Chronic rhinosinusitis is one of the most common problems encountered in routine Otorhinolaryngological practice. Regional anatomic abnormalities and pathologies in the vicinity of OMC are frequently associated with the development of chronic sinus disease [1]. Chronic rhinosinusitis is defined as a rhinosinusitis lasting >12 weeks that includes two or more major sinus symptoms with or without findings on physical examination. Major symptoms are facial pain/pressure, nasal obstruction, nasal discharge, hyposmia/anosmia, purulence in the nasal cavity on examination. Minor symptoms are headache, halitosis, fatigue, dental pain, cough and ear pain. Septal deviation is usually associated with deformities of the midline structures. Deviated nasal septum alters nasal airflow dynamics and along with the hypertrophy of nasal mucosa it leads to increased chance of osteo-meatal complex obstruction and impaired muco-cilliary clearance [2].
OMC obstruction on the side of the septal deviation is attributed to the convexity of the septum while on the contralateral side, OMC obstruction may occur due to lateral wall mucosa or middle turbinate hypertrophy. This may consecutively lead to disease in paranasal sinuses [3]. The aim of surgical treatment of sinus disease is the complete removal of the tissues causing obstruction of the osteo-meatal complex and securing the normal ventilation. Restored ventilation leads to normal mucosal appearance and function [2].
The goal of the present study was to pre-operatively assess the cases that require FESS with septoplasty or those which can be managed with septoplasty alone, so as to avoid inconvenience of extensive surgeries and avoiding general anaesthesia. Thus, this study was undertaken to compare the results of septoplasty combined with FESS and septoplasty alone in cases of chronic rhinosinusitis.
Materials and Methods
This prospective, comparative clinical study was conducted from July 2015 to June 2016 in Tertiary Care Centre in Bareilly, Uttar Pradesh, India. All the patients presenting to Ear, Nose and Throat (ENT) Out-Patient Department (OPD) with complaints suggestive of chronic rhinosinusitis with deviated nasal septum were considered for the study. Patients with clinical or radiological sinusitis who responded to medical management with broad spectrum antibiotics, antihistamines, decongestants and topical steroids were excluded from study. Patients with history of previous nasal or sinus surgery, other associated co-morbidities like Diabetes and Hypertension were also excluded from the study. After careful assessment, a total of 50 such patients unresponsive to 3 months of medical management planned for surgery and willing to be a part of study after being fully explained about study were enrolled. Permission for the study was granted from Institutional Ethical Committee vide letter number IEC/Med/048/2015 (dated 11 June 2015).
Detailed history of all the patients was taken in the form of a proforma. The complaints and associated history was recorded and all the patients underwent a detailed ENT examination, diagnostic nasal endoscopy and CECT paranasal sinuses (coronal and axial view). With help of a computerised lottery system, patients were randomly divided into two groups of 25 patients each. Patients in Group A underwent septoplasty with FESS whereas patients of Group B underwent only septoplasty.
In Group A, where FESS was performed along with septoplasty, first septoplasty was performed as done routinely i.e., local anaesthesia was given; incision was made on deviated side of septum 2 mm behind the caudal end of nasal septum. Mucoperichondrial and mucoperiosteal flap was raised and deviated part of cartilaginous and bony septum was removed with septal scissors and if a prominent maxillary crest was present, it was chiselled out. Flap was reposited, incision was sutured and nasal packing done.
FESS was performed according to surgical technique practised worldwide starting with uncinectomy to expose middle meatus after medialisation of middle meatus. Maxillary sinus ostium was widened and all the disease was cleared and maxillary antrum was flushed with fluid. Anterior and posterior ethmoidal sinus cells were opened and cleared of disease. If disease was present in sphenoidal and frontal sinus, then sphenoidal ostium and frontal recess were widened and cleared of diseases as well.
Nasal packing was done and was removed on second post-operative day in all the patients. In Group B, Septoplasty was performed as described above.
Postoperatively, all the patients were treated with oral antibiotics, analgesics, antihistamines, decongestants, nasal douching and steroid nasal spray for 6 weeks. The follow-up of the patient was done at the end of 3rd and 6th months for the relief in nasal obstruction, nasal discharge and post-nasal drip.
Statistical Analysis
The data were collected, tabulated and analysed using statistical package for social sciences (SPSS) version 23.0. The p-values <0.05 were considered statistically significant.
Results
Age of the patients ranged from 18 to 50 years. Mean age in Group A was 23.7 years while mean age of Group B was 24.1 years. Out of 50 patients, 27 were males and 23 were females.
In both the groups, all the patient had nasal obstruction and in Group A, 19 (76%) had nasal discharge and 14 (56%) had postnasal drip while in Group B, 17 (68%) had nasal discharge and 13 (52%) had postnasal drip [Table/Fig-1]. Anterior rhinoscopy revealed deviated nasal septum with middle meatal discharge in all the patients.
| Symptoms | Group ANo. (%) | Group BNo. (%) | TotalNo. (%) |
|---|
| Nasal obstruction | 25 (100%) | 25 (100%) | 50 (100%) |
| Nasal discharge | 19 (76%) | 17 (68%) | 36 (72%) |
| Postnasal drip | 14 (56%) | 13 (52%) | 27 (54%) |
CECT scan for PNS coronal and axial view was done in all the cases. All the patients had grossly deviated nasal septum [Table/Fig-1]. Osteo-meatal complex obstruction was the most common finding in 48 (96%) patients. Mucosal hypertrophy of turbinates was seen in 28 (56%) patients and sino-nasal polypoidal changes were seen in 18 (36%) patients [Table/Fig-2]. All the patients were randomly divided into Group A and Group B of 25 patients each. Patients were followed-up at 3 months and 6 months postoperatively.
Pre-operative CECT nose and paranasal sinus findings.
| HRCT findings | Group A | Group B | Total No. (%) | p-value* |
|---|
| Unilateral No. (%) | Bilateral No. (%) | Total No. (%) | Unilateral No. (%) | Bilateral No. (%) | Total No. (%) |
|---|
| Deviated nasal septum | 10 (40%) | 15 (60%) | 25 (100%) | 12 (48%) | 13 (52%) | 25 (100%) | 50 (100%) | 0.56 (Chi-square test) |
| OMC obstruction | 14 (56%) | 11 (44%) | 25 (100%) | 16 (64%) | 07 (28%) | 23 (92%) | 48 (96%) | 0.30 (Chi-square test) |
| Turbinate mucosal hypertrophy | 07 (28%) | 06 (24%) | 13 (52%) | 08 (32%) | 07 (28%) | 15 (60%) | 28 (56%) | 0.97 (Chi-square test) |
| Polypoidal sino-nasal mucosa | 04 (16%) | 06 (24%) | 10 (40%) | 05 (20%) | 03 (12%) | 08 (32%) | 18 (36%) | 0.34 (Fisher-exact test) |
At 3rd month follow-up in Group A, nasal obstruction was seen in only 3 out of 25 patients showing 88% improvement. Nasal discharge was present in 9 out of 19 patients giving 52.64% improvement whereas only 5 out of 14 patients have residual post nasal drip showing a 64.29% relief. On the contrary in Group B, 13 out of 25 patients still complained of nasal obstruction showing only a 48% relief. Nasal discharge was present in 14 out of 17 showing improvement in only 17.65% patients whereas 7 out of 13 patients still showed post nasal drip giving improvement in 46.16% patients.
At 6th month follow-up in Group A; only 2 patients out of 25 had nasal obstruction giving 92% improvement while 3 out of 19 patients showed persistent nasal discharge showing an improvement of 84.22%. Post nasal drip was still present in 3 out of 14 patients giving an improvement of 78.58% patients. In Group B, 9 out of 25 patients still had nasal obstruction giving only 64% improvement whereas 13 out of 17 had nasal discharge showing 23.53% relief. Interestingly, post nasal drip was present in 8 out of 13 giving an improvement of only 38.47% patients. This may be due to a variety of factors including the one patient probably having an attack of acute viral rhinorrhea showing as post nasal drip [Table/Fig-3].
Symptomatic improvement after 3 and 6 months on diagnostic endoscopy.
| Symptom | Follow-up time |
|---|
| 3 months | 6 months |
|---|
| Group A | Group B | p-value (Fisher-exact Test) | Group A | Group B | p-value (Fisher-exact test) |
|---|
| Nasal obstruction | 3 (12.00%) n=25 | 13 (52.00%) n=25 | 0.003 (Mid p exact) | 2 (08.00%) | 9 (36.00%) | 0.021 (Mid p exact) |
| Nasal discharge | 9 (47.36%) n=19 | 14 (82.35%) n=17 | 0.029 (Mid p exact) | 3 (15.78%) | 13 (76.47%) | 0.0006 (Mid p exact) |
| Post nasal drip | 5 (35.71%) n=14 | 7 (53.84%) n=13 | 0.377 (Mid p exact) | 3 (21.42%) | 8 (61.53%) | 0.080 (Mid p exact) |
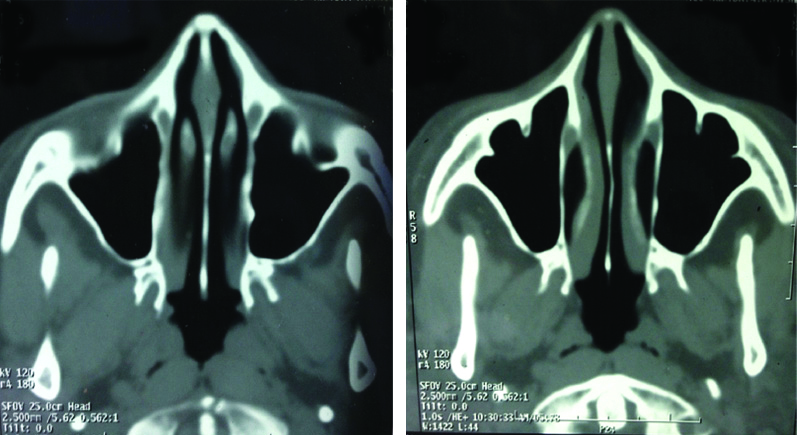
Postoperative assessment by diagnostic nasal endoscopy or CT scans in both the groups at 3 and 6 months follow-up showed midline septum [Table/Fig-4,5 and 6]. Subjectively, all the patients had significant improvement in nasal discharge and post-nasal drip.
Post-operative CECT PNS finding.
| CECT PNS findings | Type of disease |
|---|
| Unilateral | Bilateral |
|---|
| Group A | Group B | p-value (Fisher exact test) | Group A | Group B | p-value (Fisher exact test) |
|---|
| OMC obstruction | 3 (21.42%) | 6 (37.50%) | 0.2 | 2 (18.18%) | 2 (28.57%) | 1 |
| Mucosal hypertrophy | 2 (28.57%) | 2 (25.00%) | 1 | 1 (16.66%) | 2 (28.57%) | 0.55 |
| Polypoidal sino-nasal mucosa | 1 (25.00%) | 3 (60.00%) | 0.2 | 0 (00.00%) | 2 (66.66%) | 0.10 |
| Deviated nasal septum | 0 (00.00%) | 0 (00.00%) | 1 | 0 (00.00%) | 0 (0%) | 1 |
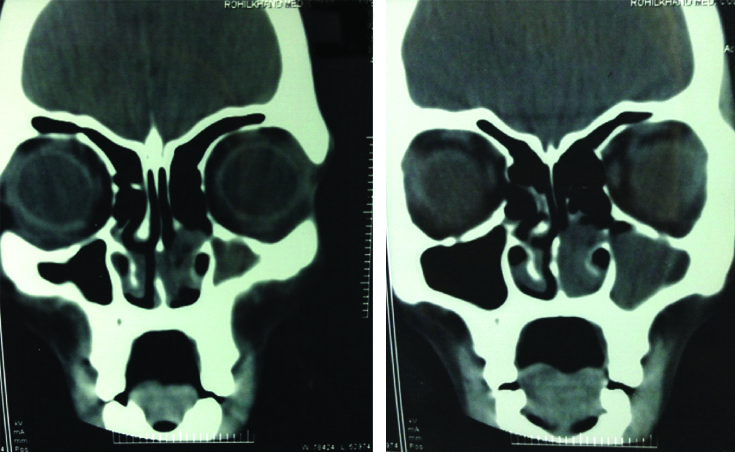
Preoperative CT scans showing DNS, bilateral inferior turbinate hypertrophy and left maxillary sinusitis.
Postoperative CT scans shows midline septum and normal paranasal sinuses.
In Group A, OMC Obstruction reduced from 14 to 3 patients in unilateral disease and from 11 to 2 in bilateral disease. Mucosal hypertrophy reduced from 7 to 2 and 6 to 1 patients in unilateral and bilateral disease respectively. Polypoidal sinonasal mucosa decreased from 4 to 1 in unilateral disease and not seen in any of the 6 patients in bilateral disease. There was less improvement in Group B in OMC obstruction, mucosal hypertrophy and sinonasal polypoidal mucosa than Group A [Table/Fig-4].
Discussion
Chronic sinusitis is one of the most common nasal problems in ENT practice. One of the reasons is obstruction caused by anatomical variations leading to mucosal hypertrophy. The maxillary sinus is the commonest to be involved due to DNS obstructing OMC [2]. Calhoun KH et al., compared 100 CT of paranasal sinuses of patients with nasal pathology with 82 scans of patients with orbital pathology and found out significant disease in the OMC of the patients with sinus disease in comparison to those with orbital pathology [4]. It was also revealed that concha bullosa and septal deviation were more commonly associated with sinus disease. Examination of these patients may reveal other findings, such as nasal allergy and polyposis which predispose to OME obstruction. Common symptoms in present study were nasal obstruction, nasal discharge and post nasal drip which is comparable to a study by Goel AK et al., Kennedy DW and Salam MA and Cable HR [2,5,6]. The clinical and radiological findings and the duration of symptoms are very important for diagnosis.
Sinha DK reported presence of mucous or mucopus in middle meatus in 76% cases in his series of 42 patients [7]. Tao Z et al., explored the influence of the deviated nasal septum on the OMC and found no difference between the incidence of sinusitis on the two sides [8]. Prasad S et al., conducted a study over 120 subjects with nasal complaints (nasal obstruction, nasal discharge, headache) [9]. It revealed male preponderance (76.6%) and no association between septal deviation and sinusitis and also that the horizontal spurs have significantly high chances of leading to sinusitis. Poorey VK and Gupta N, conducted a prospective study of 67 patients to correlate the symptoms of DNS and chronic sinusitis with findings of nasal endoscopy and computed tomography [10]. Chief symptoms of chronic sinusitis were described to be nasal obstruction (86.56%), headache (73.13%) and nasal discharge (52.23%). It was concluded that convexity of the septum results in the abnormalities in the lateral wall and turbinates which consecutively causes obstruction of the OMC and sinusitis.
The present study revealed male predominance over females as reported in a similar study by Chaitanya KV et al., [11]. Shpilberg KA et al., conducted a retrospective study to assess the relation of sino-nasal anatomic variants with the sino-nasal mucosal disease [12]. The CT scans of 192 patients with rhinosinusitis were evaluated and the prevalence of each variation was calculated. Prevalence of the variants was compared to the patients with radiologically evident rhinosinusitis and with patients who had no evidence of rhinosinusitis. Septal deviation, agger nasi cells and extension of the sphenoid sinus in the posterior nasal septum were revealed to be the most common variants. Bagri N et al., evaluated 130 patients to study the relation of angle of septal deviation with abnormalities of the lateral wall and mucosal disease of the paranasal sinuses and revealed that the severity and direction of deviation of the septum directly affects the contralateral turbinates [13].
Thakur K et al., in their study concluded that septoplasty is effective for the treatment of CRS patients with deviated nasal septum on VAS and Lund Mackay staging system than FESS alone [14]. In his study, Chaitanya KV et al., observed that when FESS was done without correcting the anatomical abnormalities like deviated nasal septum, there was 20.62% incidence of residual or recurrent disease. In this study, when pre and post-operative quality of life improvement was tabulated using SNOT 22 symptoms, there was more improvement when septoplasty was performed along with FESS. Similar studies conducted by Bayiz U et al., and Goel AK et al., are of strong opinion that septoplasty alone can be adequate in treating CRS with DNS, but they also concluded that in cases of CRS where polyps are present, then septoplasty with concomitant FESS was the better way of helping the patient get relieved of symptoms [15,16].
Similar findings were reported by Satish SH and Sreedhar KT [17] who reported improvement in SNOT 22 score after performing septoplasty alone. They concluded that septoplasty alone is relevant in cases where anatomical distortions are present and its correction can help reduce symptoms of majority of cases.
These studies are in contrast to the present study which clearly shows that patients who underwent only septoplasty had a lot of residual symptoms post-operative as well as on 3 and 6 months follow-up in comparison to those who underwent concomitant FESS and septoplasty.
Limitation
The study has its limitations as it has a follow-up period of only 6 months. Chronic diseases like CRS often have a slow course and so studies with a long follow-up need to be undertaken. Also a larger sample size would increase the variability of symptoms and understanding of problem in terms of an effective surgical outcome with minimal surgical intervention and adequate disease improvement.
Conclusion
Presence of deviated nasal septum with limited sinus disease, performing septoplasty alone is not justified, but FESS must be concomitantly combined with septoplasty in cases of deviated nasal septum with polypoidal sinus mucosa and osteo-meatal complex pathology.