The knowledge of oral lesions is essential for adequate diagnosis and correct treatment [1]. Oral white lesions are evidenced by the presence of whitish patches located in the oral cavity, many of them with malignant potential. Their aetiology is extremely diverse and certain lesions do not present one single cause, but result from the interaction of several factors [2]. A recent study suggests that the dentists should be able to recognise the white lesions of the oral cavity to establish their correct diagnosis, selecting an appropriate treatment for each type of lesion [3].
Although there are several classifications regarding white lesions, the present study adopted the criterion of superficial keratinization. According to Neville BW et al., this classification divides white lesions into two large groups: non-scrapable and scrapable [4]. In the first group, special attention should be given to leukoplakia, lichen planus, nicotine stomatitis, frictional keratosis, actinic cheilitis, and hairy tongue. The scrapable group emphasizes thermal and chemical burns, and candidiasis [5-7].
All white lesions should be biopsied if malignancy is suspected or when they do not respond to conservative treatments. For small areas of leukoplakia, excisional biopsy is usually appropriate. For larger lesions, incisional biopsy is preferable. Hyperkeratotic lesions may be monitored in the long term, with re-excision performed in case of any change in size or appearance. Lesions characterised by dysplasia and carcinoma in situ should be completely excised to clear the margins when possible [3,5,8].
For patients with history or carriers of cancerous lesions, regardless of the type, follow-up is mandatory to assess lesion recurrences and, if necessary, to perform a new surgical-therapeutic intervention [9]. Similarly, it is extremely important to computerise and use the dental documentation on lesions/normality changes through the clinical data to understand the diagnosis/treatment process. Filling the dental records correctly helps identifying the lesions, comparing pre- and post-operative periods, and verifying the effectiveness of a treatment; it also represents a legal means for the dentist to conduct his work and protect himself judicially [1].
Dogenski LC et al., performed a study at the School of Dentistry of the University of Passo Fundo, prior to the present study, seeking to focus on an overview of all oral lesions, between March 2015 and June 2017 [1]. The present study was conducted at the same school, but evaluated only patients with oral solitary white lesions treated between July 2017 and June 2019. It is important to note that the patients analysed in the study conducted by Dogenski DC et al., were not included in the present study [1]. Thus, the difference between the populations of the two studies is in the period analysed, in the patients who participated in the study and in the sample selection criteria.
The present study aimed to describe the profile of a series of white lesions of the oral mucosa treated at the School of Dentistry of the University of Passo Fundo, RS, Brazil, for two years. The results of this study are important for elaboration of public health policies because it allows the clinician to know in detail the white lesions of oral mucosa.
Materials and Methods
The present study was a retrospective study. The Research Ethics Committee of the University of Passo Fundo, RS, Brazil, approved the present study (Opinion #158.990).
The initial sample consisted of 3,000 patients treated at the Faculty of Dentistry of the University of Passo Fundo, RS, Brazil, from July 1, 2017 to June 30, 2019. Of the 3,000 patients whose records were analysed, 1,829 (60.96%) were women and 1,171 (39.04%) were men. Of the initial sample, were cataloged 36 solitary white oral lesions, without the presence of another lesion (1.2%). It is noteworthy that this research was based only on the analysis of medical records and not on the clinical analysis of the patients. So, all patients records with scrapable and non-scrapable white lesions of the oral mucosa assisted at the School of Dentistry of the University of Passo Fundo were included in the study within two years.
Patients were assessed for age, sex, ethnicity, geographical origin, and smoking habits and/or alcoholism. The respective lesions were assessed for clinical and/or histopathological diagnosis, treatment, aetiology, surface keratinization, and evolution time.
All medical records of patients with white oral lesions (scrapable or not), without the presence of another lesion, treated at the Faculty of Dentistry were included in the study. To be included in the study, lesions should have their clinical or histopathological diagnosis available on the patient’s record (depending on the type of lesion). Cases with incomplete medical records who did not allow filling the database were excluded. Cases of white lesions associated with another lesion were also excluded. Thus, nine cases were excluded from the study because they did not present complete data in the patients’ medical records, and seven cases were excluded for presenting white lesions associated with red lesions. Thus, the final sample size (eligible for the study) was 36 patients with oral white lesions (24 non-scrapable lesions and 12 scrapable lesions).
Statistical Analysis
Data collected were entered into Microsoft Excel spread sheet and analysed using SPSS version 23.0 software. Continuous data were expressed in frequencies and percentage. Chi-square test was used to compare categorical variables at 95% significance level.
Results
The variables analysed in the study are described in [Table/Fig-1].
Variables and respective categories analysed in the present study.
| Variables | Categories |
|---|
| Age group | Continuous in years |
| Sex | Male or Female |
| Ethnicity | White or Black |
| Geographic location | Northwest of the state of Rio Grande do Sul, Brazil |
| Southwest of the state of Rio Grande do Sul, Brazil |
| Northeast of the state of Rio Grande do Sul, Brazil |
| Smoking (all forms) | Yes |
| No |
| Alcoholism | Yes |
| No |
| Diagnosis (clinical and histopathological) | Fissured tongue |
| Lichen planus |
| Geographic tongue |
| Traumatic ulcer |
| Linea alba |
| Nicotine stomatitis |
| Candidiasis |
| Frictional keratosis |
| Actinic cheilitis |
| Treatment | Oral hygiene instruction |
| Prosthetic adjustment |
| Incisional biopsy |
| Topical corticoid |
| Laser therapy |
| Excisional biopsy |
| Antifungal agents |
| Sunscreen and lip moisturizer |
| Stop smoking |
| Occlusal traumatic factor removal |
| Use of wide hat to protect against the sun |
| Application of 50% glucose |
| No treatment required (some lesions clinically do not require treatment, such as linea alba or geographic tongue) |
| Aetiology | Chronic trauma |
| Smoking |
| Fungal infection |
| Autoimmune origin |
| Stress |
| Excessive sun exposure |
| Surface | Non-scrapable |
| Scrapable |
| Evolution time of the lesion in months | Up to 3 months |
| More than 3 months |
| No information |
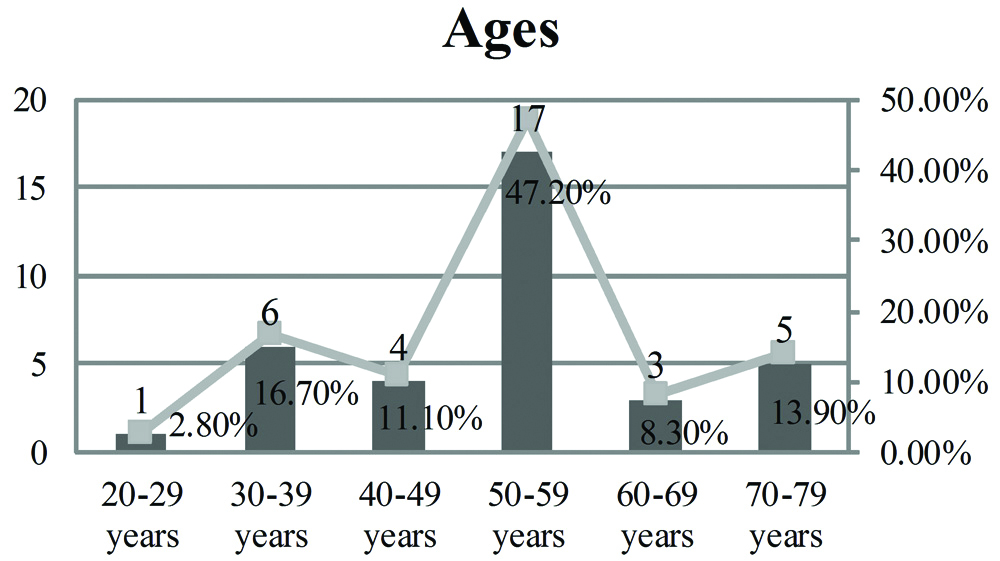
Of the 36 cases of white lesions found, 24 (66.67%) corresponded to non-scrapable lesions and 12 (33.33%) corresponded to scrapable lesions. [Table/Fig-2] shows the distribution of patients studied in terms of age. Regarding the gender of patients with oral white lesions, 25 (69.4%) were men and 11 (30,6%) were women. As for ethnicity, 31 (86.1%) cases occurred in white people and five (13.9%) cases in black people.
Distribution of patients analysed for age group (number of lesions were statistically higher in the sixth decade of life; p=0.002, Chi-square test).
There was a statistically significant relationship of the sex of patients with smoking habits (all forms) and alcoholism, showing that men presented more of these habits than women [Table/Fig-3].
Distribution of patients analysed regarding smoking habits (all forms) and alcoholism.
| Smoking | Alcoholism | p-value (Chi-square test) |
|---|
| Yes | No | Yes | No |
|---|
| Men | 14 | 11 | 06 | 19 | 0.001 |
| Women | 03 | 08 | 03 | 08 | |
| Total | 17 | 19 | 09 | 27 | |
Regarding the diagnoses obtained for white lesions, the three most striking were actinic cheilitis, lichen planus, and frictional keratosis [Table/Fig-4]. Considering the cancerous lesions included in the sample, there was a significant presence in the sixth decade of life [Table/Fig-5]. There was also a significantly higher presence of nicotine stomatitis, actinic cheilitis, and candidiasis in smokers [Table/Fig-6].
Absolute number and percentage of white lesions regarding the diagnoses.
| Diagnosis | Frequency | Percentage |
|---|
| Fissured tongue | 1 | 2.8% |
| Linea alba | 1 | 2.8% |
| Traumatic ulcer | 1 | 2.8% |
| Nicotine stomatitis | 3 | 8.3% |
| Geographic tongue | 4 | 11.2% |
| Candidiasis | 5 | 13.9% |
| Lichen planus | 7 | 19.4% |
| Actinic cheilitis | 8 | 22.2% |
| Frictional keratosis | 6 | 16.6% |
Relationship between cancerous lesions and age of patients.
| Decade of Life/Lesion | Lichen planus | Nicotine stomatitis | Actinic cheilitis | Frictional keratosis | Total | p-value (Chi-square test) |
|---|
| 3rd | 0 | 0 | 1 | 0 | 1 | 0.001 |
| 4th | 0 | 1 | 1 | 0 | 2 |
| 5th | 1 | 0 | 1 | 2 | 4 |
| 6th | 4 | 2 | 5 | 3 | 14 |
| 7th | 1 | 0 | 0 | 0 | 1 |
| 8th | 1 | 0 | 0 | 1 | 2 |
Relationship between lesion diagnosis and smoking.
| Smoking/Lesion | Nicotine stomatitis | Candidiasis | Actinic cheilitis | Total | p-value (Chi-square test) |
|---|
| Yes | 3 | 3 | 6 | 12 | 0.001 |
| No | 0 | 2 | 2 | 4 |
The most prevalent treatments included laser therapy, antifungal treatment, and the use of sunscreen and lip moisturiser [Table/Fig-7]. All treatments performed showed good results, without complications.
Absolute number and percentage of the therapeutic conducts adopted.
| Treatment | Frequency | Percentage |
|---|
| Oral hygiene instruction | 1 | 2.8% |
| Occlusal traumatic factor removal | 1 | 2.8% |
| Sunscreen/lip moisturiser | 1 | 2.8% |
| use of wide hat to protect against the sun | 1 | 2.8% |
| 50% glucose application Topical corticosteroid | 1 | 2.8% |
| No treatment required | 2 | 5.6% |
| Incisional biopsy and sunscreen/lip moisturiser | 2 | 5.6% |
| Excisional biopsy | 3 | 8.3% |
| Prosthetic adjustment | 3 | 8.3% |
| Stop smoking | 4 | 11.5% |
| Antifungal agents | 5 | 13.5% |
| Sunscreen/lip moisturiser | 5 | 13.5% |
| Laser therapy | 7 | 19.7% |
[Table/Fig-8]: It shows the most prevalent aetiologies for the lesions, with excessive sun exposure as the most common, followed by chronic trauma and stress.
Absolute number and percentage of cases regarding the aetiology of the lesion.
| Aetiology | Frequency | Percentage |
|---|
| Chronic trauma | 7 | 19.4% |
| Smoking | 4 | 11.1% |
| Fungal infection | 5 | 13.9% |
| Autoimmune | 5 | 13.9% |
| Stress | 6 | 16.7% |
| Excessive sun exposure | 8 | 22.2% |
| Idiopathic origin | 1 | 2.8% |
The surface of white lesions was non-scrapable in 24 patients (66.7%) and scrapable in 12 cases (33.3%).
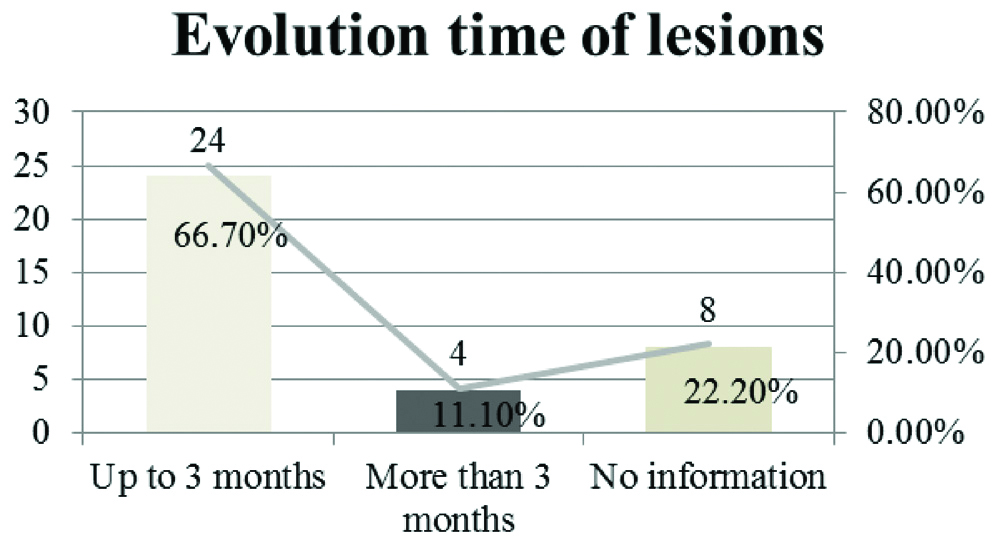
Regarding the evolution time of white lesions cataloged, the results listed in [Table/Fig-9] were identified.
Distribution of patients analysed regarding the evolution time of white lesions.
Discussion
In the present study, 36 patients with white lesions of the oral mucosa were cataloged within two years of assistance in a school service for stomatological care, and most patients were men. When investigating 52 patients with oral white lesions, Freitas MD et al., found 65% of men in a Spanish population [10]. However, Baingridge KE et al., studying US adults have found that 74.5% of patients with white lesions were women [3].
As for the age group of patients with oral white lesions; Shet R et al., indicates that Indian people older than 50 years are more affected [11]. This agrees with the findings of the present study, which showed a prevalence of patients in the sixth decade of life (17 cases-47.2%). This result, however, disagrees with a prospective clinicohistological study of premalignant and malignant lesions of the oral cavity conducted by Misra V et al., in India, in which the fourth decade of life showed a higher number of white lesions [12].
Regarding the ethnicity of patients analysed in the present study, most of the lesions were observed in white individuals. This data disagrees with those found in the literature. When analysing 1,052 individuals under dental treatment, Al-Mawer AA et al., found 25.2% of patients with oral white lesions in a population of Saudi Arabia, from which only 5.1% were white patients [13]. Though, it should be noted that the factor of ethnicity is closely related to the geographic location of the study. The region of interest of the present study (Rio Grande do Sul, Brazil) is predominantly of European colonisation, which may explain the expressive number of white patients affected by white lesions.
However, Kansky AA et al., performed a survey of oral lesions in 2,395 patients in Slovenia and found lichen planus, hairy tongue, frictional keratosis, and linea alba as the most common white lesions [14]. This corroborates the present study, in which according to the authors, lichen planus was one of the most common white lesions. Similarly, an epidemiological survey of oral lesions conducted by Hoff K et al., at the School of Dentistry of the University of Passo Fundo, RS, Brazil, between 2000 and 2013, examining 940 lesions, indicated that lichen planus was the most common non scrapable white lesion (52 cases-5.5%), the result which corroborates the findings of the present study [15]. It should be noted that such results depend on several factors such as habits, epidemiological characteristics, and geographic region of origin of the population studied.
Among the treatments most indicated for white lesions observed in the present study, laser therapy, antifungal treatment, and the use of sunscreen and lip moisturiser, were considered successful when aplicated in the correct lesion. Martins RB et al., studying a Brazilian population also claims that the treatment is strictly dependent on the nature of the white lesion to be treated [9].
Regarding the aetiologies of the lesions studied, the most frequent were excessive sun exposure, chronic trauma, and stress. These results are an addition to the systematic literature review of El-Zaemey S et al., which states that most non-scrapable white lesions occur due to a chronic cause-effect traumatic relationship, such as the use of poorly adapted prostheses, parafunctional habits, and excessive exposure to ultraviolet sunlight [16].
An expressive number of patients presented sun exposure as the aetiological factor for white lesions. This result may relate to the fact that the economy of the geographic region in which the School of Dentistry of the study is located in area largely based on agricultural activities, which corroborates the fact that patients were often exposed to ultraviolet light, as related by Moreira VS and Medeiros RMV [17]. Regarding the potential aetiological factors of the lesions, our result differs from the study performed in Morocco, by Haitami S et al., [18]. In such study, the authors found that the most significant risk factors for 306 potentially malignant or malignant white oral lesions were alcoholism and smoking. Another study performed by Henrique PR et al., in a population of the city of Uberaba, MG, Brazil, found that 320 lesion carriers (32%) were frequently exposed to the sun, 254 (25%) were smokers, and 153 (15%) were alcoholics [19]. Thus, Henrique PR et al., noted that, probably due to the regional/cultural differences of the samples studied, the aetiological factors for the lesions analysed may be different [19].
Regarding deleterious habits (smoking and alcoholism), from the 36 patients included in this study, 17 (47.2%) were smokers and only nine (25%) were alcoholics. Contrary to what was observed in the present study, almost invariably the literature states that in series of white oral lesions, smoking and alcoholism are among the main aetiological factors. A classic example is a study of Morger R et al., conducted in Switzerland with young people aged 18 to 24 years, in which alcohol consumption and smoking were related to the appearance of white patches in the oral mucosa [20]. The epidemiological study of Liu G et al., performed in the USA emphasizes that alcohol consumption, age, sex, ethnicity, level of education, and family income are related directly to the presence of oral lesions [21].
It was also considered that, because the present study did not show an expressive number of smokers and alcoholics, leukoplakia (the main white lesion caused by smoking and alcoholism) did not appear on the list of white lesions studied. Different from our results, Laskaris G found leukoplakia as the second most frequent lesion in their results of five cases, from which three were smokers [22].
Though, Neumann A et al., studying American dental institutions, indicate that dentists should implement strategies aiming to control and reduce smoking in individuals with such habit, as this is a strong risk factor for pathological oral changes [23]. These strategies, according to Gambin DJ et al., may be exercised with the motivation of individuals exposed to cigarette or alcohol, explanatory conversations, individualised personal orientation, and the development of guidelines in the form of booklets, folders, or self-explanatory figures [24].
A significant number of medical records without information were observed in the present study. Studying a Brazilian population, Benedicto EN et al., affirm that currently, dental documentation has been playing an important role in the defense of dentists against the increasing administrative, civil, and criminal proceedings, considering such documentation may be used as pre-constituted evidence, that is, evidence elaborated over time, when the patient was being subjected to several dental treatments [25].
Limitation
The sample size of the study population was relatively small. Another limitation of the present study is the lack of prospective follow-up of analysed cases.
Conclusion
The sample of oral white lesions studied represents substantial importance for epidemiological planning for the geographic region studied. Special attention should be given to actinic cheilitis, as it is the most prevalent lesion and is considered a cancerous lip injury. It was also noted that the cancerous lesions included in the samples revealed a significant presence in the sixth decade of life and men had more deleterious habits in comparison to women in the studied region.