Maxillary first molars are distinguished for their numerous anatomical variations including the single root with a single canal, the presence of additional canals or the fusion. Fusion is an uncommon morphological variation that often occurs in deciduous anteriors but in the permanent maxillary first molars, it is rarely observed. Management of such diversions requires magnification, refinement in every step such as in access cavity preparation, cleaning-shaping and modification in the technique of obturation. The reported case enlightens the endodontic management of maxillary first molar exhibiting the fusion with the supernumerary tooth diagnosed using a Cone-Beam Computed Tomography (CBCT).
Anatomic variation, Dental loupe, Fusion, Supernumerary tooth
Case Report
A 26-year-old healthy male patient was referred by a private dental practitioner to the Department of Conservative Dentistry and Endodontics with a complaint of spontaneous, throbbing pain in the maxillary right first molar region. The referring dentist reported that during the caries excavation on the mesial side of the tooth #16 and the supernumerary tooth, the carious exposure of the pulp was evident in the supernumerary tooth and hence, he initiated the root canal treatment of that tooth. However, after the initiation of the root canal treatment, the patient’s symptoms were exaggerated and hence the patient decided to undergo the extraction of the supernumerary tooth. After the unsuccessful attempt of the extraction of an extra tooth because of fusion on the Mesiobuccal (MB) aspect with the tooth #16 and due to continuous severe pain, the patient was referred to our Department for further opinion and treatment of the supernumerary tooth and tooth #16.
Clinical examination revealed a small additional, fractured cusp on the buccal aspect of the MB cusp of tooth #16 [Table/Fig-1a]. Though there was a definitive occluso-gingival groove evident between the supernumerary tooth and the buccal cusps of tooth #16, the fusion of teeth was distinctly marked.
a) Preoperative photograph showing the bilateral fusion of tooth #16 and tooth #27 with the supernumerary teeth. (b) Preoperative IOPA radiograph revealed an uncleared supernumerary tooth outline with tooth #16. (c,d) Preoperative CBCT scans confirmed the fusion of tooth #16 with the supernumerary tooth. (e) A 3-D constructed image of tooth #16 showing fusion with the supernumerary tooth.
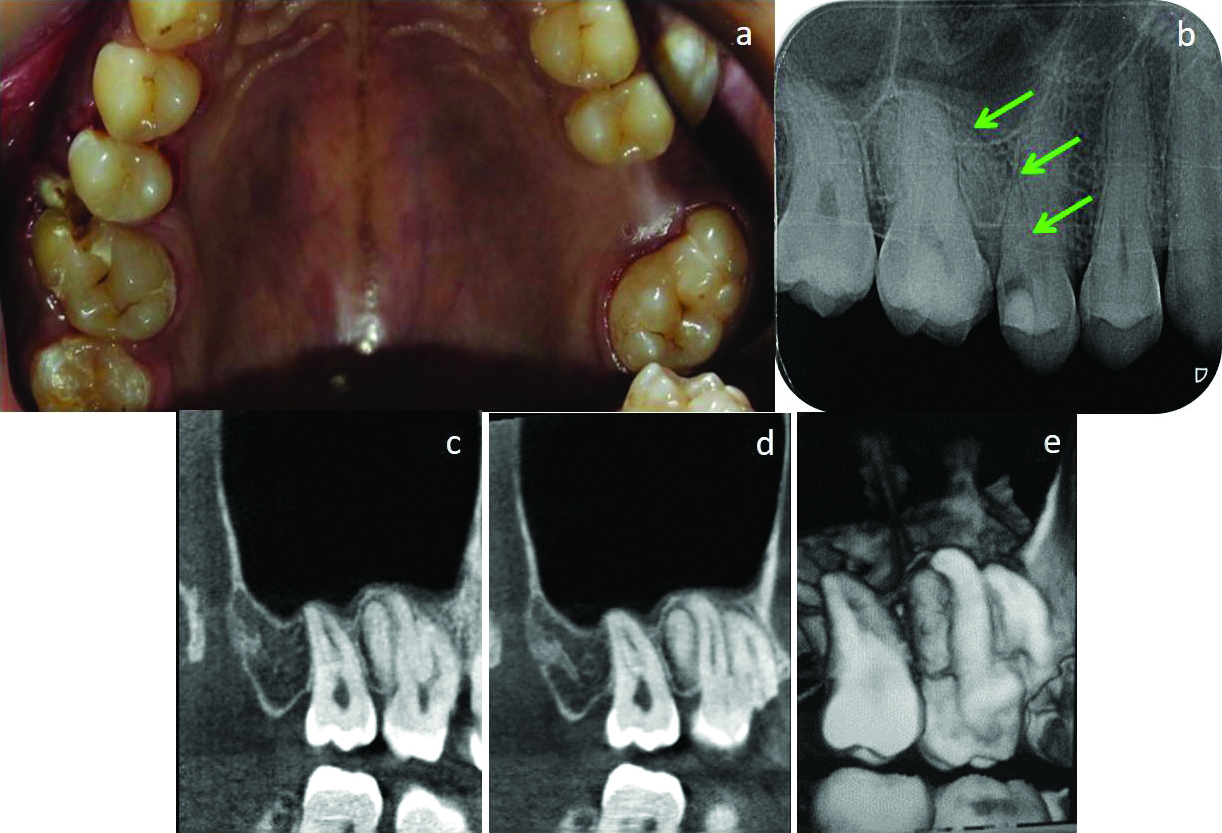
Intraoral Periapical (IOPA) radiographic examination could not reveal the exact anatomy of the tooth #16 and presented as unclear supernumerary root shadow between teeth #15 and #16 [Table/Fig-1b]. Mesial caries was present in tooth #16 and the composite restoration was evident in tooth #15. To rule out exact root canal anatomy of concerned tooth CBCT scan of tooth #16 was advised. Informed consent of the patient was obtained for the scan and further treatment. A 3-dimensional (3-D) scan [Table/Fig-1c,d] and reconstructed images of the tooth #16 [Table/Fig-1e] were also formed which exhibited its fusion with the supernumerary tooth. CBCT scans at cervical, middle and apical third sections of roots were taken of tooth #16 [Table/Fig-2a-c] which revealed; two separate pulp chambers, a single canal in supernumerary tooth and three separate canals i.e., Mesiobuccal (MB), Distobuccal (DB) and Palatal (P) canal in tooth #16. Clinically, tooth #16 showed an increased response to the electric pulp test, cold test and the tooth was tender to percussion test. The tooth #16 having fusion was diagnosed with symptomatic irreversible pulpits with apical periodontitis and advised an endodontic treatment.
(a,b,c) Preoperative CBCT horizontal sections at coronal (a); middle (b); and apical third (c) of the tooth #16 showing fusion. (d) Modified access cavity preparation after the split-dam application in tooth #16. (e) Working length IOPA radiograph of tooth #16. (f) Post-obturation IOPA radiograph of tooth #16.
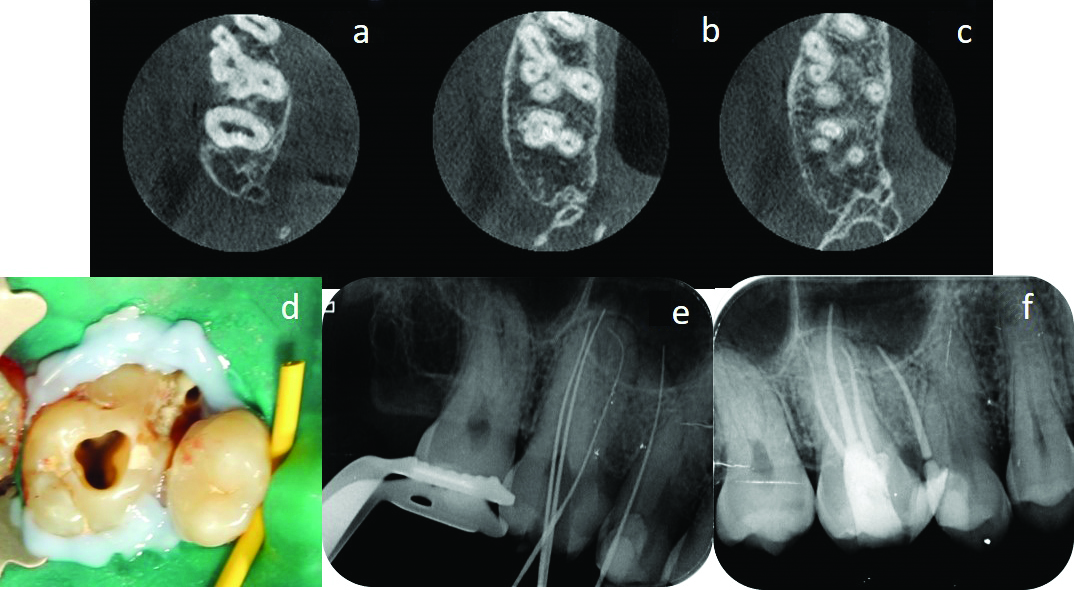
Clinically, due to the unusual crown morphology of the tooth #16, routine Rubber Dam (RD) isolation became difficult. Thus, the split-dam technique of isolation was used and margins of the rubber dam near the tooth were sealed using light cure resin barrier material (Opal Dam, Ultradent Products, Inc.). RD clamp was placed on tooth #17 and wedjets were placed between the tooth #15 and tooth #14 to stabilise the RD sheet. Following the conventional access cavity preparation using 3.5x magnification under dental loupes; the access cavity was modified to gain the entry into the root canal of the supernumerary tooth [Table/Fig-2d].
Root canals were negotiated and the glide path was established using no. #10K file (Mani Inc., Japan). Working length was measured using IOPA radiograph [Table/Fig-2e] and confirmed with Root Zx apex (J. Morita, Tokyo, Japan) locator. Coronal orifices were enlarged using Gates Glidden drill no.# 2 and no.#3. All the root canals were cleaned and shaped with Protaper gold rotary files (Dentsply Maillefer) upto #F1 (MB and DB canals) and #F2 (Palatal canal and root canal of supernumerary tooth). The root canals were sequentially irrigated with 3% sodium hypochlorite (Prime Dental, India) followed by saline and 17% Ethylene-diamine-tetra-acetic acid (EDTA) solution. Final rinsing of the canals was done using saline and 2% chlorhexidine solution. During the preparation of root canals, the irrigating solution of sodium hypochlorite was agitated with Endo-activator tip (Dentsply Tulsa, Dental Specialities). The root canals were dried with corresponding sized absorbent paper points (Dentsply). The root canal walls were then coated with AH Plus resin sealer and warm vertical compaction of the gutta-percha was done with the heated plugger. The access cavity was restored with Cavit G temporary restorative material. The postoperative IOPA radiograph was taken and the patient was scheduled for the permanent restoration [Table/Fig-2f] but, he didn’t report back.
Discussion
Endodontics is one of the specialities of dentistry dedicated for saving the pulpally involved natural teeth by preventing infection or re-infection or by treating the existing apical pathology. Knowledge of tooth morphology, root canal anatomy with their variations is essential for endodontic success. Presence of unusual, aberrant anatomy or anomalies in the teeth may complicate the endodontic treatment and compromises the tooth prognosis.
Maxillary first molars play a significant role in the mastication, the establishment of the arch perimeter, development as well as the determination of the occlusion. They usually have three roots and four canals. Their canal morphology has shown alteration in the root canal numbers which may vary from 1 canal to 8 canals or C-shaped single canal configuration or may be presented with the taurodontism or the fusion [1-4].
In the presented case, clinically tooth #27 also showed similar crown anatomy as that of tooth #16, demonstrating suspected fusion. An IOPA radiograph of the tooth #16 showed a supernumerary tooth which gave rise to the suspicion of the possibility of its fusion with the over-retained root of the deciduous second molar or its fusion with the supernumerary tooth.
Fusion occurs when the crown of teeth is not yet mineralized and the union of 2 or more separately developing tooth germs at the dentinal level forming a single large tooth during odontogenesis process with dentin confluence [5]. The fusion may also occur between the two normal teeth or between the normal tooth and the supernumerary tooth.
The incidence of fusion in permanent teeth is rare about 0.1% whereas; in deciduous dentition, it is about 0.5%-2.5% [6,7]. In one study in India, the reported incidence of fusion was 0.18% [8]. Unilateral fusion is more common than its bilateral appearance. Fusion when occurs between two normal teeth, the crown appears bigger but when the fusion occurs between the normal tooth and the supernumerary; the resultant fused tooth shows a bulbous crown with a small groove in between the two teeth [6]. In the fused tooth pulp chamber or canal may be either fused or separated and it is mainly dictated by the stage of tooth development during fusion. Fusion is more common between maxillary lateral and central incisor and between two mandibular incisors. Various syndromes have also been associated with fusion such as; Down’s syndrome, Robinow syndrome and Rubinstein Taybi syndrome etc., [9]. Similarly, the supernumerary teeth are usually associated with the syndromes namely cleft lip and palate, Cleido-cranial dysostosis, Gardner’s syndrome and Chondro-ectodermal dysplasia, but non-syndromic supernumerary teeth were also reported in the literature [10].
IOPA radiograph shows a 2-dimensional image (2D) of the 3-dimensional (3D) object and may not help to identify anatomical variation all the times. Thus, the use of CBCT become advantageous which may provide images with low radiation doses and at a lower cost when compared with other CT imaging techniques used in endodontics [11]. CBCT image provides a clear picture of root canal anatomy, adjacent hard and soft tissues which enables the clinician to understand and study the root canal configuration for proper access cavity preparation, canal instrumentation and obturation of the root canals more effectively [12]. In this case, the CBCT scan of the concerned tooth revealed the fusion between the coronal aspect of tooth #16 and the supernumerary tooth, while their roots were distinct and separated.
A similar case of fusion between the maxillary first molar and a supernumerary tooth was reported by Song CK et al., [4]. In this case, though there was a clinically distinct developmental occluso-gingival groove seen between the supernumerary tooth and the molar; there was no discernible separation between them. The CBCT scan showed the supragingival communication between the supernumerary tooth and distobuccal root and the two teeth showed the continuity of the root canals, started 2 mm below the cement-enamel junction and extended throughout the length between the canal of the supernumerary tooth and the distobuccal canal of the maxillary first molar. The communication between the supernumerary tooth and the maxillary first molar was then repaired using flowable resin [4].
In the presented case, the split dam technique of isolation was applied as the unusual crown morphology of tooth #16 restricted the use of routine rubber dam isolation [13]. This method is usually advocated in teeth with insufficient crown height, mutilated teeth with sub-gingival margins, partially erupted teeth or teeth with unusual crown morphology and where standard rubber dam isolation technique is inadequate. In this technique, two holes were punched into the rubber dam sheet adjacent to the tooth being isolated. A slit was cut to join these two holes and the rubber dam sheet was placed with the help of clamp and wedges or wedjets (Coltene/Whaledent, Cuyahoga Falls, Ohio). As this split offers poor isolation with logging of the irrigating solution or saliva in the nearby area; the margins of the rubber dam sheet were sealed by light-cured resin gingival barrier material [13].
Whenever there is clear, distinct dentinal wall present between two teeth at the line of fusion and one is involved with endodontic infection, the clinician must evaluate the pulp vitality status of both the teeth separately. In cases where there is pulpal involvement of supernumerary tooth; it should be treated with endodontic treatment and the vitality of the normal tooth must be preserved. But in our case, as pulp was exposed of the supernumerary tooth and the associated tooth was tender to percussion test; endodontic treatment of both was advised. Clinically, when the fusion or an extra root or/and an additional groove in the root is present, it may lead to the formation of an undesirable bony defect with the loss of an epithelial attachment. Performing surgical procedures like root planing, hemisection or root resection may pose access difficulties and unfavourable conditions.
Conclusion
Maxillary first molars are acclaimed for their numerous anatomical variations and every effort must be taken to search for the presence of additional roots, canals or anomalies to avoid failures. Use of multi-angulated IOPA radiographs and CBCT scans are potential diagnostic aids to rule out the unusual anatomic variations. To treat such anomalies the magnifying tools such as dental loupes or DOM may be used as well as additional changes must be incorporated during the isolation, access cavity preparation, cleaning-shaping and obturating the canals optimally in three dimensions.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Sep 02, 2019
Manual Googling: Oct 25, 2019
iThenticate Software: Nov 02, 2019 (15%)
[1]. Kottoor J, Velmurugan N, Sudha R, Hemamalathi S, Maxillary first molar with seven root canals diagnosed with cone-beam computed tomography scanning: a case reportJ Endod 2010 36(5):915-21.10.1016/j.joen.2009.12.01520416446 [Google Scholar] [CrossRef] [PubMed]
[2]. Almeida G, Machado R, Sanches Cunha R, Vansan LP, Neelakantan P, Maxillary first molar with 8 root canals detected by CBCT scanning: a case reportGen Dent 2015 63(2):68-70. [Google Scholar]
[3]. Joshi C, Joshi S, C-shaped canal in maxillary first molars: A case reportJournal of Dentistry 2014 11(1):111-17. [Google Scholar]
[4]. Song CK, Chang HS, Min KS, Endodontic management of supernumerary tooth fused with maxillary first molar by using cone-beam computed tomographyJ Endod 2010 36(11):1901-04.10.1016/j.joen.2010.08.02620951310 [Google Scholar] [CrossRef] [PubMed]
[5]. Garattini G, Crozzoli P, Brenna F, Bilateral dental fusion of the upper central incisors: a multidisciplinary approachJ Esthet Dent 1999 11:149-54.10.1111/j.1708-8240.1999.tb00392.x10825872 [Google Scholar] [CrossRef] [PubMed]
[6]. Hülsmann M, Bahr R, Grohmann U, Hemisection and vital treatment of a fused tooth- literature review and case reportEndod Dent Traumatol 1997 13:253-58.10.1111/j.1600-9657.1997.tb00051.x9558505 [Google Scholar] [CrossRef] [PubMed]
[7]. Blaney TD, Hartwell GR, Bellizzi R, Endodontic management of a fused tooth: A case reportJ Endod 1982 8:227-30.10.1016/S0099-2399(82)80359-2 [Google Scholar] [CrossRef]
[8]. Shashirekha G, Jena A, Prevalence and incidence of gemination and fusion in maxillary lateral incisors in odisha population and related case reportJ Clin Diagn Res 2013 7(10):2326-29. [Google Scholar]
[9]. Jain PS, Gupte TS, Jetpurwala AM, Dedhia SP, Robinow syndrome and fusion of primary teethContemp Clin Dent 2017 8(3):479-81.10.4103/ccd.ccd_622_1729042739 [Google Scholar] [CrossRef] [PubMed]
[10]. Anand Nayak UA, Mathian VM, Veerakumar Non-syndrome associated multiple supernumerary teeth: a report of two casesJ Indian Soc Pedod Prev Dent 2006 24:11-14. [Google Scholar]
[11]. Hassan B, Metska ME, Ozok AR, van derStelt P, Wesselink PR, Detection of vertical root fractures in endodontically treated teeth by a cone beam computed tomography scanJ Endod 2009 35:719-22.10.1016/j.joen.2009.01.02219410091 [Google Scholar] [CrossRef] [PubMed]
[12]. La SH, Jung DH, Kim EC, Min KS, Identification of independent middle mesial canal in mandibular first molar using cone-beam computed tomography imagingJ Endod 2010 36:542-45.10.1016/j.joen.2009.11.00820171380 [Google Scholar] [CrossRef] [PubMed]
[13]. Liebenberg WH, Extending the use of rubber dam isolation: Alternative procedures- Part IIQuintessence Int 1993 24(1):07-17. [Google Scholar]