Apexification as a Clinical Strategy for the Management of an Immature Non-Vital Tooth with Buccal Bone Loss: A Case Report
Helder Fernandes De Oliveira1, Vinícius Caixeta De Sousa2, Alexandre Leite Carvalho3, Brunno Santos De Freitas Silva4, Orlando Aguirre Guedes5
1 Department of Endondontics, University of Anápolis, Anápolis, Goiás, Brazil.
2 Department of Stomatologic Sciences, Federal University of Goiás, Goiânia, Goiás, Brazil.
3 Department of Stomatologic Sciences, Federal University of Goiás, Goiânia, Goiás, Brazil.
4 Department of Endondontics, University of Anápolis, Anápolis, Goiás, Brazil.
5 Department of Endondontics, University of Anápolis, Anápolis, Goiás, Brazil.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Helder Fernandes de Oliveira, Av. Universitária Km 3,5, Bloco C-Sala 408, Cidade Universitária, CEP: 75083-515., Anápolis, Goiás, Brazil.
E-mail: helfo22@gmail.com
Endodontic treatment of immature non-vital teeth poses a considerable challenge. Its goals should include the control of intracanal infection and the promotion of continuous root development. This case report describes an apexification as an alternative strategy for the maintenance of a tooth with incomplete root formation. An 11-year-old female presented with a history of pain and discomfort on the left side of the mandibular region. Intraoral examination revealed the presence of a draining sinus tract located in the buccal mucosa, next to tooth 35, for which a cold test was negative. Periapical radiographs revealed a single-rooted tooth with incomplete root formation and a periapical lesion. A diagnosis of periapical abscess with fistula was made, and a root canal treatment in conjunction with apexification was planned. Cone Beam Computed Tomography (CBCT) imaging was performed which revealed resorption on the buccal side of the root and the destruction of the buccal cortical bone. After six appointments, the intraoral sinus tract had healed, no purulent discharge was observed, and the root apex was closed. The root canal was filled, and the tooth was restored. The three years follow-up examination showed adequate bone repair and the absence of periapical lesion. Apexification shows favourable results for the management of immature non-vital teeth.
Calcium hydroxide, Open apex, Root canal therapy
Case Report
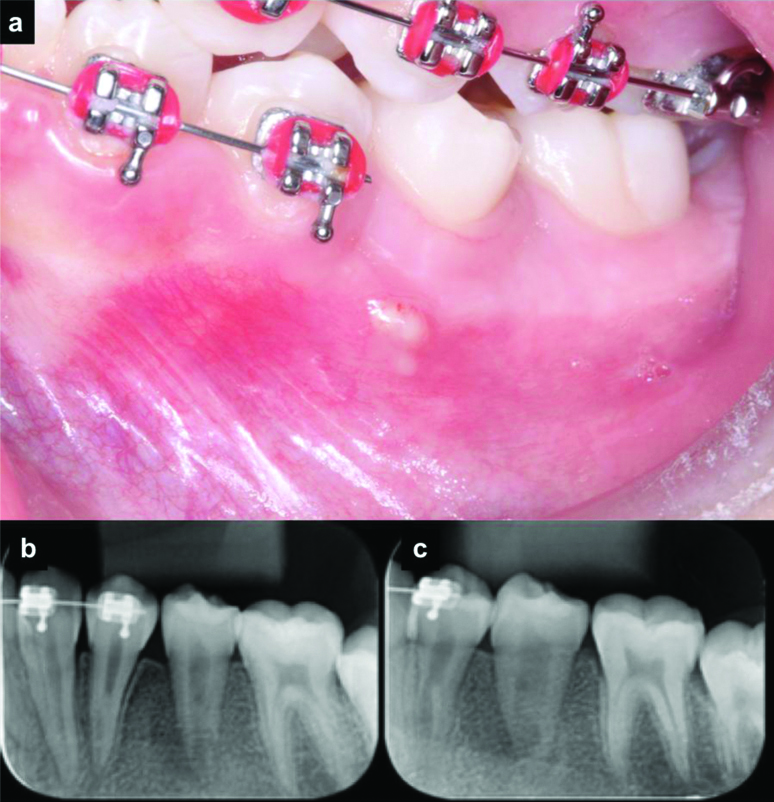
An 11-year-old female presented with the complaint of discomfort on the left side of the mouth for the past two months. Her medical history was non-contributory. The patient was under fixed orthodontic treatment. Her orthodontist removed the brackets from teeth 35 and 36 after observing the presence of a draining sinus tract located in the buccal mucosa, next to tooth 35 [Table/Fig-1a]. Intraoral examination revealed no signs of caries or existing restoration on teeth 34, 35 and 36. Cold test was performed an using a cold spray (Endo-Frost; Roeko, Langeman, Germany). The result of the test was negative for tooth 35. Radiographs revealed a mandibular premolar with incomplete root formation and a radiolucent periapical lesion [Table/Fig-1b,c].
a) Presence of fistula in the tooth 35 region; b,c) intraoral periapical radiographs of the tooth 35 region indicating the presence of incomplete root formation and periapical bone rarefaction.
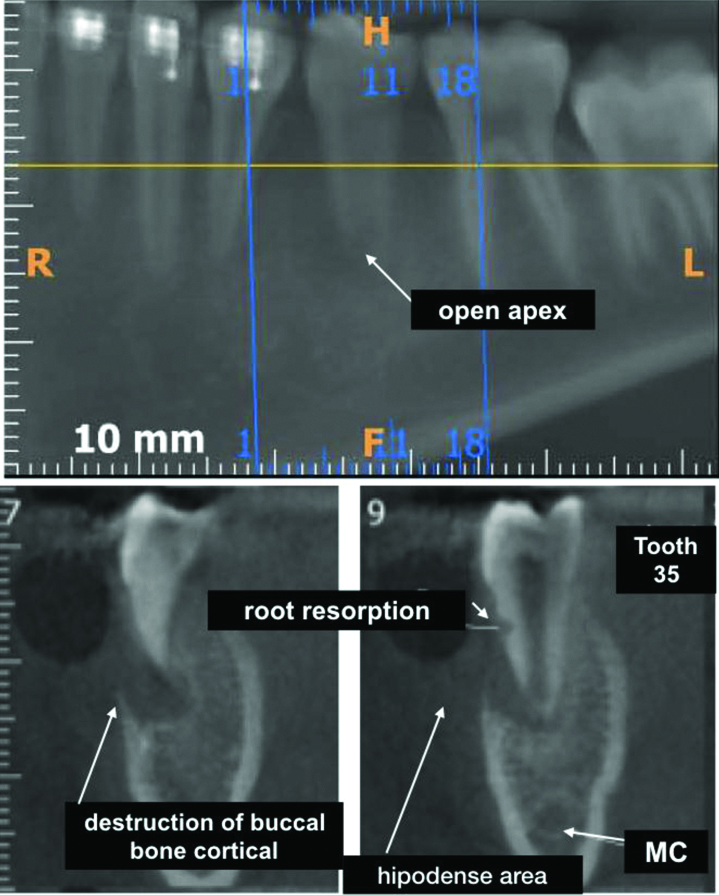
CBCT imaging was performed to better plan the case. CBCT images revealed resorption on the buccal side of the root and the destruction of the buccal cortical bone [Table/Fig-2]. The diagnosis of periapical abscess with fistula was made, and root canal treatment in conjunction with apexification was planned.
CBCT images showing open apex, root resorption and destruction of buccal bone cortical (arrows).
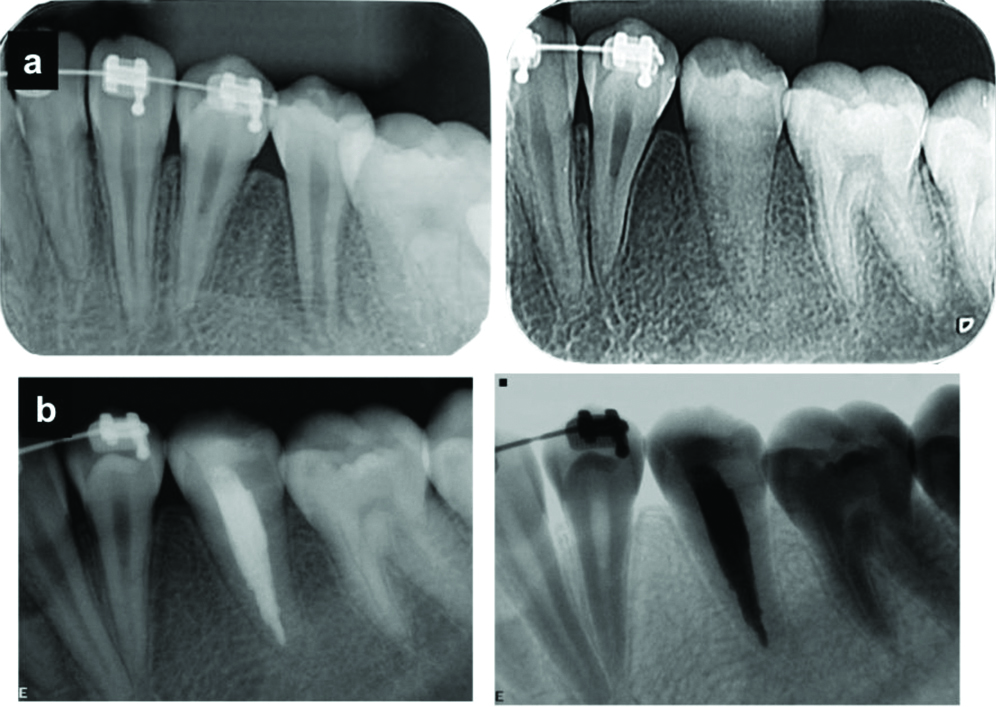
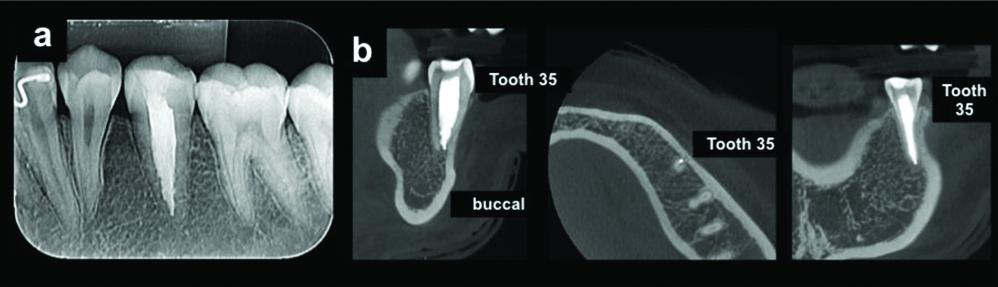
The tooth was anaesthetised and isolated with rubber dam and the pulp chamber was accessed using round diamond burs (#1011 and #1012, KG Sorensen, Barueri, SP, Brazil) and an Endo Z drill (Dentsply Maillefer, Ballaigues, Switzerland). The root canal was explored using a #15 K-file instrument (Dentsply Maillefer), and the cervical and middle thirds were enlarged using Gates-Glidden #2-3 and Largo #2 drills (Dentsply Maillefer). The Working Length (WL) was established based on the radiograph and K-file instrument. The apical third was prepared until the #60 K-file. During root canal preparation, the canal was irrigated with 2.5% sodium hypochlorite (NaOCl; Fitofarma, Goiânia, GO, Brazil), and after its completion, the canals were irrigated with 3 mL of 17% EDTA (Biodinâmica, Ibiporã, PR, Brazil). The EDTA was passively activated for 60 seconds using an EMS PM 200 ultrasonic unit (EMS- Electro Medical Systems S. A., Nyon, Switzerland) and an E1- Irrisonic tip (HELSE Capelli e Fabris Ind., Santa Rosa do Viterbo, SP, Brazil) positioned 1 mm short of the WL. The ultrasonic unit was set to 10% power. Finally, the root canal was again irrigated with 2.5% NaOCl, dried with paper points (Dentsply Maillefer), and medicated with calcium hydroxide (Biodinâmica, Ibiporã, PR, Brazil). The tooth was restored with glass ionomer cement (SS White, Rio de Janeiro, RJ, Brazil). Eight weeks later, the intraoral sinus tract had healed, and no purulent discharge was observed. Five additional appointments were performed at two-month intervals to change the intracanal medication. After 12 months, root closure was observed [Table/Fig-3a]. The root canal was filled with gutta-percha and Sealapex sealer (Sybron Endo, Glendora, CA, USA) using the lateral compaction technique. The access cavities were restored with a bulk-fill resin-based composite (3M-Espe, St Paul, MN, USA), and a final radiograph was taken to establish obturation quality [Table/Fig-3b]. The root resorption was treated by discontinuing orthodontic treatment and subsequent posterior endodontic intervention. Radiographic and CBCT follow-up examinations, performed after 3 years, showed adequate bone repair and the absence of periapical lesions [Table/Fig-4a,b].
a) Complete apex closure after intracanal medication with calcium hydroxide exchanges; b) intraoral periapical radiographs of tooth 35 after root canal filling showing adequate bone repair and absence of periapical lesions.
a) Radiographic and b) CBCT follow-up examination, performed after 3 years, of tooth 35 showing adequate bone repair and absence of periapical lesions.
Discussion
The endodontic treatment of teeth with incomplete root formation represents a significant challenge [1-4]. Clinical success and the maintenance of the affected tooth are essential factors to be analysed when choosing the best therapeutic option [3]. The possible fracture of the dentinal wall or the extravasation of the obturator material to the periapical tissue during the filling of the root canal are risks to be considered [3].
Apexification is the most classical technique and induces the formation of a mineralised tissue barrier in a root with an open apex or the continuous apical development of incomplete roots in teeth with necrotic pulp. The success of this therapy is related to a precise diagnosis and the complete understanding of the involved biological process [2]. During revascularization, after a disinfection technique, bleeding is stimulated in the periapical tissues, and a blood clot is formed within the canal, which supposedly contributes to structure growth and may produce stem cells that support the growth of tissues in the canal space and the continuous formation of roots [5]. Jeeruphan T et al., observed that revascularization is associated with higher increases in root length and thickness compared to calcium hydroxide and MTA, as well as excellent survival rates [6]. Alobaid AS et al., suggested that revascularization has comparable but not superior clinical and radiographic results compared to the traditional apexification procedures when analysing the dental survival success rate and adverse events besides quantifying changes in the root length, width, and area [7]. Chen SJ and Chen LP, evaluated the success rate through periapical radiographs with a 12-month follow-up and observed that the regenerative endodontic treatment was identical to the apexification technique [8]. Silujjai J and Linsuwanont P, stated that both methods provide a reliable result in terms of the resolution of pulp necrosis and the survival of teeth with incomplete root formation. However, none of these treatments offers predictable and satisfactory root development [9]. Kahler B et al., stated that teeth treated with regenerative endodontic procedures show clinical results comparable to traditional calcium hydroxide apexification and MTA techniques. They concluded that teeth treated with revascularization showed more adverse-effects, suggesting a need for a patient complete analysis before choosing a final treatment plan [10].
In the present case, CBCT images revealed the presence of the destruction of the buccal cortical bone [Table/Fig-2]. The presence of endodontic infection developed from necrosis, and the type of tooth movement and the applied orthodontic force may justify this finding [11]. The traditional method of apexification associated with interruption orthodontic treatment was chosen [8,9]. An immediate endodontic intervention was performed to remove all necrotic contents. NaOCl’s capacity for dissolving organic matter and its microbial properties play a fundamental role in the process of root canal decontamination. In addition, the root canal was irrigated with a 17% EDTA solution for 3 minutes prior to root canal drying to remove the smear layer and promote the opening of the dentinal tubules, which favours the diffusion of the calcium hydroxide paste [12].
The success of the apexification depends on the correct choice of medication used between sessions, as well as adequate filling and the minimum permanence time of the same inside the root canal, which enables it to manifest its total effectiveness. Calcium hydroxide paste was chosen for intracanal medication due to its clinical efficacy and its essential properties, among which the antimicrobial effect is highlighted due to its inhibition of bacterial cell enzymes at the cytoplasmic membrane level and the mineralising effect through tissue enzymatic activation, as verified by its action on alkaline phosphatase [12,13]. Six medication applications were performed at a 12-month interval, with a minimum of 60 days between sessions. This is corroborated by a study by Estrela C et al., that analysed the time required for calcium hydroxide to eliminate microorganisms in infected root canals [14].
Studies indicate that the speed of mineralised tissue barrier formation ranges from 3 to 24 months and that the suggested time for calcium hydroxide changes also ranges from once every 3 months to once every 6-8 months [13,14]. In this case, complete closure within 12 months of treatment was verified, which facilitated the filling of the root canal and the subsequent permanent restoration of the element.
Conclusion
The apexification has favourable results when it is well indicated for cases involving pulp necrosis in teeth with incomplete root formation.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jul 10, 2019
Manual Googling: Oct 19, 2019
iThenticate Software: Nov 15, 2019 (14%)
[1]. Diogenes A, Henry MA, Teixeira FB, Hargreaves KM, An update on clinical regenerative endodonticsEndod Topics 2013 28:2-23.10.1111/etp.12040 [Google Scholar] [CrossRef]
[2]. Guerrero F, Mendoza A, Ribas D, Aspiazu K, Apexification: A systematic reviewJ Conserv Dent 2018 21(5):462-65.10.4103/JCD.JCD_96_1830294103 [Google Scholar] [CrossRef] [PubMed]
[3]. Cvek M, Prognosis of luxated non-vital maxillary incisors treated with calcium hydroxide and filled with gutta-percha. A retrospective clinical studyEndod Dent Traumatol 1992 8:45-55.10.1111/j.1600-9657.1992.tb00228.x1521505 [Google Scholar] [CrossRef] [PubMed]
[4]. Huang GT, Apexication: the beginning of its endInt Endod J 2009 42(10):855-66.10.1111/j.1365-2591.2009.01577.x19549154 [Google Scholar] [CrossRef] [PubMed]
[5]. Diogenes A, Ruparel NB, Shiloah Y, Hargreaves KM, Regenerative endodontics: a way forwardJ Am Dent Assoc 2016 147:372-80.10.1016/j.adaj.2016.01.00927017182 [Google Scholar] [CrossRef] [PubMed]
[6]. Jeeruphan T, Jantarat J, Yanpiset K, Suwannapan L, Khewsawai P, Hargreaves KM, Mahidol study 1: Comparison of radiographic and survival outcomes of immature teeth treated with either regenerative endodontic or apexification methods-a retrospective studyJ Endod 2012 38:1330-36.10.1016/j.joen.2012.06.02822980172 [Google Scholar] [CrossRef] [PubMed]
[7]. Alobaid AS, Cortes LM, Lo J, Nguyen TT, Albert J, Abu-Melha AS, Radiographic and clinical outcomes of the treatment of immature permanent teeth by revascularization or apexification: A pilot retrospective cohort studyJ Endod 2014 40:1063-70.10.1016/j.joen.2014.02.01625069909 [Google Scholar] [CrossRef] [PubMed]
[8]. Chen SJ, Chen LP, Radiographic outcome of necrotic immature teeth treated with two endodontic techniques: A retrospective analysisBiomed J 2016 39(5):366-71.10.1016/j.bj.2015.12.00627884384 [Google Scholar] [CrossRef] [PubMed]
[9]. Silujjai J, Linsuwanont P, Treatment outcomes of apexification or revascularization in nonvital immature permanent teeth: A retrospective studyJ Endod 2017 43(2):238-45.10.1016/j.joen.2016.10.03028132710 [Google Scholar] [CrossRef] [PubMed]
[10]. Kahler B, Rossi-Fedele G, Chugal N, Lin LM, An evidence-based review of the efficacy of treatment approaches for immature permanent teeth with pulp necrosisJ Endod 2017 43(7):1052-57.10.1016/j.joen.2017.03.00328511779 [Google Scholar] [CrossRef] [PubMed]
[11]. Von Böhl M, Ren Y, Fudalej PS, Kuijpers-Jagtman AM, Pulpal reactions to orthodontic force application in humans: A systematic reviewJ Endod 2012 38:1463-69.10.1016/j.joen.2012.07.00123063219 [Google Scholar] [CrossRef] [PubMed]
[12]. Cvek M, Hollender L, Nord CE, Treatment of non- vital permanent incisors with calcium hydroxide. VI. A clinical, microbiological and radiological evaluation of treatment in one sitting of teeth with mature or immature rootOdont Revy 1976 27:93-108. [Google Scholar]
[13]. Estrela C, Estrela CRA, Pécora JD, A study of the time necessary for calcium hydroxide to eliminate microorganism in infected canalsJ Applied Oral Science 2003 12:133-37.10.1590/S1678-7757200300020000921409326 [Google Scholar] [CrossRef] [PubMed]
[14]. Estrela C, Pécora JD, Sousa-Neto MD, Estrela CRA, Bammann LL, Effect of vehicle on antimicrobial properties of calcium hydroxide pasteBraz Dent J 1999 10:63-72. [Google Scholar]