates the saved time period of fresh gas flow leak in the new method i.e., the ‘throat pack in-situ’ technique. This saved time reflects the time needed for NGT placement plus any lag period for change over from one procedure to another
According to a previous article, the success rate of NGT placement is found to be 50% with the use of conventional blind technique within 1st attempt [2]. It was assumed that there would be 30% increase in the success rate of NGT insertion in 1st attempt over the conventional method using the novel method of Throat Pack in-situ Technique. A superiority margin in proportion was set at 0.1. Setting the power of the study at 80% and confidence limit at 95% (α=0.05; 5% level of significance), the calculated sample size became 63 for each group. Considering a dropout of 10%, the final sample size became 70 for each group.
Statistical Analysis
Data were entered into a Microsoft Excel spreadsheet and then analysed by SPSS (version 25.0; SPSS Inc., Chicago, IL, USA) and GraphPad Prism version 5. All continuous data (numerical variables) are presented in the tables as mean with standard deviation (SD) and have been tested using Student’s t-test. For categorical variables the data are presented as number of patients (proportions) and have been tested using Pearson Chi-square test and Fischer’s exact test as appropriate. The p-value <0.05 was considered as significant.
Results
The NGT insertion was not possible in four patients in the group A and in two patients in the group B. Hence, data regarding the procedure time was available from 66 patients in group A and 68 patients from group B according to the study protocol. Both the groups were comparable in terms of demographic profile [Table/Fig-2].
| Parameters | Group A (n=70) | Group B (n=70) | p-value |
|---|
| Age (years) | 6.30±2.27 | 6.53±2.57 | 0.578 |
| Weight (kg) | 19.19±6.15 | 19.59±6.61 | 0.711 |
| Height (cm) | 107.80±12.72 | 107.74±13.56 | 0.979 |
| BMI (kg/m2) | 16.16±2.49 | 16.45±2.48 | 0.482 |
| Sex (M/F)* | 56/14 | 51/19 | 0.319 |
| ASA PS (1/2)* | 64/6 | 59/11 | 0.195 |
| MP Grade (1/2)* | 62/8 | 65/5 | 0.382 |
Continuous data are expressed as mean±SD and have been tested using Student’s t-test; Categorical data are marked with * and tested using Pearson Chi-square test
In the first attempt, 56 out of 70 anaesthetised intubated paediatric patients (80%) had successful placement of NGT in Group A. For the remaining 14 patients, another attempt was required and there was success in the correct placement of NGT in further 10 patients. Hence, the overall success rate was found to be 94.3% (66 out of 70) using conventional blind method. In Group B (Throat pack in-situ method), 62 out of 70 anaesthetised intubated paediatric patients (88.6%) had successful placement of NGT in the first attempt. For the remaining eight patients, a second attempt was required and successful placement of NGT was possible in further six patients. Hence, the overall success rate was found to be around 97.1% (68 out of 70) using ‘throat pack in-situ’ method. On inter-group analysis of overall success rate (including second attempt), the difference between the two groups were not significant (p-value=0.404). Considerably, lesser time was required for placement of NGT using throat pack in-situ technique compared with conventional method [Table/Fig-3].
Success rate and procedure times of NGT placement.
| Parameters | Group A (n=70) | Group B (n=70) | p-value |
|---|
| Attempts |
| 1st | 56 | 62 | 0.373 |
| 2nd | 10 | 6 |
| Success rate |
| Overall success | 66 (94.3%) | 68 (97.1%) | 0.404 |
| Overall failure | 4 (5.7%) | 2 (2.9%) |
| Procedure times | Group A (n=66) | Group B (n=68) | |
| Procedure time (seconds) | 31.97±24.43 | 24.12±17.41 | 0.034 |
Test applied: Pearson chi-square test for number of attempts and success rate, student’s t-test for procedure times
Mean HR and mean value of MAP in both the groups were comparable before and after the procedure between the groups.
Bleeding emerged as the most common adverse event in both the groups occurring in 29% in Group A and 19% in Group B [Table/Fig-4].
| Adverse events | Group A (n=66) | Group B (n=68) | p-value |
|---|
| Bleeding | 19 (28.8%) | 13 (19.1%) | 0.189 |
| Coiling | 18 (27.3%) | 7 (10.3%) | 0.012* |
| Kinking | 5 (7.6%) | 5 (7.4%) | 0.961 |
| Uneventful | 43 (65.2%) | 53 (77.9%) | 0.101 |
Test applied: Pearson chi-square test; *statistically significant
The throat-pack placement time was found slightly more in Group A compared with Group B. The mean duration of major gas leak in Group A and Group B were 152.8±49.1 and 77.0±30.9 seconds, respectively, [Table/Fig-5].
Throat pack placement time and duration of fresh gas flow leak.
| Parameter | Group A (n=66) | Group B (n=70) | p-value |
|---|
| Throat pack placement time (in seconds) | 27.00±9.01 | 23.44±10.17 | 0.033 |
| Major leak time (in seconds) | 152.83±49.10 | 77.044±30.89 | <0.001 |
Test applied: Student’s t-test
Discussion
The present study shows a considerable high success rate (around 97% within two attempts) for correct placement of NGT in ‘throat pack in-situ’ group. This indicates that the throat pack does not put a hindrance to NGT placement. Comparable success rate and favourable adverse event profile taken together, it can be said that the pre-existing appropriately placed throat pack may facilitate the NGT insertion instead of putting hindrance. Throat pack application before the NGT placement actually obliterates the spacious oropharynx thereby eliminating one less resistant path i.e., the oropharynx where the NGT often deviates and coils. Thus the throat pack reduces the propensity of coiling and helps steering the NGT to its intended normal pathway.
In 2008, Walker R first reported that prior existence of a throat pack have facilitated the NGT insertion attempted later on [9]. He commented that the throat-pack prevents coiling and impaction against any of the more anterior structures and helps the NGT to turn through 180 degrees making the NGT’s natural curvature facing posterior.
One important finding of the present study is a higher success rate (94%) achieved with conventional blind technique for NGT insertion in paediatric age group in comparison with that in studies involving adult population where it was 69% [11] to 75% [3]. The possible explanation for this relatively higher proportion of successful NGT placement using conventional method in paediatric patients with respect to the adult population may be due to less spacious orophaynx, relatively large tongue and anteriorly placed high-up larynx in children. In the present study, although a comparatively higher success rate was achieved with ‘throat pack in-situ’ method for NGT placement, it appeared comparable with the success rate of the conventional group which is already high in the paediatric population.
In the present study, the ETT of the same brand was used. The outer diameters of the ETTs with the same internal diameter vary widely between manufacturers and between cuffed and uncuffed ETTs from the same manufacturer [12]. Similarly, the same brand of NGT was used in the current study to nullify the variability in stiffness of NGT between the two groups.
The present study was designed to test whether the pre-existing pack influences the success of NGT placement in any way. Study in adult population indicates that the NGT placement is hindered to some extent after inflation of ETT cuff [13]. Hence, the uncuffed ETT was selected for the present study to avoid any such influencing factors attributed from the cuff.
In the present study, children aged 3 to 12 years were recruited. Gastric acidity in children may not reach the adult levels until the age of two or three [14]. During the initial stage of planning of this study, we had the intention of confirming the correct placement of NGT with additional use of pH testing of gastric aspirate besides the whoosh test. Moreover, the NGT required for newborn and infant is quite soft owing to its smaller size and thickness. NGT requires some strength to be successfully inserted while the pharyngeal pack is already there and those small sized NGT intended for use of newborn and infant are too soft to provide that strength. Hence, exclusion of newborn and infant were done to reduce the wide variation of sizes of NGT.
In the present study, considerably higher time was required for throat pack placement in conventional group compared with ‘throat pack in situ’ technique. This might be due to the presence of two tubes (NGT and ETT) in the area where the pack was applied, thus hampering the process of pack placement. However, the times in both the groups were much shorter than the average pack application time in adult study where it was between 76 to 85 seconds [15]. This lesser time is probably attributed to the fact that pack size is smaller in paediatric population compared to adult patients.
The clinical consequences of gas leak depend on the lost volume. The patient may receive less than the desired anaesthetic concentration. Pollution with anaesthetic gases is another problem that can occur if the anaesthetic gas mixture leaks during surgery. In the present study, a considerable less gas leak time was found in throat pack in-situ technique versus conventional blind method (77 seconds vs 153 seconds). In other words, gas leak time was almost halved when throat pack was applied before the NGT insertion. This extra time was necessary in the conventional group due to the time required for the changeover from tube fixation to picking up of NGT, application of lubrication, and the procedure time regarding NGT placement by conventional method and preparing for pack placement with laryngoscope. To the horizon of our knowledge, no study has studied the feasibility of NGT insertion keeping the pre-applied throat pack in-situ and assessing any additional influence on leakage in fresh gas flow, in a single setting. Bradford KE et al., assessed the effect of mouth opening or throat pack placement in minimising the fresh gas flow leak around uncuffed ETT during mechanical ventilation [16]. They found that both the interventions (mouth opening, and throat pack application) are effective in minimising the leak, thereby improving the tidal ventilation. However, the magnitude of improvement in ventilation owing to pack application was found to be almost double that of due to mouth opening manoeuvre.
Limitation
The present study bears some limitations. First, confirmation of correct placement of NGT was done by simple auscultation method instead of X-ray or other newer techniques such as capnography or USG, owing to feasibility ground. Although it was contemplated to use pH testing as a second-line confirmation for correct placement of NGT, it could not be implemented on feasibility ground (local unavailability of pH paper). Second, softer variety of NGT made of polyurethane couldn’t be used owing to its unavailability at our institution during the study period. This probably has led to higher adverse events like bleeding in paediatric population with delicate nasopharyngeal mucosa. Although life-threatening serious adverse events such as oesophageal perforation, piriform fossa penetration and pneumothorax have not occurred, the possibility of such complications in this form of study cannot be ruled out. Third, cost analysis utilising in-depth mathematical model regarding the fresh gas leak and its impact on operating room pollution was not possible in our set-up. This would remain a future scope.
Conclusion
A higher success rate was observed even in the conventional blind technique for NGT insertion when compared with adult literature. The ‘throat pack in-situ’ method appeared comparable with conventional blind technique in respect with success rate. Lesser adverse events were observed with the use of ‘throat pack in-situ’ method. Considering the comparable success rate and lesser adverse events, the ‘throat pack in-situ’ method appears better alternative to the conventional blind technique for NGT placement in paediatric population where the use of uncuffed ETT with throat pack application is still prevalent. Moreover, the duration of fresh gas leak was found to be considerably less with the use of ‘throat-pack in-situ’ method.
Continuous data are expressed as mean±SD and have been tested using Student’s t-test; Categorical data are marked with * and tested using Pearson Chi-square test
Test applied: Pearson chi-square test for number of attempts and success rate, student’s t-test for procedure times
Test applied: Pearson chi-square test; *statistically significant
Test applied: Student’s t-test