Traumatic Spinal Cord Injury (TSI) is a devastating problem which is being faced by many young patients all over the globe. In India 10,000 new cases are added every year [1,2]. Majority of them are from 16-30 years age group [1]. These patients face multiple andrology related problems in terms of ED, anejaculation, anorgasmia and infertility [3].
There have been studies which emphasise the need to manage sexual dysfunction in such patients to treat them holistically [4]. In a literature review conducted by Sunilkumar MM et al., it was inferred that, further research on how men themselves view their sexual disabilities would go a long way in planning of adequate treatment and rehabilitation [4]. A systemic review by Deforge D et al., found the need to study the long-term sexual adjustment and holistic approaches in these patients [5]. Moreover, there is a lack of large scale studies, having long follow-up, regarding sexual functioning in spinal cord injuries in the Indian setting [6]. This study was hence conducted with an attempt to study the efficacy of various treatment options for ED and EJD in patients of TSI and compare the long-term outcomes in Indian setting.
Materials and Methods
A retrospective study of patients with TSI, admitted in The Paraplegic Foundation, Mumbai from September 2011 to August 2016 was conducted.
Hospital ethics committee approval was taken for the study (IEC/04/16). Included patients were those with age more than 18 years of age with lesion below T6 level. Patients permanently on catheter (not willing for CISC) and those not willing to participate in the study were excluded.
Demographic and andrological parameters of all these patients were noted. The records of patients before and after therapy were compared.
The Department of Urology of the study hospital takes care of urological and andrology related aspects of patients admitted in ‘The Paraplegic Foundation’, Mumbai which was established in 1968. It is a multidisciplinary team approach which consists of urologist, internist, psychiatrist, microbiologist, physiotherapist, nursing staff, and health care providers.
Total patients admitted at a time in the foundation are approximately 35. Around 30 were males and 5 were females. On an average, one patient stays for 6-9 months till complete rehabilitation. From urology perspective, all patients were evaluated for their symptoms and examined in detail. History about demographic parameters, mode of injury, duration, family issues, fertility status, and andrological aspects were considered in detail. History about andrological issues consists of details of libido, arousal, masturbatory or sexual or morning erections, rigidity and duration of erections, ability for penetration, orgasm and details of ejaculation. Relevant history was also considered from spouse. Psychiatrists were actively involved in this process. Patients were evaluated for American Spinal Injury Association Impairment Scale [7,8] for their sensory and motor functions. For ED, all patients were evaluated with IIEF-5 [9] score and classified as mild to severe ED depending on the scores. These records were maintained in the case files.
Majority of patients at the time of admission were on catheter which is present for variable amount of time before admission. Urinary infections were treated as per the cultures. Baseline evaluation was done in the form of ultrasound abdomen, post-void residue, and urodynamic testing whenever indicated. Gradually, patients were taught about Clean Intermittent Self-Catheterization (CISC) and motivated for getting off catheter. Once patient is off catheter, his treatment goals are decided for ED and/or EJD depending upon the willingness to father a child.
Those patients who wish to be treated for ED after proper counselling were started on treatment. Patients were started on Phosphodiesterase-5 inhibitors (PDE-5i): Tab Tadalafil 5 mg daily and 20 mg on demand 2 hours before the activity after ruling out necessary contraindications. Visual stimulation was used wherever required. If the patient fail on above treatment, second line treatment was considered, which consists of ICIVAD. Bimix solution (used for ICIVAD) consists of Injection papaverine 4 mL (30 mg/mL) plus Injection chlorpromazine 0.1 mL (0.625 mg/mL) [10]. The solution was injected starting from a minimum dose of 0.1 mL. The dose was titrated as per the requirement, upto a maximum of 1.0 mL under supervision. Patient and/or spouse were taught to administer the dose with 30G needle in corpora cavernosa [Table/Fig-1]. Motivated patients were also encouraged for homeself-injections. Contraindications like uncontrolled coagulopathy, unstable cardiovascular disease, and psychogenic instability were ruled out before administering ICIVAD. Patients were explained about risk of priapism, and the possibility of emergent treatment in the emergency department, if it occurs. Along with these treatment options, motivated patients were also offered VED and taught about the necessary precautions during the use. Penile implants were not offered to our patients in this center as there are multiple risk factors for complications and extrusions, in the form of sensory loss, local infections and need for CISC. For EJD, treatments offered are PVS using a vibrator or EEJ using Saegar’s model (Dalzell USA Medical Systems, Dungannon, Northern Ireland). Inexpensive models of vibrators are used which have similar frequency of 110 Hz and 2.5 mm amplitude [Table/Fig-2]. Cycles of stimulation of 3-5 min followed by rest for 2 min are repeated for a maximum of 1 hour. For those who do not respond to vibrator therapy, EEJ was performed under anaesthesia with progressively increasing voltage from 5 V to 25 V with a current of 100-600 mA in intermittent manner. Non-catheterized sample of semen was collected for cryopreservation.
Technique of Intracavernosal Injection of Vasoactive Drug (ICIVAD).

Low cost vibrator used for PVS.

Results
Out of 167 patient records assessed during this study period, 110 met the inclusion criteria.
The demographic data of these patients is shown in [Table/Fig-3]. The mean age was 34 years with standard deviation of 9.39 years. The details of spinal cord injuries are given in [Table/Fig-4]. Severe and moderate ED was present in 50.9% and 30.9% patients. Mild to moderate and mild ED was present in 12.7% and 5.4% patients, respectively. The mean IIEF-5 score of the total population was 8.53 [Table/Fig-5].
Demographic data of patients.
| Parameter | | Total population | Study population |
|---|
| Age group | 20-30 years | 47 | 40 |
| 30-40 years | 33 | 22 |
| 40-50 years | 23 | 11 |
| 50-60 years | 7 | 1 |
| Marital status | Married with completed family | 50 | 21 |
| Married with family not complete | 16 | 13 |
| Unmarried | 44 | 40 |
| Educational status | Primary education | 68 | 43 |
| Secondary education | 23 | 14 |
| Higher secondary education | 18 | 16 |
| Graduate and above | 1 | 1 |
Details of spinal cord injury.
| Parameter | | Total population | Study population |
|---|
| Cause of Injury | RTA | 77 | 52 |
| Fall from height | 19 | 15 |
| Assault | 13 | 7 |
| Miscellaneous | 1 | 0 |
| Injury level | T6-T7 | 3 | 2 |
| T7-T8 | 4 | 4 |
| T8-T9 | 7 | 3 |
| T9-T10 | 12 | 9 |
| T10-T11 | 16 | 11 |
| T11-T12 | 27 | 19 |
| T12-L1 | 23 | 15 |
| L1-L2 | 11 | 7 |
| L2-L3 and lower | 7 | 4 |
| ASIA impairment scale | A | 31 | 18 |
| B | 42 | 31 |
| C | 27 | 19 |
| D | 9 | 6 |
| E | 1 | 0 |
IIEF-5 scores in each category.
| IIEF-5 Category | Total population | Study population |
|---|
| Scores before therapy | Scores after therapy |
|---|
| No ED (22-25) | 0 | 0 | 1 |
| Mild ED (17-21) | 6 | 1 | 5 |
| Mild to moderate ED (12-16) | 14 | 9 | 17 |
| Moderate ED (8-11) | 34 | 25 | 33 |
| Severe ED (5-7) | 56 | 39 | 18 |
After complete counseling and evaluations, patients motivated for treatment of ED were 74 out of 110 (67%). The mean age group of these patients was 31.3 years with a standard deviation of 7.8 years. The mean IIEF-5 score before therapy in these patients was 8. Sixteen out of 110 (14.5%) patients were concerned about treatment of anejaculation.
All 74 patients of ED were started on treatment but only 58 of them were compliant for the same. They were on 5 mg Tadalafil once a day with on-demand use of 10 mg or 20 mg as per the effect. Forty two out of 58 (72.4%) had satisfactory erections with PDE-5 inhibitors. Thirteen (22.4%) of them could have successful ejaculation. Certain patients had side effects in the form of body aches. No visual problems occurred in them.
Five out of 16 patients who were not satisfied with PDE-5i therapy and 7 out 16 who were not compliant for PDE-5i therapy (i.e., a total of 12 patients) opted for ICIVAD [Table/Fig-6]. They were continued on PDE-5 inhibitors along with injections as and when required. Average time for full erection was 15 minutes and average dose required was 0.2cc Bimix. Ten of 12 (83.3%) had penetrable erections. Six (50%) had successful ejaculations. Though a small number, overall response was poor with lumbosacral lesions as compared to higher lesions. Three patients were on home self-injections. Ten out of these patients were satisfied with the outcome.
Flowchart showing type of therapy given to patients of ED.
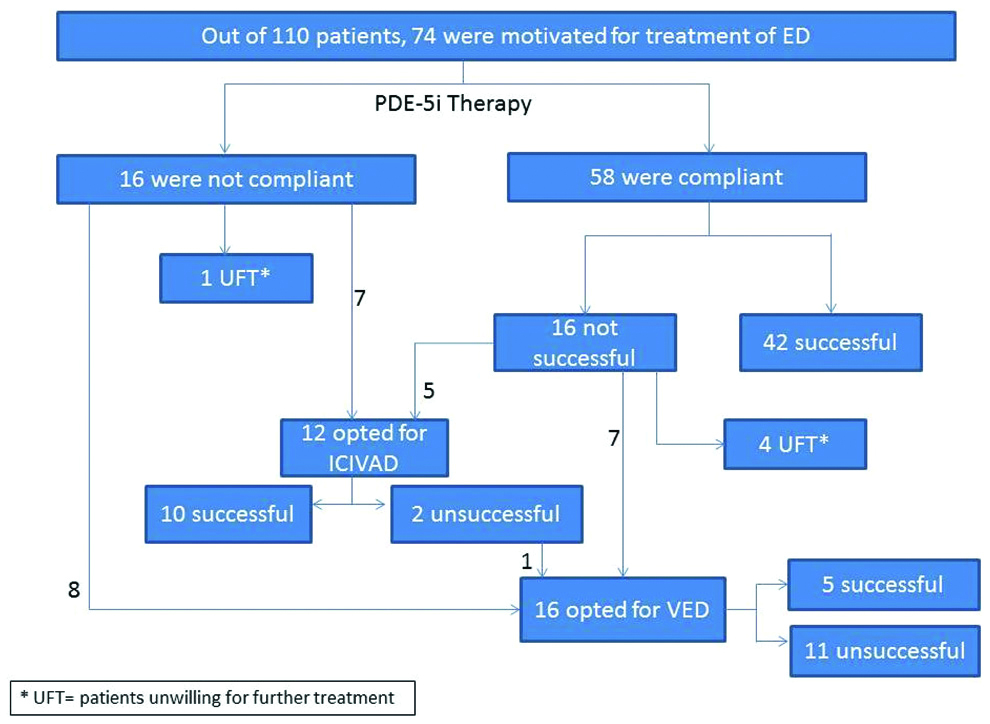
Another 7 out of the patients not successful after PDE-5i, 8 of those not compliant on oral drugs along with a patient not satisfied after ICIVAD (i.e., a total of 16 patients) opted for VED with PDE-5i or ICIVAD. Five of these patients deemed their erections to be satisfactory.
The mean follow-up was 4.6 years. (Maximum follow-up: 7.5 years, Minimum follow-up: 3.8 years).
The mean IIEF-5 score as a result of the combined therapy was 12.3, as compared to 8 before starting therapy (p<0.01) [Table/Fig-5]. Out of all patients treated for ED, a total of 57 patients (77%) had an erection which they considered satisfactory.
Total 16 patients who were concerned about EJD had penile vibratory stimulations. Five of which could have ejaculation. They were asked to go ahead with IUI (Intra-uterine Insemination) if the semen parameters were appropriate. Only one patient out of those not successful on PVS, opted for EEJ. It was done in an in-patient setting, under anesthesia. The semen sample obtained after EEJ was found to have oligozoospermia. None of the patients were affording for ICSI or cryopreservation. Though few of them tried for IUI, none had successful pregnancy as the outcome.
Discussion
An improvement of IIEF-5 score from 8 to 12.3 (p<0.01) was observed in the study; 77% of patients treated for ED had an erection which was deemed satisfactory by them. Biering-Sørensen I et al., conducted a similar study in which 78-94% of men with TSI had positive effects of penile vibration, drugs and intracavernous injection for erection [11]. Similarly, Del Popolo G et al., reported an improvement of mean IIEF scores of 3.5 to 6.6 in patients treated by PDE-5i for ED [12]. This is in concordance with the improvement in the mean IIEF-5 scores in this study.
Guttman L have described three phases for erectile functions after spinal injury in the form of spinal shock, reflex return and readjustment [13]. In the shock phase, there may not be any erections, in second phase there is reflex return of functions and the final phase depends majorly on the pre-injury functions and rehabilitation. After injury, reflexogenic erections can occur after cutaneous stimulation below the level of lesion which requires intact sacral reflex arc. Psychogenic erections can occur because of audio-visual stimuli [14]. Few authors consider that patients with incomplete injury are better for assessment of erectile functions than complete lesions [15]. Correlation has also been established for the spinal level of lesion and the erectile function. It has been reported that higher lesions with intact local parasympathetic arc have better function as compared to lower lesions with damaged sacral arc [16]. Although it has also been mentioned that level and completeness of lesion has no effect on sexual outcomes after TSI [17]. Overall ability of erection varies from 54% to 95% and ability for successful coitus varies from 5% to 75% [18].
It has been studied that the effect of PDE-5 inhibitors is more if there is a sparing of sacral or thoracolumbar segments in cases with spinal injury [19]. Word of caution for the patients who are on PDE-5 inhibitors is to avoid nitrates for the treatment of autonomic dysreflexia which can occur in them. Virag R introduced intracavernosal injection of vasoactive agent (papaverine) for the first time in 1982 [20]. After that multiple agents have been used. We prefer a combination of Papaverine and chlorpromazine [10]. It is a cost effective alternative of prostaglandins in developing countries without any specific side effects. The site of injection should be alternate on both corpora on lateral aspect to avoid chances of fibrosis [21]. Overall the treatment response to oral or intracavernosal agents is better in these patients due to the fact that they have predominantly neurological ED with intact healthy vascularity maintained in cavernosal tissues [21]. Penile implants have been tried in past in TSI patients for reasons of erection, ease of CISC and ease of condom type catheter application [22,23]. Multiple series report against use of implants in these patients with higher rates of erosion or extrusion in the range of 10-25% [24]. Because of lack of sensation, there is delay in identification and salvage of implant related infective complications [25].
PVS as the modality for ejaculation was demonstrated by Sobrero AJ et al., [26]. PVS action depends on the integrity of dorsal penile nerve and sacral reflex arc. Authors have mentioned that intactness of bulbocavernous reflex (S2-S4) [27] or hip flexion reflex (L2-S1) [28] predicts favourable response to PVS. The vibrator which we use is an inexpensive variety of the standard one and has good outcomes in our small set of patients. EEJ was first time demonstrated in 1931 by Learmonth JR, and modification was introduced in 1987 by Halstead LS et al., [29,30]. Various precautions during EEJ have been standardised in the form of catheterisation before procedure, check anoscopy before and after the procedure, catheterised or non-catheterised collection of sample with preservative medium (Ham’s F 10). Interrupted current delivery is considered to be better than continuous one for obtaining good numbers and quality [31]. It has been reported that EEJ is useful for obtaining ejaculation in patients with all types of SCI in spite of loss of ejaculatory reflex arc [32]. Authors have demonstrated rates of 80% to 100% for induction of ejaculation with EEJ in spinal cord injured patients [33].
In spite of positive results in terms of ejaculation with the use of different modalities, overall semen parameters in these patients are of poor quality; aetiology of which is multifactorial [34]. Testicular function is abnormal because of abnormal HPG axis and testicular fibrosis leading to maturation arrest. Epididymal and testicular hypofunction occurs because of increased temperature. Seminal content also has high reactive oxygen species, leukocytes, inhibitory cytokines and structural defects in sperms. A study reported that inactivation of the inhibitory cytokines (IL-6, IL 1 beta, TNF alpha) by monoclonal antibodies enhances sperm motility [35]. Basic research for improvement of all parameters in paraplegic patient is on-going throughout the globe. Neuro-prostheses are also tried which are the devices that use electrodes to interact with neurological system for restoration of function especially in SCI patients [36]. Although in the experimental stage, these experiments can be the future for paraplegic patients. A meta-analysis mentioned that stem cell therapy for cavernous injured rats increases intra-cavernosal pressures and prove the validity and safety of stem cells for neurological ED in rat model [37]. We considered this project as a part of complete rehabilitation of our patients from “Paraplegic foundation.”
Limitation
Although overall sample size in this study was small, the patients had significant improvement in different aspects of sexuality. The study was retrospective in nature with a small sample size, especially those patients who were treated for EJD were less.
Conclusion
A step-by-step approach of oral PDE-5i therapy, ICIVAD and VED is adequate to manage ED in a majority of patients with SCI. Similarly, PVS and EEJ can be used for management of EJD in these patients. These modalities are efficacious as well as cost-effective for long-term management of these patients in Indian settings.