Introduction
Chikungunya infection is an acute disabling illness characterised by high fever and severe arthralgia. Most of the patients recover completely; however few may develop post-Chikungunya Chronic Inflammatory Rheumatism (CHIK-CIR).
Aim
To detect the seroprevalence of chikungunya among Rheumatoid Arthritis (RA) patients and to demonstrate association between them.
Materials and Methods
This was a prospective study conducted from July 2018 to November 2018 at the Department of Microbiology, in a tertiary care hospital. Patients attending rheumatology clinic with complaints of arthritis and clinically suspected to have RA were included in the study. Samples were tested for Anti-Citrullinated Peptide Antibodies (ACPA), Anti-Chikungunya IgM and IgG antibodies by Enzyme Linked Immunosorbent Assay (ELISA) as per manufacturer’s instructions.
Results
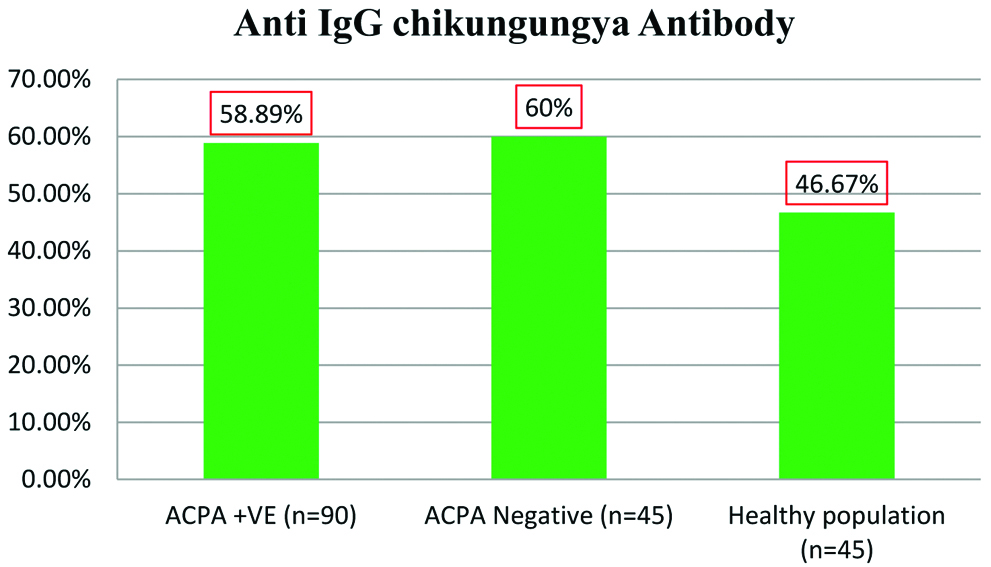
A total of 373 patients were included in the study. Of these serum samples 90 (24.12%) samples were positive for ACPA, with female predominance (n=66, 73.33%) and 29 (7.77%) patients’ serum samples tested positive for chikungunya IgM. Highest positivity for APCA was observed in the age group 40-60 years (n=47, 52.22%). IgG ELISA for chikungunya was positive in 58.89% (n=53), 60% (n=27) and 46.67% (n=21) of clinically suspected and ACPA positive, 45 clinically suspected but ACPA negative and 45 healthy individuals respectively. The difference was not statistically significant across the different groups. However, seroprevalence was higher among patients suffering with arthralgia as compared to that of healthy population group.
Conclusion
Rheumatologist should always consider Chikungunya infection as one of the causes for arthralgia. In endemic countries like India it is difficult to ascertain whether chikungunya infection progresses to RA or not.
Arthralgia, Chikungunya fever, Post-chikungunya chronic inflammatory rheumatism
Introduction
Chikungunya an arboviral infection, transmitted by Aedes aegpti species of mosquito which has emerged as an epidemic threat over the past 15 years. Chikungunya Virus is an enveloped, spherical single-stranded RNA virus about 60-70 nm in diameter, belonging to the alphavirus genus and family Togaviridae. This virus was first identified in 1952-53 during an outbreak that occurred in the Makonde Plateau in the southern region of Tanzania [1,2]. In the Makonde language, the word “chikungunya” literally means “the one which bends up” referring to the bent posture of affected patients due to severe joint pains. It causes an acute disabling illness characterised by high fever and severe arthralgia called Chikungunya Fever (CHIKF). The infection is associated with significant morbidity but very low mortality. Most of the patients recover completely; however, in some patients, the symptoms may last for several months and at times for years, which is called as ‘post’ CHIK-CIR. It mainly affects the quality of life [3-5]. In India, the virus re-emerged as a major epidemic in 2006 after a gap of 32 years, imposing heavy epidemiological burden [6-8].
More than 1.3 million cases were reported in 2006, with attack rates of 45% in some regions [9]. Since then chikungunya virus infection has caused severe outbreaks every year across the country. It continues to be endemic in India, Africa, some countries in Southeast Asia and Latin America. Massive outbreaks of chikungunya virus infection was experienced in different states of India during 2005-2006. The first report of the CHIKV epidemic was from Andhra Pradesh which was the most affected state [10].
RA is a common autoimmune disease characterised by chronic progressive inflammation of joints. Some studies have suggested the role of viral infection in RA initiation [11,12]. Cytokines play an important role in immunopathology of chikungunya virus induced arthritis or arthralgia, as the cytokine profile in chikungunya chronic infection is similar to the cytokine signature seen in RA. Though IL-2, IL-10 and IFN-γ have been implicated in the pathogenesis of chikungunya but the detection of IL-7 and IL-15 is significantly interesting, because IL-7 is known to have an important role in the development of RA while IL-15 has been associated with the development of joint inflammation. Few studies have suggested to use these cytokines as biomarkers for the diagnosis but in the absence of validation and owing to biomarker heterogeneity, these tests are limited in clinical practice [13,14]. Incidences of chronic chikungunya virus-associated joint disease (RA) have been frequently reported but a causal relationship has not been established till date. Most of these studies were follow-up studies of the chronic chikungunya patients for longer period and reported their progression to RA. Various studies with different follow-up periods (2.5-72 months) have reported the prevalence of CHICK-CIR differently ranging from 4.4-81.1% [5,11,15-19]. Development of symptoms of RA in these studies was due to chikungunya infection or otherwise cannot be commented as none of the studies could demonstrate chikungunya antibodies in the synovial fluid.
On the basis of above context this study was planned to detect the seroprevalence of chikungunya infection among clinically and laboratory confirmed RA patients and to evaluate the association between the two.
Materials and Methods
This was a prospective study conducted in the Department of Microbiology from July 2018 to November 2018, at a tertiary care teaching hospital, located in Southern India, Andhra Pradesh, India. It is a laboratory based study; tests were done on left over samples and no financial burden was imposed on the patients therefore ethical clearance was not obtained. A total of 373 patients presenting with joint pains and who attended the Rheumatology clinic during the study period were included.
Sample size: No previous study was available on the detection of prevalence of anti-chikungunya antibodies in RA patients therefore sample size calculation was not feasible and all patients attending the rheumatology clinic during the study period with complains of joint pains were included in the study. Around 5 mL of blood sample was collected from the patient. Serum was separated and kept at -40°c till further testing.
Exclusion criteria: Haemolysed, lipemic and grossly contaminated samples were excluded.
Samples were tested for Anti-citrullinated peptide antibody (ACPA), Anti-Chikungunya IgM and Anti-Chikungunya IgG antibodies.
Test for ACPA was done by ELISA using Anti-CP IgG ELISA Kit supplied by DIA.METRA.S.r.l Spello(PG)-Italy ELISA with sensitivity of 76% and specificity of 94% (As per kit insert).
Test for Anti-Chikungunya IgM antibody: It was done by ELISA using NIV chikungunya IgM Capture ELISA Kit supplied by ICMR-National Institute of Virology, Pune (India) with sensitivity of 95% and specificity of 98% (As per kit insert).
Test for Anti-chikungunya IgG: Samples positive for ACPA were further tested for Anti-chikungunya using CHIK jj DetectTM IgG ELISA wth sensitivity of 90.9% and specificity of 100% (as per kit insert) supplied by InBios International Inc. Seattle, WA, USA and equal number of controls (two groups; group A-45 randomly selected ACPA negative samples and group B-45 samples from healthy population) were also tested.
Statistical Analysis
Microsoft Excel Worksheet was used for data compilation. All continuous variables that were normally distributed were summarised as mean±SD and all categorical variables were represented as number and percentage. For the study purpose, samples positive for ACPA was considered as RA positive sample. Association between the two variables was calculated with chi-squared test using online link https:www.medcalc.org. and the p<0.05 was considered significant.
Results
Out of 373 patients, there was female (n=271, 72.65%) preponderance over males (n=102, 27.34%) with 66 females (73.33%) being positive for ACPA. The sex wise distribution of patients is depicted in [Table/Fig-1]. Maximum number of patients (n=198, 53.08%) were in the age group of 40-60 years with highest positivity (n=47, 52.22%); [Table/Fig-2]. From the 373 samples, 24.12% (n=90) were positive for ACPA. Of the 90 ACPA positive samples Anti-chikungunya IgG antibody ELISA was positive in 58.89% (n=53) samples.
Sex wise distribution of patients.
| Sex | Total patients (373) | ACPA (n-90) | Anti-IgM antibody (n-29) |
|---|
| Male | 102 | 24 (26.67%) | 8 (27.57%) |
| Female | 271 | 66 (73.33%) | 21 (72.41%) |
Age wise distribution of patients.
| Age-range (yrs) | Total number of patients (percentage) n=373 | Total number of ACPA positive patients (percentage) n=90 | Total number of IgM positive patients (percentage) n=29 |
|---|
| <20 | 18 (4.82) | 7 (7.78) | 0 (0) |
| 20-40 | 114 (30.56) | 28 (31.11) | 5 (17.24) |
| 40-60 | 198 (53.08) | 47 (52.22) | 24 (68.97) |
| 60-80 | 43 (11.52) | 8 (8.89) | 4 (13.79) |
Twenty nine samples (7.77%) tested positive for Anti-IgM chikungunya antibodies. Of these 29 IgM antibodies positive samples, 6 samples were also positive for ACPA. No significant difference was observed in the seroprevalence of Chikungunya between ACPA positive and ACPA negative samples with 60% and 46.67% being positive respectively [Table/Fig-3]. A difference of 12.59% was noted among patients with arthralgia to that of the healthy population, though not statistically significant [Table/Fig-4].
Seroprevalence of Chikungunya among ACPA (Anti-Citrullinated Peptide Antibody) Positive, ACPA negative and healthy population.
Comparison of seroprevalence of IgG Chikungunya among different groups.
| Anti-IgG chikungunya | Chi-square value | p-value |
|---|
| 1 | RA positive Group (n=90)53 (58.89%) | Control (n=90)48 (53.33%) | 0.562 | 0.4536 |
| 2 | Patients with arthralgia (n=135)80 (59.26%) | Healthy population (n=45)21 (46.67%) | 2.160 | 0.1416 |
Discussion
RA affects around 1% of the population with the female to male ratio of approximately 2.5-1. The incidence of RA increases with age and more commonly affects women than male. Generally autoimmune diseases are more common in females for reasons unknown but genetic (x-linked) and hormonal aspects are likely to be involved [20].
RA occurs at any age, but it most commonly begins in the middle age and the severity of the disease increases with the progression of age [21,22], in our study 52.22% (n=47) of ACPA positive patients were in the age range of 40-60 years which is in concordance to other studies available.
Though chikungunya manifestations subside in most of the patients but in some subset of patients there is development of CHIK-CIR over the years. In our study ACPA which is an important diagnostic marker for RA was positive in 24.12% (n=90) patients. Of the ACPA positive patients 58.89% patients were also positive for anti-chikungunya IgG antibodies indicating past infection with chikungunya virus. Seroprevalence of anti-IgG chikungunya antibody was high among all the three groups (46.6%, 58.89% and 60%). There was no significant difference in the seroprevalence of Anti-IgG chikungunya among ACPA positive and controls (Difference of 5.56% (95% CI-1.0 to 19.58). Chi square value=0.562 and p=0.4536), this depicts that there was no association between CHIKV infection and development of RA in our study, but difference of 12.59% (95% CI-1 to 28.4425, Chi square value=2.160 and p=0.1416) was found among patients suffering from joint pain to that of a healthy population group, though this difference was again not statistically significant. The high seroprevalence of anti-chikungunya IgG antibodies could be due to the endemicity of the chikungunya infection in our region. Since the La Reunion outbreak of chikungunya, reports of chronic CHIKV-associated joint diseases have increased. In most of these reports whether the underlying joint abnormalities were present prior to or at the time of infection cannot be confirmed [23-26]. It might have also been possible that the patient developed joint disease which was completely unrelated to chikungunya infection.
A study by Chang AY et al., reported that during 2015-2016 columbian epidemic, 25% of patients from the cohort of 500 patients had persistent joint pains at 20 months post infection period with chikungunya virus [27]. Few studies in the literature reported that chronic chikungunya infection led to the development of RA. Javelle E et al., studied 159 cases of chronic CHIK for over two years and reported that among them, 112 cases presented with symptoms of post-CHIK-CIR and 40 cases met the clinical and radiologic criteria for RA [5]. Another study by Bouquillard É and Combe B, reported 21 severe cases of RA post chikungunya virus infection in Reunion Island. Even in the presence of low rate of anti-CCP antibodies, outcome of the patient was severe in most cases; suggesting the role of viral infection in the initiation of RA [11]. None of the published studies in literature are similar to our study as most of the published studies were follow-up studies of chronic chikungunya patients progressing to RA whereas our study was conducted on patients with joint pains clinically suspected of RA. Our study highlights that in an endemic country like India proving the association of chikungunya and RA is difficult. Whether RA developed in chikungunya patients or chikungunya infection happened in RA patients is difficult to ascertain.
CHIKV infection triggers rapid innate immune responses, primarily by strong activation of type 1 interferon (IFN) and by production of proinflammatory cytokines [28,29]. The cytokine profile in CHIK chronic infection is similar to the cytokine signature seen in RA. Afterwards, the adaptive immune response begins to be stimulated, with production of specific IgM and IgG antibodies. Serum IgM is usually detected within an average period of 5-7 days of infection and can persist for 3-6 months. Anti-CHIKV IgG is detectable approximately 2 weeks after the onset of symptoms, that is between the acute and convalescent phase, which can remain elevated for a span of 6 months and persist for years [30-32].
In the present study Anti-chikungunya IgM antibody was found to be positive in 7.77% (n=29) samples, of which 20.69% (n=6) were also positive for ACPA indicating chikungunya infection as the probable cause for joint pain in these patients. Whether the chikungunya IgM positivity in these 6 ACPA positive patients was due to recent infection or due to prolonged persistence of IgM antibodies cannot be affirmed as it is reported that in few patients the IgM antibodies may persist even after 2-3 years of chikungunya infection [17,28,33]. The presence of both RA and Chikungunya infection can either be co-incidental, completely unrelated to each other or there might be a real association, causal or otherwise. One recent study has reported that CHIK-CIR can persist even after 6 years of follow-up, as was the case for 59% of patients from 2006-2012 in La Reunion, France [5]. Similarly the ACPA positivity was a consequence of chinkungunya infection or an incidental finding cannot be confirmed.
Future Recommendation
Rheumatologist should always consider chikungunya as the probable cause for arthralgia in the endemic region and follow the patient with radiological and laboratory markers to identify and diagnose CHIK-CIR and provide timely appropriate treatment to curtail its progression and development of complications.
Limitation
No follow-up of cases was done to study the progression of disease in Anti-chikungunya IgM antibody positive patients.
Conclusion
Seroprevalence of Chikungunya IgG antibodies was high in patients suffering from arthralgia as compared to the healthy population but no association existed between the RA and chikungunya infection. In endemic regions it is difficult to differentiate arthralgia due to chikungunya from that of other causes due to high seroprevalence of Anti-chikungunya antibodies.
Author Declaration:
Financial or Other Competing Interests: No
Was Ethics Committee Approval obtained for this study? No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jul 27, 2019
Manual Googling: Oct 21, 2019
iThenticate Software: Nov 12, 2019 (12%)
[1]. Yactayo S, Staples JE, Millot V, Cibrelus L, Ramon-Pardo P, Epidemiology of chikungunya in the AmericasJ Infect Dis 2016 214(suppl_5):S441-45.10.1093/infdis/jiw39027920170 [Google Scholar] [CrossRef] [PubMed]
[2]. Mohan A, Kiran DH, Manohar IC, Kumar DP, Epidemiology, clinical manifestations, and diagnosis of Chikungunya fever: Lessons learned from the re-emerging epidemicIndian J Dermatol 2010 55(1):54-63.10.4103/0019-5154.6035520418981 [Google Scholar] [CrossRef] [PubMed]
[3]. Simon F, Javelle E, Oliver M, Leparc-Goffart I, Marimoutou C, Chikungunya virus infectionCurr Infect Dis Rep 2011 13(3):218-28.10.1007/s11908-011-0180-121465340 [Google Scholar] [CrossRef] [PubMed]
[4]. Foissac M, Javelle E, Ray S, Guérin B, Simon F, Post-chikungunya rheumatoid arthritis, Saint MartinEmerg Infect Dis 2015 21(3):530-32.10.3201/eid2103.14139725695499 [Google Scholar] [CrossRef] [PubMed]
[5]. Javelle E, Ribera A, Degasne I, Gaüzère BA, Marimoutou C, Simon F, Specific management of post-chikungunya rheumatic disorders: a retrospective study of 159 cases in Reunion Island from 2006-2012PLoS Negl Trop Dis 2015 9(3):e000360310.1371/journal.pntd.000360325760632 [Google Scholar] [CrossRef] [PubMed]
[6]. Mourya DT, Mishra AC, Chikungunya feverLancet 2006 368(9531):186-87.10.1016/S0140-6736(06)69017-X [Google Scholar] [CrossRef]
[7]. Krishnamoorthy K, Harichandrakumar KT, Kumari AK, Das LK, Burden of chikungunya in India: Estimates of disability adjusted life years (DALY) lost in 2006 epidemicJ Vector Borne Dis 2009 46:26-35. [Google Scholar]
[8]. Mavalankar D, Shastri P, Bandyopadhyay T, Parmar J, Ramani KV, Increased mortality rate associated with chikungunya epidemic, Ahmedabad, IndiaEmerg Infect Dis 2008 14(3):412-15.10.3201/eid1403.07072018325255 [Google Scholar] [CrossRef] [PubMed]
[9]. World Health OrganizationOutbreak and spread of chikungunyaWkly Epidemiol Rec 2007 47:409-15. [Google Scholar]
[10]. Ravi V, Re-emergence of chikungunya virus in IndiaIndian J Med Microbiol 2006 24(2):83-84.10.4103/0255-0857.2517516687855 [Google Scholar] [CrossRef] [PubMed]
[11]. Bouquillard É, Combe B, A report of 21 cases of rheumatoid arthritis following Chikungunya fever. A mean follow-up of two yearsJoint Bone Spine 2009 76(6):654-57.10.1016/j.jbspin.2009.08.00519945329 [Google Scholar] [CrossRef] [PubMed]
[12]. Chang AY, Martins KA, Encinales L, Reid SP, Acuña M, Encinales C, Chikungunya arthritis mechanisms in the Americas: A cross-sectional analysis of chikungunya arthritis patients twenty-two months after infection demonstrating no detectable viral persistence in synovial fluidArthritis Rheumatol 2018 70(4):585-93.10.1002/art.4038329266856 [Google Scholar] [CrossRef] [PubMed]
[13]. Ng LF, Chow A, Sun Y, Kwek DJ, Lim P, Dimatatac F, IL-1b, IL-6, and RANTES as biomarkers of chikungunya severityPLoS One 2009 4(1):e426110.1371/journal.pone.000426119156204 [Google Scholar] [CrossRef] [PubMed]
[14]. Chirathaworn C, Poovorawan Y, Lertmaharit S, Wuttirattanakowit N, Cytokine levels in patients with chikungunya virus infectionAsian Pac J Trop Med 2013 6:631-34.10.1016/S1995-7645(13)60108-X [Google Scholar] [CrossRef]
[15]. Chopra A, Venugopalan A, Persistent rheumatic musculoskeletal pain and disorders at one year post-chikungunya epidemic in south Maharashtra-a rural community based observational study with special focus on naïve persistent rheumatic musculoskeletal cases and selected cytokine expressionIndian Journal of Rheumatology 2011 6(1):05-11.10.1016/S0973-3698(11)60023-X [Google Scholar] [CrossRef]
[16]. Gérardin P, Fianu A, Malvy D, Mussard C, Boussaïd K, Rollot O, Perceived morbidity and community burden after a Chikungunya outbreak: the TELECHIK survey, a population-based cohort studyBMC Medicine 2011 9(1):510.1186/1741-7015-9-521235760 [Google Scholar] [CrossRef] [PubMed]
[17]. Chopra A, Anuradha V, Ghorpade R, Saluja M, Acute Chikungunya and persistent musculoskeletal pain following the 2006 Indian epidemic: a 2-year prospective rural community studyEpidemiol Infect 2012 140(5):842-50.10.1017/S095026881100130021767452 [Google Scholar] [CrossRef] [PubMed]
[18]. Chaaithanya IK, Muruganandam N, Raghuraj U, Sugunan AP, Rajesh R, Anwesh M, Chronic inflammatory arthritis with persisting bony erosions in patients following chikungunya infectionThe Indian J Med Res 2014 140(1):142-45. [Google Scholar]
[19]. Miner JJ, Aw Yeang HX, Fox JM, Taffner S, Malkova ON, Oh ST, Brief report: chikungunya viral arthritis in the United States: a mimic of seronegative rheumatoid arthritisArthritis Rheumatol 2015 67(5):1214-20.10.1002/art.3902725605621 [Google Scholar] [CrossRef] [PubMed]
[20]. Smolen JS, Aletaha D, McInnes IB, Rheumatoid arthritisLancet 2016 388:2023-38.10.1016/S0140-6736(16)30173-8 [Google Scholar] [CrossRef]
[21]. Carmona L, Villaverde V, Hernandez-Garcia C, Ballina J, Gabriel R, Laffon A, The prevalence of rheumatoid arthritis in the general population of SpainRheumatology 2002 41:88-95.10.1093/rheumatology/41.1.8811792885 [Google Scholar] [CrossRef] [PubMed]
[22]. Ampofo RO, Osei-Sarpong C, Botwe BO, Rheumatoid arthritis among autoimmune diagnosed patients: A pilot study at Africa’s third largest hospitalTrop J Med Res 2016 19:88-93.10.4103/1119-0388.185425 [Google Scholar] [CrossRef]
[23]. Mizuno Y, Kato Y, Takeshita N, Ujiie M, Kobayashi T, Kanagawa S, Clinical and radiological features of imported chikungunya fever in Japan: a study of six cases at the National Center for Global Health and MedicineJ Infect Chemother 2011 17:419-23.10.1007/s10156-010-0124-y20862507 [Google Scholar] [CrossRef] [PubMed]
[24]. Sissoko D, Malvy D, Ezzedine K, Renault P, Moscetti F, Ledrans M, Post-epidemic Chikungunya disease on Reunion Island: course of rheumatic manifestations and associated factors over a 15-month periodPLoS Negl Trop Dis 2009 3:e38910.1371/journal.pntd.000038919274071 [Google Scholar] [CrossRef] [PubMed]
[25]. Schilte C, Staikowsky F, Couderc T, Madec Y, Carpentier F, Kassab S, Chikungunya virus-associated long-term arthralgia: A 36-month prospective longitudinal studyPLoS Negl Trop Dis 2013 7:e213710.1371/journal.pntd.000213723556021 [Google Scholar] [CrossRef] [PubMed]
[26]. Manimunda SP, Vijayachari P, Uppoor R, Sugunan AP, Singh SS, Rai SK, Clinical progression of chikungunya fever during acute and chronic arthritic stages and the changes in joint morphology as revealed by imagingTrans R Soc Trop Med Hyg 2010 104:392-99.10.1016/j.trstmh.2010.01.01120171708 [Google Scholar] [CrossRef] [PubMed]
[27]. Chang AY, Encinales L, Porras A, Pacheco N, Reid SP, Martins KAO, Frequency of chronic joint pain following chikungunya virus infection: A Colombian cohort studyArthritis Rheumatol 2018 70:578-84.10.1002/art.4038429266783 [Google Scholar] [CrossRef] [PubMed]
[28]. Roosenhoff R, Anfasa F, Martina B, The pathogenesis of chronic chikungunya: evolving conceptsFuture Virol 2016 11:61-77.10.2217/fvl.15.107 [Google Scholar] [CrossRef]
[29]. Tang BL, The cell biology of c94hikungunya virus infectionCell Microbiol 2012 14:1354-63.10.1111/j.1462-5822.2012.01825.x22686853 [Google Scholar] [CrossRef] [PubMed]
[30]. Lum FM, Teo TH, Lee WW, Kam YW, Renia L, NG LF, An essential role of antibodies in the control of chikungunya virus infectionJ Immunol 2013 190:6295-302.10.4049/jimmunol.130030423670192 [Google Scholar] [CrossRef] [PubMed]
[31]. Kam YW, Simarmata D, Chow A, Her Z, Teng TS, Ong EK, Early appearance of neutralizing immunoglobulin G3 antibodies is associated with chikungunya virus clearance and long-term clinical protectionJ Infect Dis 2012 205:1147-54.10.1093/infdis/jis03322389226 [Google Scholar] [CrossRef] [PubMed]
[32]. Hawman DW, Stoermer KA, Montgomery SA, Pal P, Oko L, Diamond MS, Chronic joint disease caused by persistent Chikungunya virus infection is controlled by the adaptive immune responseJ Virol 2013 87:13878-88.10.1128/JVI.02666-1324131709 [Google Scholar] [CrossRef] [PubMed]
[33]. Burt F, Chen W, Mahalingam S, Chikungunya virus and arthritic diseaseLancet Infect Dis 2014 14(9):789-90.10.1016/S1473-3099(14)70869-2 [Google Scholar] [CrossRef]