Introduction
Local anaesthesia is used to reduce pain while performing the extraction of teeth. But local anaesthesia injection itself causes pain while administration, especially palatal injections. Many patients avoid dental extractions due to the same reason, which can lead to life threatening situations. In the present-day dental practice, providing treatment with least amount of pain and discomfort is the key.
Aim
The study was done to compare the efficacy of 4% articaine and 2% mepivacaine without palatal injection for assessment of pain during maxillary teeth extraction.
Materials and Methods
A double blinded pilot randomised clinical trial was performed on 54 patients which required extraction of anterior and posterior maxillary teeth. Single buccal infiltration of 1 mL of 4% Articaine hydrochloride with adrenaline 1:200000 solution was given to 27 patients in study group A and 1 mL of 2% Mepivacaine with adrenaline 1:200000 was given to 27 patients in control group B. Objective signs of palatal anaesthesia was checked and pain was assessed by VAS scale. Mann-Whitney U test was used to compare the pain at different stages of extraction between group A and group B. Chi-square test was used to compare palatal injection needed between groups. The statistical analysis was performed with the SPSS version 15.
Results
The subjects who required re-anaesthesia is significantly higher percentage (70.4%) in the Mepivacaine group than compared to Articaine group (29.6%) (p=0.003). Hence, patients in the group where 4% articaine was administered showed significant reduction of pain without palatal anaesthesia.
Conclusion
Articaine 4% was superior in comparison to 2% Mepivacaine in its characteristics of bony diffusion and there was no absolute requirement to use palatal infiltration for the extraction of maxillary teeth.
Buccal infiltration, Extraction, Local anaesthesia, Palatal anaesthesia
Introduction
Removal of a tooth, even if it is mobile will cause pain. Pain is a protective mechanism of the body to tissue injury caused by different stimulations. Dental pain is usually acute inflammatory in nature, and it compels the patient to seek professional help [1]. Reduction of pain has been the subject of continuous research in the field of Oral and Maxillofacial Surgery. Intraoperative and postoperative pain varying in intensity and duration may affect a patient during an oral surgical procedure. Therefore, a method to decrease or eliminate pain has its usefulness justified.
The number of local anesthetic agents available has improved the interest in research on dental pain control. Thus, local anaesthesia is required to prevent pain during the extraction. The mechanism of action of local anesthetia is by stoppage of generation and conduction of nerve impulses and prevention from reaching the brain, hence not interpreted as pain by the patient. The availability of the number of local anesthetic agents to control intra-operative and post-operative pain has led to several studies comparing the efficacy of one over the other [2]. For the extraction of maxillary teeth, it is absolutely necessary that palatal infiltration or block be given. Palatal injections are very painful. Many patients felt pain during injection even after the application of surface anaesthesia palatally prior to the injection. The palatal mucosal binding to its underlying periosteum and its abundant nerve supply makes injections to the palate extremely painful. The pain can also be caused by the displacement of mucoperiosteum.
However, the injection of local anaesthesia prior to the tooth extraction itself causes pain and thus induces great anxiety and fear in the patient [3, 4]. Many factors are attributed to this discomfort, including the speed of injection, the volume of solution, the density of the tissue and psychological factors. The acidic pH of the anesthetic solutions plays an important role in aggravating uneasiness during local anesthetic administration.
Among the different techniques of local anaesthesia administration, palatal anaesthesia proved to be a very traumatic experience reported by the majority of the patients [5]. The firmly adherent palatal mucosal binding to its underlying periosteum and its abundant nerve supply makes injections to the palate extremely painful [6]. Injection of the solution causes separation of tightly bound mucoperiosteum from the underlying bone of the hard palate resulting in discomfort to the patient [7].
Therefore, various techniques have been advocated to reduce the pain of palatal injections. The most commonly practiced is the application of topical anesthetics prior to the injection. Even though other methods like, topical cooling of the palate, computerised injection systems, pressure administration, application of Eutectic Mixture Of Local Anesthetics (EMLA), and transcutaneous Electrical Nerve Stimulation (TENS) are mentioned in the literature but it is not universally accepted [4].
The anesthetic agent which is gaining popularity in oral surgery for its superior property of pain control is Articaine. The advantage of the drug is due to its special pharmacokinetics, property of excellent bone penetration and its effectiveness in patients with hypokalaemic sensory overstimulation [8,9]. The hypothesis is that, the different chemical structure, presence of thiophene ring which is a substitution of the aromatic ring in articaine, causes increased lipid solubility and potency. This will help a major amount of the injected anesthetic to enter the neurons [8,10]. The extra ester ring is responsible for the property of increased lipid solubility, intrinsic potency, and increased plasma protein binding property. These features are as shown reduced latency, increased duration of anaesthesia and increased hard tissue diffusion clinically [11].
Mepivacaine is found to be a safe local anesthetic to be used in children. Mepivacaine has very mild vasodilation property which leads to longer duration of pulpal anaesthesia compared to most of the local anesthetics, when administered without a vasoconstrictor. Hence, it is recommended for patients where vasoconstrictor is not indicated [12].
Therefore, this study compares the efficacy of 4% Articaine and 2% Mepivacaine without palatal injection for the extraction of the maxillary tooth. As the LA given to a patient is the same irrespective of anterior or posterior area, the same criteria are followed in this study. Indeed, the property of Articane is, increased bone diffusion, hence the effect of anaesthesia will be achieved for both firm or mobile tooth [13]. To the best of our knowledge this study is first of its kind in Malaysia with an aim to compare the efficacy of 4% articaine and 2% mepivacaine without palatal injection for assessment of pain during maxillary teeth extraction and other specific objectives were to compare objective symptoms of numbness, pain intensity during flap elevation, pain intensity during tooth extraction and requirement of palatal injections between study group and control group.
Materials and Methods
A double-blinded pilot randomised clinical trial was carried out from February 2017 to March 2018. It was a parallel-group study design with 1:1 allocation ratio. As it was a pilot study Julious rule of thumb was used for sample size calculation [14].
The trial is registered in Clinical trial registry with no: NCT03470532. Ethical approval was obtained from the Human and Ethics Committee of Melaka Manipal Medical College- MMMC/FOD/AR/B5/E C-2017(24). The informed consent form was collected from the patients prior to the commencement of the procedure. All subject information was kept confidential by the research team.
All healthy patients (ASA I) or patients with mild systemic disease with no functional limitations (ASA II) requiring extraction of maxillary teeth including grossly decayed tooth, grade I mobile tooth, root stumps and indicated for therapeutic reasons and who were not allergic to the drugs or anesthetic agents used in the surgical protocol were included in the study.
All patients who were allergic to local anesthetics, those who had severe systemic disease and classified under (ASA III & ASA IV) and under anti-inflammatory drugs and pain killers were not included in the study. Patients having Grade II and Grade III mobile tooth and infected tooth were also excluded from the study.
The consented 54 participants were randomised to Articaine and Mepivacaine groups by lottery method. A double blinding technique was done by blinding the operator and patient. Based on the randomised group, the dental surgery assistant provided the masked cartridge of the respective local anesthetic agent to the operator. Year 5 Dental students performed the procedure. A thorough case history was taken, and a clinical examination was done before the procedure was carried out. Patients were explained about the Visual Analogue Scale (VAS) before administring them the local anesthetic. The VAS was composed of a marked, continuous, horizontal, 100-mm line, anchored by the endpoints of “no pain” on the left and “worst pain” on the right.
In Group A, the buccal mucosa was dried with cotton gauze, and a topical anesthetic gel was applied to the buccal injection site and a buccal infiltration of 1 mL of 4% Articaine hydrochloride with adrenaline 1:200000 was administered along the long axis of the corresponding tooth to be extracted.
In the control group B, a similar protocol was followed except that after the topical anesthetic application, a buccal infiltration of 1 mL of 2% Mepivacaine with adrenaline 1:200000 was administered.
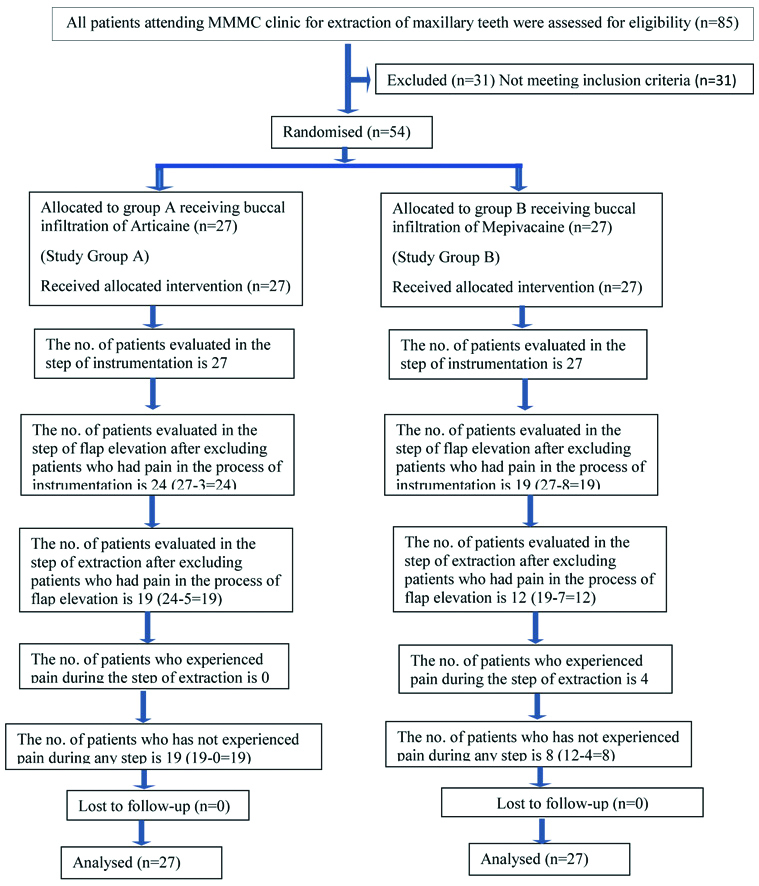
After 10 minutes, the objective signs of local anaesthesia were checked using a sharp periosteal elevator on the palatal gingival aspect of the corresponding tooth to be extracted. If the objective symptoms were negative, then the tooth extraction was completed with the sequential steps of mucoperiosteal flap elevation and removal of the tooth using forceps. Each step was performed at an interval of 3 minutes. The pain experienced by the patient during any of the steps, if any, was measured using the VAS scale and recorded. If the pain was below 44 in the VAS scale, then the extraction was completed without any additional local anaesthesia. If the patient complained of pain during any of the steps (>44 in VAS scale), an additional injection of the local anesthetic solution was given on the palatal side, and the extraction was completed, and this patient was not considered for further steps of the study. According to VAS, scores from 5 to 44 mm is considered as mild pain and from 45 to 74 mm as moderate pain [15]. In the literature it is shown that the extractions which were performed without further administration of LA were categorised as successful. All the patients in our study were comfortable without supplementary LA to continue with the procedure in mild pain category [Table/Fig-1] [16,17].
Consort Diagram.
*Analysis of 27 subjects were done, as author has performed the procedure of extraction in all 27 cases in both the groups. Patients who has experienced pain during any step were excluded for statistical analysis not from the treatment
Statistical Analysis
The tool used in this study is the VAS. Mann-Whitney U test was used to compare the pain at different stages of extraction between group A and group B. Chi-square test was used to compare palatal injection needed between the groups and if p<0.05, the result was considered statistically significant. The statistical analysis was performed with the SPSS version 15.
Results
The gender and Ethnicity distribution of the study participants are shown in [Table/Fig-2] The age of participants in the Articaine administrated group ranged from 18 to 70 years (Mean=44.4, SD=18.9) and that of Mepivacaine administrated group was 15 to 65 years (Mean=41.5, SD=14.9).
Socio-demography profile of the patients.
| Variables | Articaine (n=27) Freq. (%) | Mepivacaine (n=27) Freq. (%) |
|---|
| Gender | Male | 13 (48.1) | 7 (25.9) |
| Female | 14 (51.9) | 20 (74.1) |
| Ethnicity | Malay | 7 (25.9) | 10 (37.0) |
| Chinese | 16 (59.3) | 12 (44.4) |
| Indian | 2 (7.4) | 2 (7.4) |
| Others | 2 (7.4) | 3 (11.1) |
[Table/Fig-3,4 and 5] shows the comparison of the pain at different stages of extraction between group A and group B. [Table/Fig-6] shows the details of the stage which required palatal anaesthesia.
Comparison of objective symptoms of numbness between study group A and study group B.
| Variables | | Q1 | Median | Q3 | p-value |
|---|
| Objective symptoms of numbness | Drug A Articaine | 0.0 | 10.0 | 20.0 | 0.263 |
| Drug B Mepivacaine | 0.0 | 20.0 | 50.0 |
Mann-Whitney U test is done. Q1 is the first quartile value, and Q3 the third quartile value. Q1=0 means 25% of the participants in that group had symptom score 0 or less, Q3=20 means 75 % of the participants had their score less than 20 for Articaine and 25% of the participants in group Mepivacaine had symptom score less than 0 or less, 75% of the participants had scores less than 50
Comparison of pain intensity during flap elevation between study group A and study group B.
| Variables | Q1 | Median | Q3 | p-value |
|---|
| Pain intensity during flap elevation | Drug A Articaine | 0.0 | 10.0 | 40.0 | 0.087 |
| Drug B Mepivacaine | 10.0 | 20.0 | 50.0 |
Mann-Whitney U test is done. Q1 is the first quartile value, and Q3 the third quartile value. Q1=0 means 25% of the participants in that group had symptom score 0 or less, Q3=40 means 75 % of the participants had their score less than 40 for Articaine and 25% of the participants in group Mepivacaine had symptom score less than 10 or less, 75% of the participants had scores less than 50
Comparison of pain intensity during tooth extraction between study group A and study group B.
| Variables | Q1 (25%) | Median | Q3 (75%) | p-value |
|---|
| Pain intensity during tooth extraction | Drug A Articaine | 0.0 | 0.0 | 20.0 | 0.048 |
| Drug B Mepivacaine | 0.0 | 25.0 | 50.0 |
Mann-Whitney U test is done. Q1 is the first quartile value, and Q3 the third quartile value. Q1=0 means 25% of the participants in that group had symptom score 0 or less, Q3=20 means 75 % of the participants had their score less than 20 for Articaine and 25% of the participants in group Mepivacaine had symptom score less than 0 or less, 75% of the participants had scores less than 50
Stage at which palatal injection was required*.
| Based on objective symptoms of numbness | During flap elevation | During tooth extraction | Not required at any stage of the procedure | Total |
|---|
| Treatment | Freq. (%) | Freq. (%) | Freq.(%) | Freq. (%) | Freq.(%) |
| Articaine | 3 (11.11) | 5 (18.52) | 0 (0) | 19 (70.37) | 27 (100) |
| Mepivacaine | 8 (29.63) | 7 (25.93) | 4 (14.81) | 8 (29.63) | 27 (100) |
*VAS pain score was assessed at each stage
The distribution of subjects who required re-anaesthesia is shown in [Table/Fig-7]. Significantly higher percentage (70.4%) of subjects in the Mepivacaine group required re-anaesthesia compared to Articaine (29.6%) group (p=.003). The null hypothesis was rejected.
Comparison of palatal injection requirement between Articaine and Mepivacaine group.
| Treatment | Injection given | Injection not given | Total | | |
|---|
| Freq.(%) | Freq.(%) | Freq.(%) | χ2 Value | p-value |
|---|
| Articaine | 8 (29.6%) | 19 (70.4%) | 27 (100) | 8.96 | .003 |
| Mepivacaine | 19 (70.4%) | 8 (29.6%) | 27 (100) | | |
Chi square test is done
Discussion
In 2001, Malamed MF et al., compared the safety and efficacy of 4% Articaine with epinephrine 1:100,000 with 2% Lidocaine with epinephrine 1:100,000 and found that 4% Articaine with epinephrine 1:100,000 was more efficient in providing pain relief during most dental procedures. It was also well tolerated, had appropriate time of onset and duration of anaesthesia for clinical use as compared to other commercially available local anesthetics [18]. Our study is in accordance with these results.
Fan S et al., compared Articaine with lignocaine in maxillary extractions in 71 patients and concluded that when Articaine hydrochloride is used as the local anesthetic then palatal injection is not indicated for the extraction of permanent maxillary teeth. The time limit was 5 min for the initiation of the procedure [8]. Our results are also in supportive of this study.
Sreekumar K and Bhargava D, conducted a study to compare the onset and duration of action of soft tissue and pulpal anaesthesia with three volumes 0.6 mL, 0.9 mL and 1.2 mL of 4% Articaine with 1:100,000 epinephrine in maxillary anaesthesia and found that maxillary infiltration anaesthesia with Articaine and epinephrine had a faster onset, a greater success rate and a longer duration with a volume of 1.7 mL which is similar to our study [19].
The duration of action of an anesthetic is proportional to its degree of protein binding and injection site or concentration of vasoconstrictor present in the local anesthetic solution [11]. Articaine has the greatest protein binding percentages compared to other amide local anesthetics [19].
In our pilot study, total no of re-anaesthesia on the palatal side given to group A (Articaine) was 29.6% while to group B (Mepivacaine) was 70.4% which was statistically significant. This pilot study showed that Articaine has superior diffusion properties as compared to Mepivacaine as observed in the previous studies [20-22].
Limitation and Future Recommendation
The pain threshold varies in each patient. As the pain threshold is not a factor which can be controlled by the operator, it is a major limitation. Another limitation was that, the different operators have different skills in injection technique and tooth extraction procedure. Similar studies with a larger sample size will give a better perspective of the study.
Conclusion
The results of this pilot study indicated that Articaine hydrochloride 4% with epinephrine 1:200,000 produced more effective palatal anaesthesia (63.0%) than the 2% Mepivacaine with 1:20,000 without any palatal injection given. From our study, we conclude that Articaine 4% has an increased bone penetration property in comparison to 2% Mepivacaine. Hence in maximum cases there was no absolute necessity to use palatal infiltration for the removal of maxillary teeth while using Articaine as local anaesthesia.
Mann-Whitney U test is done. Q1 is the first quartile value, and Q3 the third quartile value. Q1=0 means 25% of the participants in that group had symptom score 0 or less, Q3=20 means 75 % of the participants had their score less than 20 for Articaine and 25% of the participants in group Mepivacaine had symptom score less than 0 or less, 75% of the participants had scores less than 50
Mann-Whitney U test is done. Q1 is the first quartile value, and Q3 the third quartile value. Q1=0 means 25% of the participants in that group had symptom score 0 or less, Q3=40 means 75 % of the participants had their score less than 40 for Articaine and 25% of the participants in group Mepivacaine had symptom score less than 10 or less, 75% of the participants had scores less than 50
Mann-Whitney U test is done. Q1 is the first quartile value, and Q3 the third quartile value. Q1=0 means 25% of the participants in that group had symptom score 0 or less, Q3=20 means 75 % of the participants had their score less than 20 for Articaine and 25% of the participants in group Mepivacaine had symptom score less than 0 or less, 75% of the participants had scores less than 50
*VAS pain score was assessed at each stage
Chi square test is done
Author Declaration:
Financial or Other Competing Interests: No
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Aug 13, 2019
Manual Googling: Aug 27, 2019
iThenticate Software: Nov 05, 2019 (17%)
[1]. Hunter JP, Simmonds MJ, Pain: putting the whole person at the centrePhysiotherapy Canada Physiotherapie Canada 2010 62(1):01-08.10.3138/physio.62.1.121197173 [Google Scholar] [CrossRef] [PubMed]
[2]. Silva LC, Santos TD, Santos JA, Maia MC, Mendonca CG, Articaine versus lidocaine for third molar surgery: A randomized clinical studyMedicina Oral, Patologia Oral y Cirugia Bucal 2012 17(1):e140-45.10.4317/medoral.1714822157664 [Google Scholar] [CrossRef] [PubMed]
[3]. Hupp JR, Contemporary Oral and Maxillofacial Surgery 2013 6th edPhiladelphia, United StatesElsevier Health Services [Google Scholar]
[4]. Uckan S, Dayangac E, Araz K, Is permanent maxillary tooth removal without palatal injection possible?Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006 102(6):733-35.10.1016/j.tripleo.2005.12.00517138173 [Google Scholar] [CrossRef] [PubMed]
[5]. Frazer M, Contributing factors and symptoms of stress in dental practiceBritish Dental Journal 1992 173(3):11110.1038/sj.bdj.48079481503841 [Google Scholar] [CrossRef] [PubMed]
[6]. Isen DA, Articaine: pharmacology and clinical use of a recently approved local anestheticDentistry Today 2000 19(11):72-77. [Google Scholar]
[7]. McArdle BF, Painless palatal anesthesiaJ Am Dent Assoc 1997 128(5):64710.14219/jada.archive.1997.02659150649 [Google Scholar] [CrossRef] [PubMed]
[8]. Fan S, Chen WL, Yang ZH, Huang ZQ, Comparison of the efficiencies of permanent maxillary tooth removal performed with single buccal infiltration versus routine buccal and palatal injectionOral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics 2009 107(3):359-63.10.1016/j.tripleo.2008.08.02518996033 [Google Scholar] [CrossRef] [PubMed]
[9]. Srinivasan N, Kavitha M, Loganathan CS, Padmini G, Comparison of anesthetic efficacy of 4% articaine and 2% lidocaine for maxillary buccal infiltration in patients with irreversible pulpitisOral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics 2009 107(1):133-36.10.1016/j.tripleo.2008.09.00219101495 [Google Scholar] [CrossRef] [PubMed]
[10]. Vree TB, Gielen MJ, Clinical pharmacology and the use of articaine for local and regional anaesthesiaBest Practice & Research Clinical Anaesthesiology 2005 19(2):293-308.10.1016/j.bpa.2004.12.00615966499 [Google Scholar] [CrossRef] [PubMed]
[11]. Hawkins JM, Moore PA, Local anesthesia: advances in agents and techniquesDental clinics of North America 2002 46(4):719-32.:ix10.1016/S0011-8532(02)00020-4 [Google Scholar] [CrossRef]
[12]. S M. Handbook of local anesthesia Philadelphia: Elsevier Health Sciences; 2012 [Google Scholar]
[13]. Bataineh AB, Al-Sabri GA, Extraction of maxillary teeth using articaine without a p[alatal injection: A comparison between the anterior and posterior regions of the maxillaJournal of Oral and Maxillofacial Surgery: Official Journal of the American Association of Oral and Maxillofacial Surgeons 2017 75(1):87-91.10.1016/j.joms.2016.06.19227528103 [Google Scholar] [CrossRef] [PubMed]
[14]. Whitehead AL, Julious SA, Cooper CL, Campbell MJ, Estimating the sample size for a pilot randomised trial to minimise the overall trial sample size for the external pilot and main trial for a continuous outcome variableStatistical Methods in Medical Research 2016 25(3):1057-73.10.1177/096228021558824126092476 [Google Scholar] [CrossRef] [PubMed]
[15]. Jensen MP, Chen C, Brugger AM, Interpretation of visual analog scale ratings and change scores: a reanalysis of two clinical trials of postoperative painJ Pain 2003 4(7):407-14.10.1016/S1526-5900(03)00716-8 [Google Scholar] [CrossRef]
[16]. Khan SR, Qazi SR, Extraction of maxillary teeth by dental students without palatal infiltration of local anaesthesia: a randomised controlled trialEur J Dent Educ 2017 21(4):e39-e42.10.1111/eje.1221527324934 [Google Scholar] [CrossRef] [PubMed]
[17]. Sirintawat N, Sawang K, Chaiyasamut T, Wongsirichat N, Pain measurement in oral and maxillofacial surgeryJ Dent Anesth Pain Med 2017 17(4):253-63.10.17245/jdapm.2017.17.4.25329349347 [Google Scholar] [CrossRef] [PubMed]
[18]. Malamed SF, Gagnon S, Leblanc D, Efficacy of articaine: a new amide local anestheticJ Am Dent Assoc 2000 131(5):635-42.10.14219/jada.archive.2000.023710832257 [Google Scholar] [CrossRef] [PubMed]
[19]. Sreekumar K, Bhargava D, Comparison of onset and duration of action of soft tissue and pulpal anesthesia with three volumes of 4% articaine with 1:100,000 epinephrine in maxillary infiltration anesthesiaOral and Maxillofacial Surgery 2011 15(4):195-99.10.1007/s10006-011-0275-821590273 [Google Scholar] [CrossRef] [PubMed]
[20]. Srisurang S, Narit L, Prisana P, Clinical efficacy of lidocaine, mepivacaine, and articaine for local infiltrationJournal of Investigative and Clinical Dentistry 2011 2(1):23-28.10.1111/j.2041-1626.2010.00035.x25427324 [Google Scholar] [CrossRef] [PubMed]
[21]. Gazal G, Is articaine more potent than mepivacaine for use in oral surgery?J Oral Maxillofac Res 2018 9(3):e510.5037/jomr.2018.930530429965 [Google Scholar] [CrossRef] [PubMed]
[22]. Kambalimath DH, Dolas RS, Kambalimath HV, Agrawal SM, Efficacy of 4% Articaine and 2% Lidocaine: A clinical studyJ Maxillofac Oral Surg 2013 12(1):03-10.10.1007/s12663-012-0368-424431806 [Google Scholar] [CrossRef] [PubMed]