Giant Placental Chorioangioma with Severe Polyhydramnios and Foetal Anaemia- A Case Report
Harpreet Kour Isher1, Mandeep Singh2
1 Fellow Maternal Fetal Medicine, Department of Obstetrics and Gynaecology, AIIMS, New Delhi, India.
2 Clinical Director, Department of Obstetrics and Gynaecology, Southend University Hospital NHS Foundation Trust, Southend on Sea, Essex, United Kingdom.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Harpreet Kour Isher, House No. 1874, Sector 34-D, Chandigarh, India.
E-mail: harpreetsukhija1@yahoo.com
Giant placental chorioangioma is a rare, benign, vascular hamartoma of the placenta of >4-5 cm in size, since size beyond this range is associated with adverse perinatal outcome. This is a case of giant placental chorioangioma with severe polyhydramnios and foetal anemia. Serial ultrasound surveillance was able to detect foetal anemia due to the arterio-venous shunt in the chorioangioma. Severe polyhydramnios was managed with repeated amnio-reduction to relieve the mother. A non-reassuring cardiotocography and suspicion of placental abruption, following the last amnio-reduction led to an emergency caesarean. Perinatal morbidity was increased due to severe foetal anemia, coagulopathy and prematurity which was successfully managed.
Amnioreduction, Doppler, Middle cerebral artery, Ultrasound
Case Report
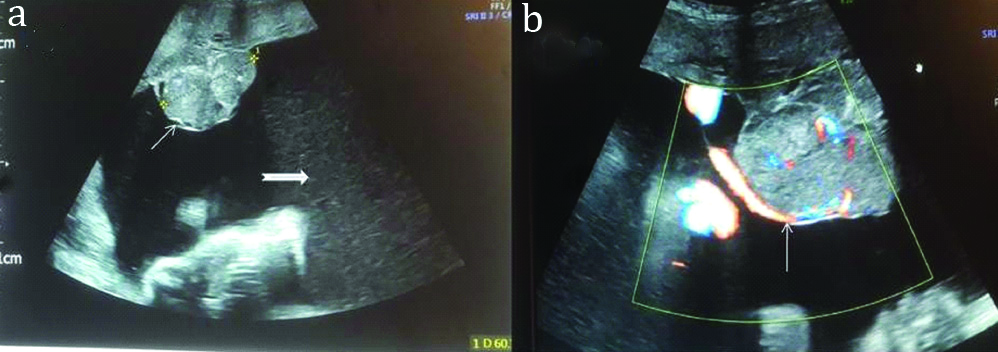
A 36-year-old, para 2, lady was referred at 28 weeks to the foetal medicine department with the diagnosis of severe polyhydramnios and placental chorioangioma. Grey scale ultrasound with color doppler imaging confirmed a well-circumscribed hypoechoic placental mass [Table/Fig-1] projecting into the amniotic cavity, close to the cord, measuring 61×57×47 mm, with both arterial and venous blood flow as well as severe polyhydramnios (single deepest pocket of 20 cm). The maternal abdomen was excessively distended (abdominal girth 120 cm). Apart from the great discomfort, all other maternal parameters including blood pressure and glucose tolerance test was normal. An appropriate for age grown foetus with no anomaly or hydrops. Doppler study of middle cerebral artery ruled out anaemia at the initial presentation.
Ultrasound picture of giant placental chorioangioma. a) Grey scale image showing chorioangioma (thin white arrow) along with increased amniotic fluid (thick white arrow). b) Colour Doppler showing the vascularity of the chorioangioma (white arrow).
Amnio-reduction was done to relieve the mother of excessive abdominal discomfort from severe polyhydramnios. Amniotic fluid analysis did not reveal any foetal chromosomal abnormality. On a repeat scan 5 days later, MCA PSV at 95th centile (1.55 MOM) suggested foetal anemia. At this stage, laser ablation to devasularize the chorioangioma, with its attendant risks was offered to the patient, which she declined. She was also given a course of antenatal steroids due to the threat of preterm labour.
Ongoing foetal surveillance with ultrasound confirmed recurrence of severe polyhydramnios necessitating repeat amnioreduction again at 30 weeks (AFI 56.4) and 33+6 weeks (AFI 33.6). Meanwhile, the foetal MCA PSV suggested foetal anemia (MCA PSV 1.62 MOM-1.48 MOM) without signs of hydrops or cardiac failure. Following the last amnioreduction, emergency caesarean was undertaken due to suspicion of placental abruption and a non-reassuring foetal heart trace pattern.
Intraoperatively, the foetus was in transverse lie with blood stained liquor. Approximately, 3L of liquor and 700 mL of blood loss was estimated. Macroscopic examination and histology of placenta confirmed the diagnosis of giant placental chorioangioma measuring 9×7×6 cm. The placenta weighed 900 gms. The baby was born pale, with apgar of 2, 6, 8 (1, 5, 10 min) and needed neonatal resuscitation . At birth, the cord (venous) gases were 7.26 BE -4.4, lactate 5.6 mmol/l and weight 2375 grams. Fetal haemoglobin was 7.4 g/dL and the baby had bleeding from stump and nasogastric tube. The baby was transfused 17 packed red cells, fresh frozen plasma and cryoprecipitate and was referred to a higher centre where she was treated for anaemia, coagulopathy, jaundice and hypoglycaemia. Haemolytic anaemia and sepsis were ruled out. She was discharged after 21 days. At one year follow-up, baby was well with no apparent neurodevelopmental delay.
Discussion
The reported incidence of giant chorioangiomas is 0.29%-0.11% [1,2]. They are associated with a perinatal mortality rate of about 40% [3-5]. Foetal complications include anemia, thrombocytopenia, non-immune hydrops, cardiac failure, growth restriction and foetal demise [3]. The central factor for the foetal complications with this vascular tumour is that it acts as an arterio-venous shunt. The feto-placental blood volume is increased and leads to increase venous return, foetal cardiomegaly, hydrops and heart failure [1]. The hyperdynamic circulation could eventually lead to foetal demise as can be in acute events like rupture of the vessels within the chorioangioma [1,3]. This shunt can compromise the functional capacity of the rest of the placenta and cause utero-placental insufficiency leading to its association with foetal growth restriction and foetal demise [3] Maternal complications include polyhydramnios leading to preterm labour, abnormal lie, premature rupture of membranes, placental abruption, and emergency caesarean and post-partum haemorrhage [1,3].
The index case presented with severe polyhydramnios due to the giant placental chorioangiomas. Polyhydramnios is the most common complication of giant placental chorioangioma and is attributed to three reasons: increased foetal urine production due to the hyperdynamic circulation, increased transudation from the abnormal tumour vasculature or increased transudation from the umbilical vein in the cord due to the mechanical compression by the commonly adjacent tumour [1,3]. In this case, the tumour was also located close to the cord. Repeated amnio-reduction was done in this patient for maternal relief due to severe polyhydramnios. However, following the third amnioreduction, placental abruption occurred which increased the foetal morbidity by adding fetomaternal haemorrhage and prematurity to the neonatal complications.
Kim A et al., also reported placental abruption with multiple rapid amnioreductions [6]. Some reports have shown that amnioreduction should be performed following vascular occlusion of feeder vessels to reduce the likelihood of further foetal deterioration [7,8]. Amnioreduction in the presence of a compromised foetal cardiac status may worsen the foetal status due to increase in the arteriovenous shunting from the reduction in the intra-amniotic pressure [1,3,4] as could have happened in this case with the last amnioreduction. This implies that the decision for amnioreduction should be judiciously taken keeping in view the risks of the procedure and the prior haemodynamic status of the foetus. Medical therapy with sulindac (cox2 inhibitors) for treating polyhydramnios has been reported at 26 weeks by Al Wattar BH et al., though it was not for severe polyhydramnios [9].
Severe foetal anemia in this case could be explained due to the dual elements of chronic sequestration of blood in the chorioangioma and placental abruption. Foetal anemia and thrombocytopenia also results from microangiopathic haemolysis within the hamartomatous capillaries [1,3,10]. However, there was no haemolysis in the baby in this case. The foetus in the present case also had coagulopathy which could be due to the same mechanism as explained in Kasabach-Merritt Syndrome where multiple microthrombi form within the tumour leading to consumptive coaguloapathy in utero [10,11].
The role of ultrasound with color Doppler imaging is indispensable in a case of giant placental chorionagioma. It also helps to differentiate from other placental masses (haematoma, teratoma) as well as in prognosticating because increased vascularity of the chorioangioma is associated with more adverse outcomes [1,2] and spontaneous thrombosis with better outcomes [3]. It is an essential modality to detect the foetal complications of anemia, heart failure and growth restriction.
The choice of prenatal intervention depends upon the gestation age, the foetal cardiac status and the resources. Amnio-reduction can be done in severe polyhydramnios best after devascularisation of the chorioangioma due to risks of placental abruption and worsening status of an anemic foetus as experienced by us. It is better to do amnioreduction after. Intrauterine transfusions to treat foetal anaemia/or hydrops, may be needed once or more depending upon gestation. Definitive treatment by devascularising the tumour has been done by various techniques with the highest success rate reported with laser coagulation by interstitial technique [12]. Other modalities as bipolar electro surgery, clip application, injection of absolute alcohol and embolisation with micro coil or enbucrilate have also been reported. One needs to be wary of the risks to the foetus which is dependent upon the technique, vascular map of the chorioangioma, position of the placenta, proximity to the cord insertion as well as status of foetal compromise [1,3]. Risks of foetal exsanguinations, collateral damage and foetal demise need to be explained to the mother.
Conclusion
The placenta should thus be evaluated critically in all case of polyhydramnios. Giant placental chorioangioma is a potentially high risk condition for both foetus and mother and its diagnosis entails follow-up with ultrasound in the antenatal period for foetal complications. The need, timing and type of any prenatal intervention requires individualisation with preparedness for acute foetal and maternal complications.
Abbreviations
MCA: Middle cerebral Artery
PSV: Peak Systolic Velocity
MOM: Multiple of Median
AS: Apgar Score
AFI: Amniotic Fluid Index
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Aug 12, 2019
Manual Googling: Sep 16, 2019
iThenticate Software: Nov 04, 2019 (3%)
[1]. Fan M, Skupski DW, Placental chorioangioma: Literature reviewJ Perinat Med 2014 42:273-79.10.1515/jpm-2013-017024334427 [Google Scholar] [CrossRef] [PubMed]
[2]. Ulkumen BA, Pala HG, Nese N, Baytur Y, Prenatal diagnosis and fetomaternal outcomes of two cases with placental chorioangiomaCase Reports in Obstetrics and Gynecology Volume 2013 Article ID 926743, 3 pages10.1155/2013/92674324251055 [Google Scholar] [CrossRef] [PubMed]
[3]. Zanardini C, Papageorghiou A, Bhide A, Thilaganathan B, Giant placental chorioangioma: Natural history and pregnancy outcomeUltrasound Obstet Gynecol 2010 35:332-36.10.1002/uog.745119859897 [Google Scholar] [CrossRef] [PubMed]
[4]. Lim FY, Coleman A, Polzin W, Jaekle R, Habli M, Van Hook J, Giant chorioangiomas: Perinatal outcomes and techniques in fetoscopic devascularizationFetal Diagn Ther 2015 37(1):18-23. Epub 2014 Aug 2810.1159/00036360025195565 [Google Scholar] [CrossRef] [PubMed]
[5]. Merry-Sperry AD, Chaffin DG, Denning KL, Shamma B, Massey C, Werthammer J, Placental chorioangioma with nonimmune hydrops FetalisSouth Med J 2018 111(8):457-59.10.14423/SMJ.000000000000084030075468 [Google Scholar] [CrossRef] [PubMed]
[6]. Kim A, Economidis MA, Stohl HE, Placental abruption after amnioreduction for polyhydramnios caused by chorioangiomaBMJ Case Rep 2018 2018:pii: bcr-2017-22239910.1136/bcr-2017-22239929507014 [Google Scholar] [CrossRef] [PubMed]
[7]. Jauniaux E, Ogle R, Color doppler imaging in the diagnosis and management of chorioangiomasUltrasound Obstet Gynecol 2000 15:463-7.10.1046/j.1469-0705.2000.00127.x11005112 [Google Scholar] [CrossRef] [PubMed]
[8]. Mendez-Figueroa H, Papanna R, Popek EJ, Byrd RH, Goldaber K, Moise KJ Jr, Endoscopic laser coagulation following amnioreduction for the management of a large placental chorioangiomaPrenat Diagn 2009 29:1277-78.10.1002/pd.240019918962 [Google Scholar] [CrossRef] [PubMed]
[9]. Al Wattar BH, Hillman SC, Marton T, Foster K, Kilby MD, Placenta chorioangioma: A rare case and systematic review of literatureJ Matern Fetal Neonatal Med 2014 27(10):1055-63.10.3109/14767058.2013.84742424460422 [Google Scholar] [CrossRef] [PubMed]
[10]. Abiramalatha T, Sherba B, Joseph R, Thomas N, Unusual complications of placental chorioangioma: Consumption coagulopathy and hypertension in a preterm newbornBMJ Case Rep10.1136/bcr-2016-21573427154993 [Google Scholar] [CrossRef] [PubMed]
[11]. Gultekin ND, Yilmaz FH, Altunhan H, Findik S, Tokgoz H, Caliskan U, Coexistence of Kasabach-Merritt Syndrome and placental chorioangioma in a premature infantJournal of Neonatal-Perinatal Medicine 2018 11(2):209-13.10.3233/NPM-18175429991142 [Google Scholar] [CrossRef] [PubMed]
[12]. Papaioannou GK, Evangelinakis N, Kourtis P, Konstantinidou A, Papantoniou N, Giant chorioangioma treated with interstitial laser coagulationUltrasound Obstet Gynecol 2018 52(2):280-81.Epub 2018 Jul 410.1002/uog.1894129072331 [Google Scholar] [CrossRef] [PubMed]