Migration of Thecoperitoneal Shunt into a Hernial Sac
Yeshwant Lamture1, Varsha Gajbhiye2
1 Professor, Department of Surgery, JNMC, Wardha, Maharashtra, India.
2 Associate Professor, Department of Surgery, JNMC, Wardha, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Yeshwant Lamture, JNMC, Wardha, Maharashtra, India.
E-mail: dryrlamture@yahoo.co.in
Thecoperitoneal shunts are commonly used to treat several conditions, but their use can result in significant complications like migration of it in hernial sac. Only few cases of scrotal migration of shunt is reported. This case report is about a middle aged gentleman, presented with irreducible right sided inguinal hernia. He was subjected to emergency surgery and found to have omentum and thecoperitoneal shunt as a content.
Early surgical removal is recommended for catheters remaining in the abdomen or in scrotum after thecoperitoneal shunt migration. These tubing can cause injury to the testicle, or other abdominal viscera.
Cerebrospinal fluid leakage, Hydrocephalus, Irreducible hernia
Case Report
A 60-year-old farmer presented with right sided non-reducible inguinal swelling since five hours. The swelling has been recurring since one year but was reducible.
The patient gave history of spinal surgery for disc prolapsed, three years back. After surgery he developed Cerebrospinal Fluid leakage (CSF) from the operative site. To treat this CSF leak, a thecoperitoneal shunt was placed.
On clinical examination, there was a right-sided inguino-scrotal swelling reaching the bottom of scrotum; it was non-reducible, firm in consistency and cough impulse was present. Getting above the swelling was not possible. There was a linear scar on lower back suggesting the past surgery of spine.
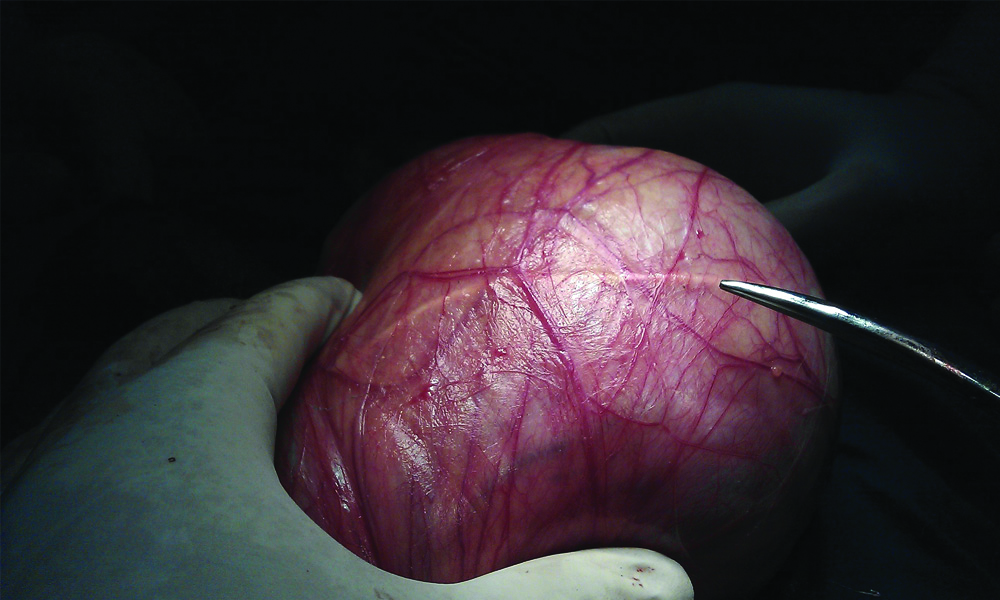
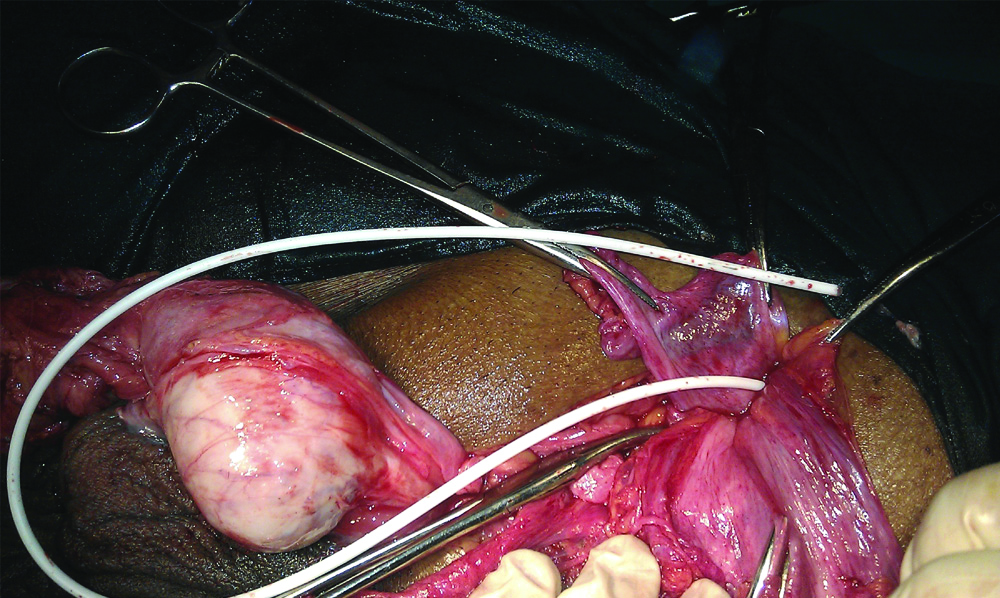
A diagnosis of right-sided irreducible inguinal hernia was done and the patient was posted for surgery. Perioperatively, a hernia sac was found containing omentum and tubing of thecoperitoneal shunt [Table/Fig-1,2]. The omentum was not reducible because of adhesions at neck of the sac. Adhesinolysis was done and omentum was reduced. The migrated shunt had its other end lying free into the abdomen. As the CSF leak had already stopped despite the shunt lying outside, it was removed. Herniotomy with hernioplasty was done after reduction of omentum.
Showing intact sac of hernia with tubing of thecoperitoneal shunt.
Showing open sac of hernia with tubing of thecoperitoneal shunt.
Patient had an uneventful post-operative recovery. He was followed for six months to detect any complication like CSG leak, recurrence of hernia etc but there was none.
Discussion
The thecoperitoneal shunt (arachnoid peritoneal shunt, lumbar peritoneal shunt) was introduced in 1905 as a treatment for hydrocephalus. In its simplest form, it consists of a plastic tubing without valves through which CSF drains from the lumbar sub-arachnoid space to the peritoneal cavity. This is only appropriate for communicating type of hydrocephalus. Despite the development of valve system including a reservoir the popular design remains; that of a simple tube between thecal sac and the peritoneal cavity [1].
Communicating hydrocephalus due to infective diseases like tuberculosis or bacterial infection is common in India, while it is more frequent following sub-arachnoid haemorrhages in western countries. Shunt surgery is performed in such a condition. Thecoperitoneal shunt has the advantage of being an entirely extra cranial operation [2].
The thecoperitoneal shunts are entirely extra cranial, very effective and safe for treating communicating hydrocephalous compared to the Ventriculo-Peritoneal (VP) shunt. The thecoperitoneal shunt is also effective in some non-hydrocephalous conditions like CSF leaks [3]. In present case, thecoperitoneal shunt surgery was done to treat the same condition (CSF leak).
Though the surgery of thecoperitoneal shunt is rewarding but not without hazards, many complications are documented. Most common complications of this procedure are shunt block, infections, CSF leakage, cerebellar tonsil herniation followed by death, sudden visual loss due to an acute rise of intracerebral pressure in a blocked shunt, radicular leg pain, dyspnoea, and disturbance of consciousness that necessitates conversion to a VP shunt in patients who subsequently are noted to have Chiari malformations, and intracranial bleeding, acute subdural haematoma and migration of shunt in pelvis and in sub-arachnoid space [4]. Migration of thecoperitoneal shunt in hernial sac is very rare event [5]. Only less than 40 cases have been reported of scrotal migration of distal end of the shunt, till 2016 [6]. The present report is of migrated thecoperitoneal shunt and it was found as a content of the hernial sac.
Rajendran B et al., reported a case of a three-year-old child with a right sided hydrocele with the distal end of the VP in scrotum, 3 years after a VP shunt surgery for congenital hydrocephalus [6]. Present case also had migration of distal end of shunt in scrotum.
Ricci C et al., presented a case report of migration of 2 VP shunt catheters to the scrotum similar to the index case [7]. They described a case of 10-year-old male with a history of hydrocephalus operated for VP shunt placement for three times. Two catheter were migrated in scrotum, one was entangled and fibrosed to the testis. A second shunt tubing was also in the scrotum.
Gupta M et al., also reported a similar case of migration of the peritoneal catheter of a VP shunt into the scrotum [8]. This procedure was done in a two-year-old boy with congenital hydrocephalus. The patient was operated, and hernial sac containing a VP shunt was reduced and herniotomy was performed.
The VP shunt can migrate to scrotum. This migration may cause secondary hydrocele, blockage of catheter, and shunt malfunction. These complications leads to worsening of the hydrocephalus or CSF leak [6], hence early removal is recommended.
Conclusion
In the present case, patient had a right sided irreducible inguinal hernia with omentum and shunt tubing as a content of it. Early surgical removal is recommended for catheters remaining in the abdomen or in scrotum after thecoperitoneal shunt migration. These tubing can cause injury to the testicle, or other abdominal viscera.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Sep 09, 2019
Manual Googling: Oct 30, 2019
iThenticate Software: Nov 02, 2019 (12%)
[1]. West CG, Grebbell FS, A means of assessing theco-peritoneal shunt patencyBr J Radiol 1980 53(631):647-49.10.1259/0007-1285-53-631-6477426885 [Google Scholar] [CrossRef] [PubMed]
[2]. Yadav YR, Parihar V, Agarwal M, Lumbar peritoneal shunt in idiopathic intracranial hypertensionTurkish Neurosurgery 2012 22(1):21-26.10.5137/1019-5149.JTN.4307-11.122274966 [Google Scholar] [CrossRef] [PubMed]
[3]. Yadav YR, Pande S, Raina VK, Singh M, Lumboperitoneal shunts: Review of 409 casesNeurol India 2004 52(2):188-90. [Google Scholar]
[4]. Chumas PD, Armstrong DC, Drake JM, Tonsillar herniation: The rule rather than the exception after lumboperitoneal shunting in pediatric populationJ Neurosurg 1993 78:568-73.10.3171/jns.1993.78.4.05688450330 [Google Scholar] [CrossRef] [PubMed]
[5]. Aoki N, Lumboperitoneal shunt: Clinical applications, complications, and comparison with ventriculoperitoneal shuntNeurosurgery 1990 26(6):998-1003.10.1227/00006123-199006000-000132362678 [Google Scholar] [CrossRef] [PubMed]
[6]. Rajendran B, Sriram PR, Arumugam A, Herniotomy alone as treatment for scrotal migration of ventriculoperitoneal shuntJ Head Neck Spine Surg 2019 3(5):555623 [Google Scholar]
[7]. Ricci C, Velimirovic BM, Fitzgerald TN, Case report of migration of 2 ventriculoperitoneal shunt catheters to the scrotum: Use of an inguinal incision for retrieval, diagnostic laparoscopy and hernia repairInt J Surg Case Rep 2016 29:219-22.10.1016/j.ijscr.2016.11.00227883967 [Google Scholar] [CrossRef] [PubMed]
[8]. Gupta M, Goyal S, Agrawal A, Migration of the peritoneal catheter of a ventriculoperitoneal shunt into the scrotumSouth African Journal of Child Health 2012 6(3):93-94.10.7196/sajch.386 [Google Scholar] [CrossRef]