Mycobacterium Tuberculosis and Mycobacterium Leprae Co-infection: A Case Report
Bimal K Agrawal1, Saurabh Marwaha2, Manu Mathew3
1 Professor, Department of Medicine, M M Institute of Medical Sciences and Research, Maharishi Markandeshwar (Deemed to be University), Haryana, India.
2 Assistant Professor, Department of Medicine, M M Institute of Medical Sciences and Research, Maharishi Markandeshwar (Deemed to be University), Haryana, India.
3 Junior Resident, Department of Medicine, M M Institute of Medical Sciences and Research, Maharishi Markandeshwar (Deemed to be University), Haryana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Bimal K Agrawal, Professor, Department of Medicine, M M Institute of Medical Sciences and Research, Maharishi Markandeshwar (Deemed to be University), Haryana-133207, India.
E-mail: onlybimal@gmail.com
Tuberculosis (TB) is one of the oldest diseases known to affect man caused by bacteria of the Mycobacterium tuberculosis complex. World Health Organisation (WHO) estimate shows that 10.4 million new cases of tuberculosis occurred worldwide in 2016. Likewise, leprosy is another age-old disease caused by Mycobacterium leprae. Leprosy is predominantly a disease seen in the developing world with a worldwide estimation of 0.6 to 8 million affected individuals. Both are chronic diseases, prevalent in various parts of the world and account for significant disease morbidity. Co-infection of the two Mycobacteria, although rare, has been reported to occur. Here the present authors discuss one such case of co-infection with both Mycobacteriae. A 24-year-old male was presented with fever, cutaneous lesion and cough. The clinical diagnosis of leprosy was made and chest X-ray was suggestive of tuberculosis. After confirming the diagnosis, the patient was treated with four antitubercular drugs as per the guidelines along with dapsone and clofazimine. The patient gradually improved and after six months treatment was continued only for leprosy.
Cough, Fever, Macular lesions
Case Report
A 24-year-old male patient reported with a history of fever for 15 days. Fever was moderate in grade, on and off and more in the evenings. It was associated with cough with scanty white mucoid expectoration. Patient also provide the history of swelling of bilateral upper eyelids and eyebrows and hyperpigmented macular lesions over bilateral upper and lower limbs, which the patient had noticed when one of his friends showed them to him. The patient’s father had pulmonary tuberculosis 4 years back.
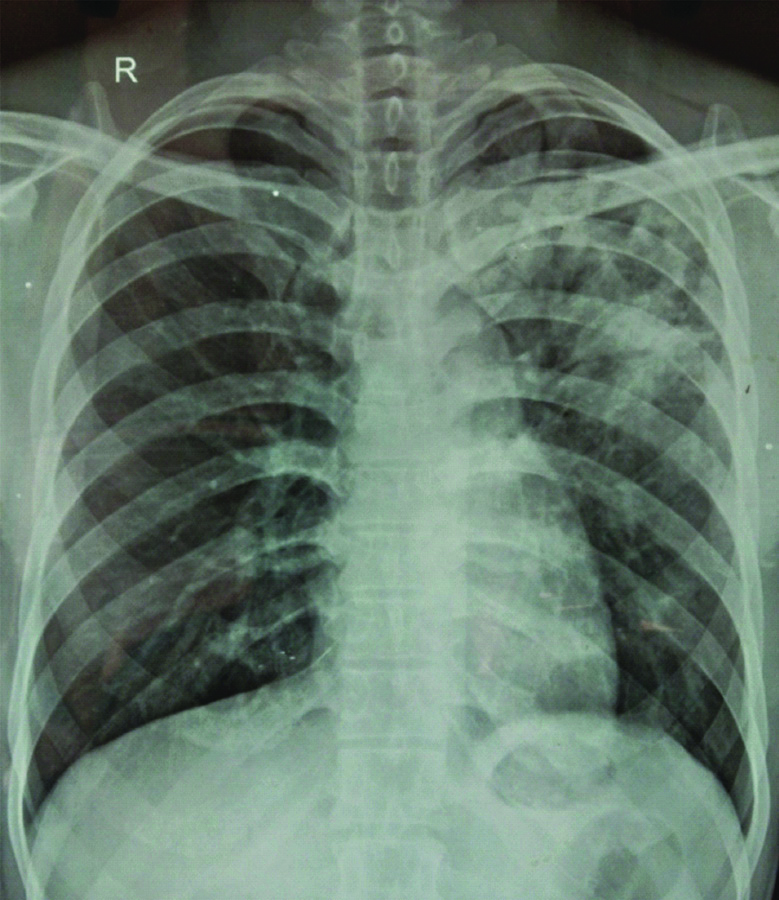
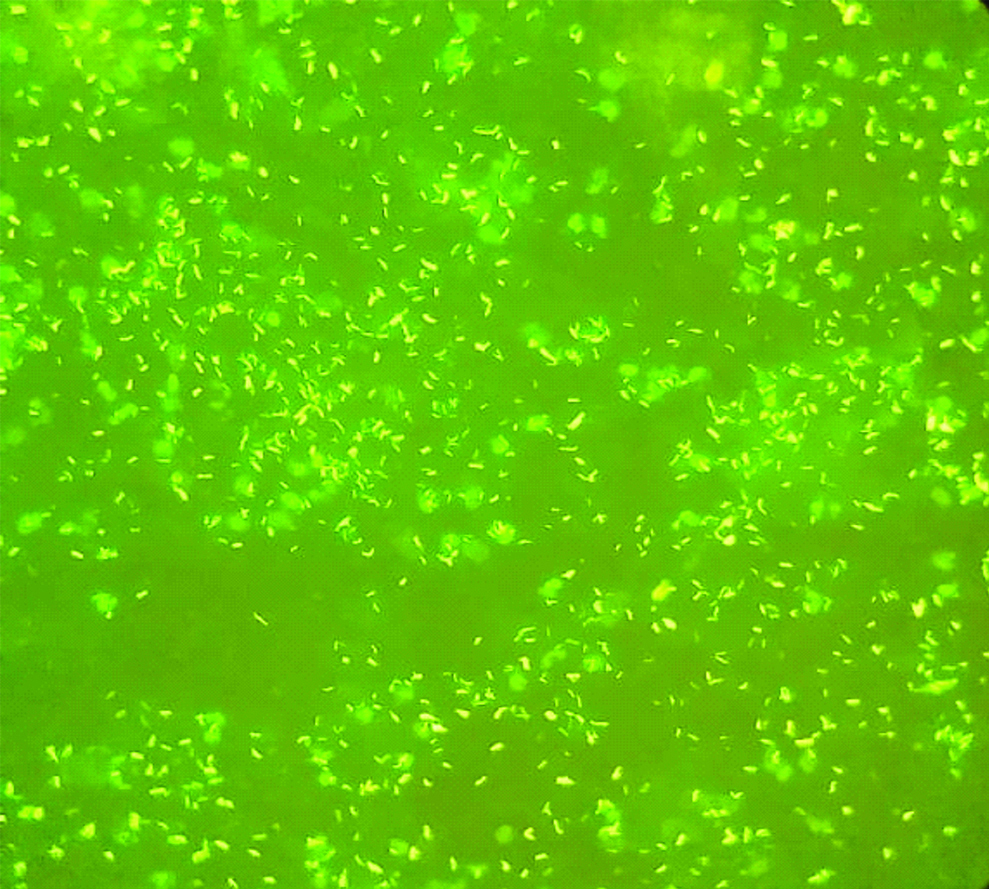
On examination, bilateral pinnae showed lobulations [Table/Fig-1], bilateral ulnar nerves were thickened and hyperpigmented and hypopigmented macular lesions in upper limbs [Table/Fig-2]. Impaired hot and cold sensations were observed using hot and cold water in a test tube. Chest X-ray showed an inhomogeneous opacity in the left upper and middle zones [Table/Fig-3]. Slit skin smear from ear lobule with Ziehl Neelsen staining showed the presence of acid-fast bacilli indicative of multi-bacillary leprosy. Sputum for tuberculosis bacilli was positive as seen by auramine staining [Table/Fig-4]. Later on, tuberculosis was confirmed by Cartridge Based Nucleic Acid Amplification Test (CBNAAT) testing which also showed sensitivity to rifampicin.

Hyperpigmented macular lesions.

Inhomogeneous opacity on chest X-ray.
Sputum smear showing tuberculous bacilli stained using Auramine stain (40X).
The patient was started on antitubercular treatment under directly observed treatment short-course regimen as per Revised National Tuberculosis Control Program (RNTCP) guidelines. The patient was on isoniazid, rifampicin, pyrazinamide and ethambutol (RHZE). For leprosy clofazimne 300 mg per month was given under supervision followed by 50 mg/day along with dapsone 100 mg daily.
The patient was followed-up regularly. After two months the tuberculosis regimen was changed to RHE for four months. The cutaneous and pulmonary lesions had resolved on subsequent follow-up. The patient was reviewed at monthly interval for six months. The repeat chest radiograph had shown resolution. The antitubercular treatment was stopped and the patient was advised to continue multidrug therapy for leprosy from the nearest primary health centre.
Discussion
Tuberculosis and leprosy have similar endemicity geographically [1,2]. The interactions between tuberculosis and leprosy and its effects on each other’s incidence are still a matter of debate [3]. The occurrence of both mycobacteria has been reported since long in the literature [4,5]. Moreover, postmortem studies had previously shown the high incidence of tuberculosis to be the cause of death in patients of leprosy [6,7]. Overall, these studies were of the view that leprosy predisposes to TB, especially the anergic form of leprosy.
Donoghue HD et al., using polymerase chain reaction, demonstrated the presence of wide-spread M. leprae and M. tuberculosis co-infection in human archaeological samples from the Roman period [8]. Their point of view was that the impaired cell-mediated response to the lepra bacilli in lepromatous leprosy patients would enable the advancement of the more virulent tubercle bacilli. However, as a result of cross-immunity, those individuals who acquired immunity against M. leprae would be less prone to pulmonary tuberculosis than the population in general, however, reverse would depend according to patient’s immune status, i.e., the hyperergic and not the anergic form of leprosy would offer protection [9]. Since then authors have conflict of thoughts with such hypotheses. One of the recent reviews concludes that co-infection is more likely to occur in borderline and lepromatous leprosy [5]. The index patient had multibacillary leprosy. Continued occurrence of such co-infection assumes significance since there is a global and national drive to eliminate leprosy and tuberculosis [10,11].
Because of co-infection, treatment of such cases remains a challenge. It has been advised to always rule out TB before starting treatment for leprosy. Interferon-Gamma Release Assays (IGRAs), sputum culture, chest radiograph help in diagnosing co-infection. Although false IGRA positive cases may occur but it should not be ignored and other investigations should be done to confirm or exclude the co-infection. As of now, cases of leprosy with co-infection of TB if undetermined and put on monthly rifampicin would carry a severe risk of developing drug resistance. As per WHO guidelines patients who cannot be started on rifampicin or till such time that patient is being worked up for TB, minocycline should be given as 100 mg daily [5]. Once TB is diagnosed, patient may be started on RHZE with dapsone.
Conclusion
Tuberculosis and leprosy to a lesser extent remain major public health problems. Both can cause a significant burden to the patient as well as the community as a whole. Any patient diagnosed with leprosy needs to be carefully evaluated for the presence of tuberculosis and vice versa.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 21, 2019
Manual Googling: Nov 07, 2019
iThenticate Software: Nov 15, 2019 (14%)
[1]. World Health Organization. World health statistics 2016: monitoring health for the SDGs sustainable development goals. World Health Organization; 2016 Jun 8 [Google Scholar]
[2]. World Health Organization. Global Leprosy Strategy 2016-2020: accelerating towards a leprosy-free world: Monitoring and Evaluation Guide [Google Scholar]
[3]. Rao GR, Sandhya S, Sridevi M, Amareswar A, Narayana BL, Lupus vulgaris and borderline tuberculoid leprosy: An interesting co-occurrenceIndian Journal of Dermatology, Venereology, and Leprology 2011 77(1):11110.4103/0378-6323.7499721220903 [Google Scholar] [CrossRef] [PubMed]
[4]. Kumar B, Kaur S, Kataria S, Roy SN, Concomitant occurrence of leprosy and tuberculosis-a clinical, bacteriological and radiological evaluationLeprosy in India 1982 54(4):671-76. [Google Scholar]
[5]. Mangum L, Kilpatrick D, Stryjewska B, Sampath R, Tuberculosis and leprosy co-infection: a perspective on diagnosis and treatmentInOpen Forum Infectious Diseases 2018 5(7)USOxford University Press:13310.1093/ofid/ofy13330046638 [Google Scholar] [CrossRef] [PubMed]
[6]. Premnath M, Ramu G, The association of tuberculosis and leprosyJ Indian Med Assoc 1976 67:143-45. [Google Scholar]
[7]. Gray HH, Bancroft H, Tuberculosis at the United States Public Health Service Hospital, Carville, Louisiana, 1922-1950International Journal of Leprosy 1952 20(4, Pt. 1):467-78. [Google Scholar]
[8]. Donoghue HD, Marcsik A, Matheson C, Vernon K, Nuorala E, Molto JE, Co-infection of Mycobacterium tuberculosis and Mycobacterium leprae in human archaeological samples: a possible explanation for the historical decline of leprosyProceedings of the Royal Society B: Biological Sciences 2005 272(1561):389-94.10.1098/rspb.2004.296615734693 [Google Scholar] [CrossRef] [PubMed]
[9]. Chaussinand R, Tuberculosis and leprosy, antagonist diseases. Prevention of leprosy by tuberculosisInt J Lepr 1948 16:431-38. [Google Scholar]
[10]. Blok DJ, De Vlas SJ, Richardus JH, Global elimination of leprosy by 2020: are we on track?Parasites & vectors 2015 8(1):54810.1186/s13071-015-1143-426490878 [Google Scholar] [CrossRef] [PubMed]
[11]. Pai M, Bhaumik S, Bhuyan SS, India’s plan to eliminate tuberculosis by 2025: converting rhetoric into realityBMJ Global Health 2017 2:e00032610.1136/bmjgh-2017-00032628589035 [Google Scholar] [CrossRef] [PubMed]