Introduction
Adhesive Capsulitis (AC) causes musculoskeletal disorder of shoulder which is a common reason for loss of function and disability in patients. Several interventions have been used for treatment of AC but very few of them have taken into consideration “Myofascial Origin” as a probable cause of pain.
Aim
To review the current literature related to prevalence, diagnosis, and treatment of “Myofascial Trigger Points (MTrPs) in AC”. To compare the prevalence of MTrPs in Diabetic and Non-Diabetic patients.
Materials and Methods
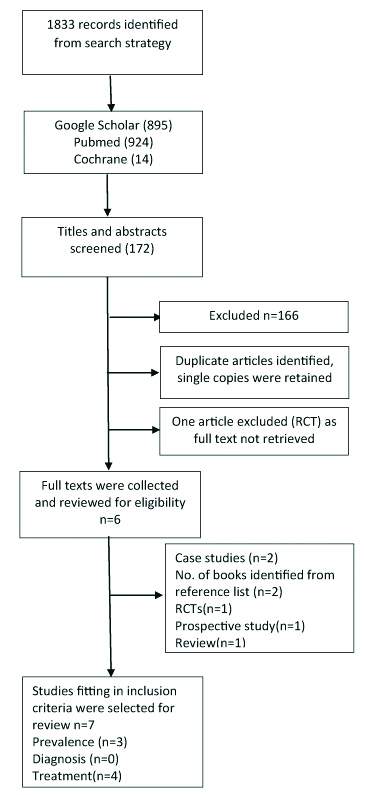
Google Scholar, Pubmed, Cochrane library, Central register for clinical trial were searched for published randomised controlled trials, systematic or literature reviews, case study, pilot study and book references in English language from inception till December 2018. Out of total 1833 results identified, 7 relevant studies with a total of 190 patients were finally selected for the review. Four studies were analysed for methodological quality using Pedro tool for randomised controlled trial and National Institutes of Health tool for observational study and case reports. The study was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses statement (PRISMA).
Results
Among all the articles, three of them discussed about the prevalence of MTrPs in AC. These studies showed the greater prevalence of MTrPs in subscapularis muscle which may be the cause for pain and restricted shoulder movements. There was no study on diagnosis of MTrPs in AC. The studies (four in number) which showed the efficacy of treatment of MTrPs included techniques like Myofascial release technique+deep stroking (Niel Asher Technique), Ischaemic Compression of MTrPs, Dry Needling, Infiltration of Subscapularis TrPs with Subscapularis nerve block.
Conclusion
MTrPs acts as an important contributing factor for causing pain, movement restriction and disability in the patients. Interventional studies have found significant improvement in shoulder pain and function but the exact method and the muscles which received the treatment were not mentioned. This review suggests that, there is need for good quality studies related to the prevalence, diagnosis and treatment of MTrPs in AC subjects with Diabetes Mellitus as well as without Diabetes Mellitus.
Introduction
AC is a condition which can occur either in isolation or simultaneously with other shoulder pathologies (eg., rotator cuff tendinopathy, bursitis, etc.,). It results from contraction of the glenohumeral capsule which adheres to the head of humerus [1]. Patients usually have a history of debilitating pain and progressive limitation of glenohumeral movements. External rotation of shoulder is the most restricted movement followed by abduction and internal rotation [2,3].
Though the exact cause remains unknown, AC is associated with various precipitating factors. Studies have shown that people who are elderly, females, with diabetes mellitus and abnormal lipid profiles have increased risk of developing AC [4,5]. In addition, thyroid dysfunction is also found to be a risk factor for AC [6,7]. Furthermore, frozen shoulder is also found to be associated with upper limb injury and cardiac or neuro surgery [8]. The prevalence of AC is approximately 2% in the general population, but the actual figure is very close to 0.75% [9]. However, a meta-analysis of prevalence of AC, reported that subjects with Diabetes Mellitus (DM) have 5 times greater probability to develop AC with a prevalence of 13.4% [10].
DM is a metabolic disease characterised by elevated blood sugar levels either due to inadequate secretion of insulin or its action or both. It is associated with various complications which disrupt the function of various organs like eyes, kidneys, nerves, heart, and blood vessels and damage them [11]. The prevalence of AC in DM and vice-versa is found to be high (13.4% and 30% respectively) [10].
MTrPs are one of the common causes of pain in various musculoskeletal disorders [12]. It is found that these might be present in the muscles around the shoulder in subjects with AC. These muscles may include subscapularis and latissimus dorsi which in turn may restrict overhead elevation, abduction and external rotation of the shoulder [13].
A MTrP is a highly sensitive spot within a taut band of skeletal muscle, which produces pain on compression and can result in referred pain, motor dysfunction and autonomic response [14,15]. It may be an active or latent TrP. An active MTrP causes spontaneous clinical pain and constant tenderness which may be localised to the tissue and or referred to specific areas. Latent MTrP produce pain only when it is palpated [14].
A study on subjects with chronic non traumatic shoulder pain (n=72) showed high prevalence of MTrPs in all subjects; highest prevalence being in infraspinatus (78%) followed by upper trapezius (58%), middle trapezius (43%), deltoid and teres minor [16]. A literature review showed greater number of active TrPs in shoulder pain [17].
Clinically, TrPs are usually identified by palpation at the site of pain and taut band. Various studies have concluded that palpation was a reliable technique for identifying MTrPs in shoulder muscles [17], [18]. Some studies have also evaluated the use of ultrasonography, electromyography, magnetic resonance imaging, spontaneous electrical activity, biopsies in understanding the characteristics of MTrPs [19-22]. In a literature review on assessment of MTrPs using Ultrasound, three techniques of ultrasound were found useful in localising MTrPs: conventional grey scale imaging, doppler and elastographic techniques [22]. In another study grey scale images were initially not useful (showed hyperechoic regions) in identifying MTrPs [23], but later on further investigation proved fruitful [21-26] (most showed hypoechoic regions). Still adequate sensitivity has not been achieved [26]. The applicability and reliability of doppler technique to diagnose TrP needs further investigation. One of the useful objective measures in identifying MTrP were findings of electromyography and ultrasound imaging, the spontaneous activity in MTrP, and biopsies of MTrPs [20]. Both the nerve terminal and the muscle fiber after the neuromuscular junction were involved in the endplate dysfunction characteristic of MTrPs and so, the criteria should be taken into consideration while diagnosing MTrPs.
Various treatment techniques have been used to treat these TrPs in shoulder pain eg. Dry needling, manual pressure, ischaemic compression, ultrasonography, stretching and application of ice, laser therapy, soft tissue mobilisation, joint mobilisation etc., [27-39]. A study found that dry needling and manual pressure both showed significant improvements in Neck Disability Index (NDI), Pressure Pain Threshold (PPT), muscle elasticity and stiffness [27]. Other studies also showed significant improvements in VAS (Visual Analogue Scale) scores, PPT, range of motion, and muscle function [28-35].
As discussed earlier, there are enough studies about the prevalence, diagnosis and treatment of MTrPs in shoulder pain. However, there are very few studies which discuss about the prevalence and treatment of MTrPs in AC. Moreover, no study as per our knowledge, has commented about any difference in the prevalence rate of MTrPs in AC including those having diabetes mellitus and in those without diabetes mellitus.
Furthermore, there are many reviews on the diagnosis and management of AC [36-42]. However, none of those discuss about the diagnosis, prevalence and effective management of MTrPs to reduce pain and improve functional ability in these patients.
So, aim of the review article is to review the current literature about the prevalence, diagnosis, and management of MTrPs in AC patients with or without diabetes mellitus.
Materials and Methods
Search strategy and information sources: Google Scholar, Pubmed, Cochrane library, Central register for clinical trial were searched for the relevant articles from inception till December 2018. Books were also used as a source of reference. The keywords used for the search were: myofascial trigger points, Adhesive Capsulitis, frozen shoulder, periarthritis shoulder. The reference list of relevant publications was also reviewed to identify any related trials.
Study selection criteria: All types of published studies were included for the review; Randomised Controlled Trials (RCT), systematic or literature reviews, case study, pilot study and books were also included. All articles which discussed about the prevalence, diagnosis or/and management of MTrPs in AC patients were included for the review. The studies in which shoulder pain was due to AC alone were included.
Exclusion criteria: Studies on shoulder pain which did not specify AC in their inclusion criteria or in their discussion or conclusion were excluded. Studies in languages apart from English were also excluded. Interventional articles for AC excluding the treatment of MTrPs were eliminated.
Data items: All the reviewers independently collected the data. The data items included population baseline characteristics, intervention given to both the treatment and control groups, outcomes and study design.
Risk of bias in individual studies: The risk of bias for randomised controlled trials was assessed using PEDro (Physiotherapy Evidence Database) quality scale [43]. The study quality assessment tools of the National Heart, Lung, and Blood Institute of the National Institutes of Health (NIH) was used to assess the quality of case reports, case series and observational study [44].
Study selection: A total of 1833 results were found from databases (14 from cochrane library and 924 from pubmed and 895 from google scholar). After reading the abstract and title, 172 studies were identified for screening. On reading the full text, 166 studies were excluded due to inappropriate intervention and inappropriate population. If there were duplicate articles identified, only single copies were considered. The full texts of selected articles were thoroughly studied again for the eligibility. One study (RCT) was again excluded as the full text of the article could not be retrieved. The references from the selected articles was also searched. Finally, 7 studies were selected for the review. The flow chart illustrates the results of the search [Table/Fig-1].
Overview of the review procedure.
Results
Study characteristics and risk of bias of included studies: [Table/Fig-2,3] shows the summary of the studies included for the review. The risk of bias assessment demonstrated moderate quality of the included studies (n=4) due to lack of patient, therapist and assessor blinding [13,14,45].
Summary of relevant prevalence studies in AC [13,14,45].
| Author’s name | Year | Outcome |
|---|
| Travell JG et al., [14] | 1999 | MTrPs in subscapularis muscle are an important factor for symptoms |
| Lewit K [45] | 1991 | Spasm of subscapularis with TrPs accompanies AC |
| Gerwin RD [13] | 1997 | Limitation of abduction and external rotation in AC due to MTrPs in shoulder muscles |
Summary of relevant interventional studies in AC [47,49-51].
| Sl. No | Author/Year | Study design | Randomisation | Mean age (years) | Gender | Treatment technique | Outcome measures | Results |
|---|
| 1. | Jeyakumar S et al, 2016 [47] | Randomised Controlled Trial | Yes | 30 subjects with mean age of 40-60 | Male and Female | MTrP release technique to one group and Maitland mobilisation to other group for 4 weeks | VAS, SPADI | Both the groups showed significant improvement in SPADI scores and ROM values but more improvement (p<0.01) in Maitland mobilisation group than in TrP release group |
| 2. | Niel-Asher S et al, 2014 [49] | Prospective observational multi-centre study | No | 54.2 (22-77) | 67 Male, 87 Female n=154 | Niel-Asher technique (NAT) which consisted of compression of trigger points and deep stroking massage performed in 5 steps. Treatment given for a mean period of 11 weeks | AROM (flexion and abduction), VAS for pain | Significant improvement in AROM in all centres with greatest in Israel where reduction of pain was also significant |
| 3. | Clewley D et al., 2014 [50] | Case report | No | 54 | Female n=1 | 2 sessions of mobilisation and manipulation of cervical and thoracic joints and 1 session of Dry needling on identified TrPs in the upper trapezius, levator scapulae, deltoid and infraspinatus | SPADI (Disabilities of the Arm, Shoulder and Hand questionnaire) | Significant improvement in Shoulder ROM and functions |
| 4. | Jancovic D et al., 2006 [51] | Case report | No | 57.6 | 2 Male, 3 Female, n=5 | Subscapularis nerve block and infiltration of subscapular trigger point with triamcinolone and ropivacaine | VAS | Significant improvement in the VAS score suggesting contribution of subscapularis muscle in the etiology of AC. |
Prevalence of MTrPs in patients with AC: In patients with frozen shoulder, active TrPs in subscapularis muscle are identified to be a major factor in producing symptoms of AC such as pain and restriction in range of motion of shoulder [14]. Painful spasm of subscapularis muscle with TrPs accompanies frozen shoulder. The reason is that other muscles of shoulder also become involved which add to pain pattern (reference of pain in arm) and restrict movement. Until and unless subscapularis TrPs are identified and corrected, symptoms will persist [45].
Another study explained that limitation of movements in frozen shoulder can be due to TrPs in muscles (supraspinatus, infraspinatus, teres major and minor, deltoid, pectorals, subscapularis and latissimus dorsi) around shoulder which restrict the movements. Trigger points in these muscles may lead to referred pain that may be local (eg., In teres major and minor) or distant (eg., In infraspinatus). In anterior shoulder pain, TrPs are seen in pectoral muscle, deltoid and infraspinatus. In posterior shoulder pain, subscapularis, deltoid and teres major muscle have TrPs. In lateral shoulder pain, supraspinatus muscle has TrPs. Pain inferomedial to the scapula usually is seen with TrPs in latissimus dorsi. In frozen shoulder, the TrPs in subscapularis and in latissimus dorsi are responsible for restriction of abduction and external rotation of shoulder and inhibit overhead elevation [13].
Treatment of MTrPs in AC: One study found that TrPs may be existent around the shoulder muscles of patients with AC especially subscapularis which causes restriction of shoulder elevation and external rotation [36]. They found that TrP (esp. In subscapularis and latissimus dorsi) irritation and pain might be reduced by the Spray and Stretch® technique which gradually help lengthen the tight muscles [46].
In another article the effect of Maitland mobilisation and MTrP release in patients with AC of shoulder were compared [47]. Total of 30 subjects (both male and female between 40 -60 years of age) who took part in the study were allotted into two groups (15 patients in each group). One group was given MTrP release technique and the other received Maitland mobilisation for a duration of four weeks. The outcome measures used were VAS, range of motion of shoulder and SPADI (Shoulder Pain and Disability Index). Both the groups demonstrated statistically significant difference (p<0.01) in decreasing pain, improving range (abduction and external rotation) and improving functional activity. The reduction of pain was almost same in both the groups. However, the improvement in goniometric values and SPADI scores was better in the maitland group rather than the TrP release group.
Another study was a randomised trial on 90 type 2 diabetes mellitus subjects with AC [48]. The subjects of both gender (41 male, 49 female) participated and having an average age of 54.14±12.85 years. One group received anti diabetic drugs, pain killers, active exercises of shoulder joint. The experimental group was given mobilisation of shoulder joint, neurodynamic mobilisation, myofascial release and TrPs therapy in addition to that received by the control group. The treatment was given for 45 minute for five (one session/week) weeks. The experimental group indicated statistically significant improvements (p<0.05) in pain, abduction and external rotation range, SPADI scores and Shoulder Functional Tests Battery (SFTB) scores. This study was not included in the systematic review as full text was not retrieved despite various attempts.
A multicentre study was performed in three centres (Israel, UK and US) to assess the effectiveness of Niel Asher Technique (NAT) [49]. Total of 154 subjects (113 from Israel, 25 from and 16 from US) diagnosed with AC participated. There were 67 males and 87 females who were 54.2-year-old on an average. The technique consisted of compression of TrPs and deep stroking massage performed in 5 steps. The session lasted for an average of 30 minutes. Treatment sessions were given for a mean period of 11 weeks. The number of sessions and gaps between sessions were decided based on the acuteness of the condition (mean number of sessions being 7). The active range of abduction and flexion and VAS were measured pre and post treatment. Results showed that there was significant improvement in shoulder range in all the centres, greatest being in Israel. The subjects from Israel also showed significant decrease in pain (VAS in UK and US patients was not recorded).
Another study was a case study on a 54-year-old woman established with AC [50]. Treatment initially consisted of two sessions of shoulder mobilisation and manipulation of cervical and thoracic joints. Though these sessions improved the functions of shoulder to a little extent, there was a lot of pain which was preventing further improvement. On examination, TrPs were identified in the upper trapezius, levator scapula, deltoid, and infraspinatus muscles. Dry needling of these points was performed in the third session which resulted in significant reduction in pain (greater than that in the first two sessions). This helped the patient to better tolerate the manual therapy. The subjects received 13 treatment sessions for 6 weeks. The patient showed significant progress in shoulder range and functions at the completion of the treatment.
In a study on five subjects diagnosed with frozen shoulder, TrPs in subscapularis were infiltrated and nerve block was given to the subscapular nerve in those patients who had no or minimal improvement through conventional therapy. The subscapular nerve block was given by inserting the needle into the midpoint of the medial margin of the scapula pointing towards acromion and injecting 10-15 mL of ropivacaine (0.375-0.75%) [51]. Results showed that both these treatments were useful for diagnosis as well as treatment of the frozen shoulder thus suggesting the contribution of subscapularis muscle in the aetiology of AC.
Discussion
MTrPs are found to be present in the muscles around the shoulder in AC patients [13]. The objective of the review was to find the prevalence, diagnosis and treatment of the MTrPs in AC patients and to ascertain whether there was any difference between diabetic and non-diabetic subjects with AC.
Two studies discussed about the prevalence of MTrPs in AC [13,14]. These studies showed that greater restriction of abduction and external rotation of the shoulder is due to prevalence of MTrPs in subscapularis and latissimus dorsi muscle in patients with frozen shoulder [Table/Fig-2]. However, these are not randomised controlled studies and the prevalence rates are not specified. Hence, prevalence studies should be conducted and investigated in future. In general shoulder pain, there is higher prevalence of MTrPs in infraspinatus (78%) followed by that in upper trapezius (58%) and other muscles [16]. But in one study, it was found that the prevalence of TrPs varies according to the type of shoulder pain. For example, in anterior shoulder pain, TrPs are seen in pectoral muscle, deltoid and infraspinatus. In posterior shoulder pain, subscapularis, deltoid and teres major muscle have MTrPs. In lateral shoulder pain, supraspinatus muscle has MTrPs. Pain inferomedial to the scapula usually is seen with TrPs in latissimus dorsi. In frozen shoulder, the TrPs in subscapularis and in latissimus dorsi are responsible for restriction of abduction and external rotation of shoulder and inhibit overhead elevation [13]. So, there is a need to study the prevalence of MTrPs in the specific shoulder pain such as frozen shoulder.
On reviewing the studies which focused on diagnosis of MTrPs in AC patients, it was found that there were no studies as per the author’s knowledge which investigated the same. But, there were many studies which discussed about the reliability of manual palpation of MTrPs [18] and diagnostic ultrasound [21,22] techniques to diagnose the MTrPs in general pain. There is a dearth of studies on diagnostic criteria of MTrPs in specific conditions like AC. Henceforth, future studies need to concentrate on diagnosis of MTrPs in AC patients.
The studies reviewed on treatment of MTrPs in AC exhibited significant reduction in shoulder pain and improvement in function through different interventions like Maitland mobilisation, TrPs compression and deep stroking massage (Niel Asher technique), dry needling, trigger point release and subscapularis infiltration and nerve block [Table/Fig-3]. The maitland mobilisation technique in the study by Jeyakumar S et al., made use of grade I and II small amplitude and large amplitude rhythmic oscillations at the beginning of available range of movement. These grades help in relieving pain by stimulating mechanoreceptors and inhibiting pain at spinal cord or brainstem levels [47]. The study also made use of TrP release technique which involved releasing the TrPs in the taut bands of the muscles by compressing it and holding it for 15 seconds. This technique also helps in relieving pain by washing out noxious substances due to improved blood flow [47]. The Niel Asher technique consisted of five step protocol made up of deep stroking massage, passive movement and TrP compression which improved the active range of shoulder abduction and flexion [49]. Dry needling technique made use of filiform needles inserted into the TrPs to upper trapezius, levator scapula, deltoid, and infraspinatus muscles which resulted in pain free range of motion and improvement of shoulder function [50]. Gerwin RD in his review found that spray and stretch technique (stretching the muscle followed by spraying of a vapo-coolant spray) can also help to treat the TrPs present in subscapularis or latissimus dorsi responsible for restriction of shoulder abduction and external rotation [13].
However, very few among these studies specified the muscles which received the treatment. In those studies which had specified the muscles to be treated, the diagnostic criteria of evaluating MTrPs were not mentioned. In few studies, the exact methods were not mentioned. Moreover, the individual effects of treatment of MTrPs were not evaluated as most of the studies used a combination of various treatment techniques. One study found the significant contribution of subscapularis muscle in the etiology of AC [51]. Moreover, Travel JG and Simons DG, and Lewit K have also stressed the key role of subscapularis MTrPs in AC [14,45]. Since there is a dearth of these types of studies, they are not enough to evaluate the importance of the myofascial origin of pain due to specific muscles in AC.
Limitation
There were certain limitations in the study. The studies included in the review were of different designs as one of them was randomised controlled trial, two were case reports, one was review and two were articles from book. The studies were of moderate quality. Book sources could not be analysed for methodological quality. Decent randomised controlled trials on the diagnosis, prevalence and treatment of MTrPs in AC are lacking. Henceforth, further studies are needed to assess the role of specific MTrPs in causing aches and disability in patients with AC.
Conclusion
Higher prevalence of MTrPs in shoulder pain explains the critical contribution of MTrPs in causing shoulder disability. However, different disorders of shoulder joint have different prevalence rates of muscular TrPs in the shoulder. In subjects with AC, there seems to be higher prevalence of subscapularis MTrPs. Thus, meticulous diagnosis and treatment of these TrPs can contribute to a significant extent in relieving shoulder aches and disability in AC. However, there are lack of studies on prevalence and diagnosis of TrPs in AC subjects. Hence, there is a need for future studies focusing on the same. Also, the prevalence of DM in AC and vice versa is significant. But as per the knowledge of the authors, no study has compared the prevalence of MTrPs in diabetic versus non- diabetic AC patients. This can be an important factor in understanding the differences with respect to disability and hence the treatment of diabetic and non-diabetic subjects.
[1]. Ewald A, Adhesive capsulitis: A reviewAm Fam Physician 2011 83(4):417-22.Available from: http://www.ncbi.nlm.nih.gov/pubmed/21322517 [Google Scholar]
[2]. Calis M, Demir H, Ulker S, Kirnap M, Duygulu F, Calis HT, Is intraarticular sodium hyaluronate injection an alternative treatment in patients with adhesive capsulitis?Rheumatol Int 2006 26(6):536-40.Available from: http://www.ncbi.nlm.nih.gov/pubmed/1609192010.1007/s00296-005-0022-216091920 [Google Scholar] [CrossRef] [PubMed]
[3]. Reeves B, The natural history of the frozen shoulder syndromeScand J Rheumatol 1975 4(4):193-96.Available from: http://www.tandfonline.com.ezproxy.med.nyu.edu/doi/pdf/10.3109/0300974750916525510.3109/030097475091652551198072 [Google Scholar] [CrossRef] [PubMed]
[4]. Huang Y-P, Fann C-Y, Chiu Y-H, Yen M-F, Chen L-S, Chen H-H, Association of diabetes mellitus with the risk of developing adhesive capsulitis of the shoulder: A longitudinal population-based follow-up studyArthritis Care Res (Hoboken) 2013 65(7)):1197-202.Available from: http://doi.wiley.com/10.1002/acr.2193810.1002/acr.2193823281342 [Google Scholar] [CrossRef] [PubMed]
[5]. Salek A, Mamun M, Haque M, Mannan M, Ali E, Islam S, Serum triglyceride level in type 2 diabetes mellitus patients with or without Frozen shoulderBangladesh Med Res Counc Bull 2011 36(2)Available from: http://www.banglajol.info/index.php/BMRCB/article/view/699010.3329/bmrcb.v36i2.699021473204 [Google Scholar] [CrossRef] [PubMed]
[6]. Li W, Lu N, Xu H, Wang H, Huang J, Case control study of risk factors for frozen shoulder in ChinaInt J Rheum Dis 2015 18(5):508-13.Available from: http://doi.wiley.com/10.1111/1756-185X.1224610.1111/1756-185X.1224624438046 [Google Scholar] [CrossRef] [PubMed]
[7]. Cakir M, Samanci N, Balci N, Balci MK, Musculoskeletal manifestations in patients with thyroid diseaseClin Endocrinol (Oxf) 2003 59(2)):162-67.Available from: http://www.ncbi.nlm.nih.gov/pubmed/1286479210.1046/j.1365-2265.2003.01786.x12864792 [Google Scholar] [CrossRef] [PubMed]
[8]. Hand C, Clipsham K, Rees JL, Carr AJ, Long-term outcome of frozen shoulderJ Shoulder Elb Surg 2008 17(2):231-36.Available from: http://linkinghub.elsevier.com/retrieve/pii/S105827460700486710.1016/j.jse.2007.05.00917993282 [Google Scholar] [CrossRef] [PubMed]
[9]. Bunker T, Time for a new name for frozen shoulder—contracture of the shoulderShoulder Elb 2009 1(1):4-9.Available from: http://sel.sagepub.com/lookup/doi/10.1111/j.1758-5740.2009.00007.x10.1111/j.1758-5740.2009.00007.x [Google Scholar] [CrossRef]
[10]. Zreik Nasri H, Adhesive capsulitis of the shoulder and diabetes: A meta-analysis of prevalenceMuscles Ligaments Tendons J 2016 Available from: http://www.mltj.org/index.php?PAGE=articolo_dett&ID_ISSUE=884&id_article=753210.11138/mltj/2016.6.1.02627331029 [Google Scholar] [CrossRef] [PubMed]
[11]. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 200;27 Suppl 1:S5-10. Available from: http://www.ncbi.nlm.nih.gov/pubmed/1469392110.2337/diacare.27.2007.S514693921 [Google Scholar] [CrossRef] [PubMed]
[12]. Simons DG, Review of enigmatic MTrPs as a common cause of enigmatic musculoskeletal pain and dysfunctionJ Electromyogr Kinesio 2004 14(1):95-107.Available from: http://www.ncbi.nlm.nih.gov/pubmed/1475975510.1016/j.jelekin.2003.09.01814759755 [Google Scholar] [CrossRef] [PubMed]
[13]. Gerwin RD, Myofascial pain syndromes in the upper extremityJ Hand Ther 1997 10(2):130-36.Available from: http://dx.doi.org/10.1016/S0894-1130(97)80067-110.1016/S0894-1130(97)80067-1 [Google Scholar] [CrossRef]
[14]. Travell JG, Simons DG, Myofascial Pain and Dysfunction: The Trigger Point Manual. Volume 1Upper Half of Body 1999 Volume 12nd editio:596-612. [Google Scholar]
[15]. Ge HY, Fernández-de-las-Peñas C, Arendt-Nielsen L, Sympathetic facilitation of hyperalgesia evoked from myofascial tender and trigger points in patients with unilateral shoulder painClin Neurophysiol 2006 117(7):1545-50.10.1016/j.clinph.2006.03.02616737848 [Google Scholar] [CrossRef] [PubMed]
[16]. Bron C, High prevalence of shoulder girdle muscles with myofascial trigger points in patients with shoulder painBMC Musculoskelet Disord 2011 12:13910.1186/1471-2474-12-13921711512 [Google Scholar] [CrossRef] [PubMed]
[17]. Sergienko S, Kalichman L, Myofascial origin of shoulder pain: A literature reviewJ Bodyw Mov Ther 2015 19(1):91-101.Available from: http://linkinghub.elsevier.com/retrieve/pii/S136085921400076X10.1016/j.jbmt.2014.05.00425603748 [Google Scholar] [CrossRef] [PubMed]
[18]. Bron C, Franssen J, Wensing M, Oostendorp RAB, Interrater reliability of palpation of myofascial trigger points in three shoulder musclesJ Man Manip Ther 2007 15(4):203-15.Available from: http://www.tandfonline.com/doi/full/10.1179/10669810779081947710.1179/10669810779081947719066669 [Google Scholar] [CrossRef] [PubMed]
[19]. Zhuang XQ, Tan SS, Huang QM, Understanding of myofascial trigger pointsChin Med J (Engl) 2014 127(24):4271-77. [Google Scholar]
[20]. Simons DG, Diagnostic criteria of myofascial pain caused by trigger pointsJ Musculoskelet Pain 1999 7(1/2):111-20.10.1300/J094v07n01_11 [Google Scholar] [CrossRef]
[21]. Sikdar S, Shah JP, Gebreab T, Yen RH, Gilliams E, Danoff J, Novel applications of ultrasound technology to visualize and characterize myofascial trigger points and surrounding soft tissueArch Phys Med Rehabi 2009 90(11):1829-38.Available from: http://dx.doi.org/10.1016/j.apmr.2009.04.01510.1016/j.apmr.2009.04.01519887205 [Google Scholar] [CrossRef] [PubMed]
[22]. Kumbhare DA, Elzibak AH, Noseworthy MD, Assessment of myofascial trigger points using ultrasoundAm J Phys Med Rehabil 2016 95(1):72-80.Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00002060-201601000-0000910.1097/PHM.000000000000037626334421 [Google Scholar] [CrossRef] [PubMed]
[23]. Lewis J, Tehan P, A blinded pilot study investigating the use of diagnostic ultrasound for detecting active myofascial trigger pointsPain 1999 79(1):39-44.Available from: http://www.ncbi.nlm.nih.gov/pubmed/992877410.1016/S0304-3959(98)00155-9 [Google Scholar] [CrossRef]
[24]. Shankar H, Reddy S, Two- and three-dimensional ultrasound imaging to facilitate detection and targeting of taut bands in myofascial pain syndromePain Med 2012 13(7):971-75.Available from: http://www.ncbi.nlm.nih.gov/pubmed/2268118510.1111/j.1526-4637.2012.01411.x22681185 [Google Scholar] [CrossRef] [PubMed]
[25]. Sikdar S, Shah JP, Gilliams E, Gebreab T, Gerber LH, Assessment of myofascial trigger points (MTrPs): A new application of ultrasound imaging and vibration sonoelastographyConf Proc. Annu Int Conf IEEE Eng Med Biol Soc IEEE Eng Med Biol Soc Annu Conf 2008 2008:5585-88.Available from: http://www.ncbi.nlm.nih.gov/pubmed/1916398310.1109/IEMBS.2008.465048019163983 [Google Scholar] [CrossRef] [PubMed]
[26]. Turo D, Otto P, Shah JP, Heimur J, Gebreab T, Zaazhoa M, Ultrasonic characterization of the upper trapezius muscle in patients with chronic neck painUltrason Imaging 2013 35(2):173-87.Available from: http://www.ncbi.nlm.nih.gov/pubmed/2349361510.1177/016173461247240823493615 [Google Scholar] [CrossRef] [PubMed]
[27]. De Meulemeester KE, Castelein B, Coppieters I, Barbe T, Cools A, Cagnie B, Comparing trigger point dry needling and manual pressure technique for the management of myofascial neck/shoulder pain: A randomized clinical trialJ Manipulative Physiol Ther 2017 40(1)):11-20.Available from: http://www.ncbi.nlm.nih.gov/pubmed/2801718810.1016/j.jmpt.2016.10.00828017188 [Google Scholar] [CrossRef] [PubMed]
[28]. Hsieh YL, Kao MJ, Kuan TS, Chen SM, Chen JT, Hong CZ, Dry needling to a key myofascial trigger point may reduce the irritability of satellite MTrPsAm J Phys Med Rehabil 2007 86(5):397-403.10.1097/PHM.0b013e31804a554d17449984 [Google Scholar] [CrossRef] [PubMed]
[29]. Hains G, Descarreaux M, Hains F, Chronic shoulder pain of myofascial origin: A randomized clinical trial using ischemic compression therapyJ Manipulative Physiol Ther 2010 33(5):362-69.Available from: http://dx.doi.org/10.1016/j.jmpt.2010.05.00310.1016/j.jmpt.2010.05.00320605555 [Google Scholar] [CrossRef] [PubMed]
[30]. Bron C, de Gast A, Dommerholt J, Stegenga B, Wensing M, Oostendorp RAB, Treatment of myofascial trigger points in patients with chronic shoulder pain: a randomized, controlled trialBMC Med 2011 9:8Available from: http://www.ncbi.nlm.nih.gov/pubmed/2126197110.1186/1741-7015-9-821261971 [Google Scholar] [CrossRef] [PubMed]
[31]. Yamany AA, Salim SE, Efficacy of low level laser therapy for treatment myofascial trigger points of shoulder painWorld Applied Sciences Journal 2011 12(6):758-64. [Google Scholar]
[32]. Cagnie B, Dewitte V, Coppieters I, Van Oosterwijck J, Cools A, Danneels L, Effect of ischemic compression on trigger points in the neck and shoulder muscles in office workers: a cohort studyJ Manipulative Physiol Ther 2013 36(8):482-89.Available from: http://www.ncbi.nlm.nih.gov/pubmed/2399375610.1016/j.jmpt.2013.07.00123993756 [Google Scholar] [CrossRef] [PubMed]
[33]. Penas C, Campo MS, Carnero JF, Page JCM, Manual therapies in myofascial trigger point treatment: A systematic reviewJ Bodyw Mov Ther 2005 9(1):27-34.Available from: www.intl.elsevierhealth.com/journals/jbmt10.1016/j.jbmt.2003.11.001 [Google Scholar] [CrossRef]
[34]. Gam AN, Warming S, Larsen LH, Jensen B, Høydalsmo O, Allon I, Treatment of myofascial trigger-points with ultrasound combined with massage and exercise--A randomised controlled trialPain 1998 77(1):73-79.Available from: http://www.ncbi.nlm.nih.gov/pubmed/975502110.1016/S0304-3959(98)00084-0 [Google Scholar] [CrossRef]
[35]. Hong C-Z, Chen Y-C, Pon CH, Yu J, Immediate effects of various physical medicine modalities on pain threshold of an active myofascial trigger pointJ Musculoskelet Pain 1993 1(2):37-53.Available from: http://www.tandfonline.com/doi/full/10.1300/J094v01n02_0410.1300/J094v01n02_04 [Google Scholar] [CrossRef]
[36]. Page P, Labbe A, Adhesive capsulitis: Use the evidence to integrate your interventionsN Am J Sports Phys Ther 2010 5(4):266-73.Available from: http://www.ncbi.nlm.nih.gov/pubmed/21655385%5Cnhttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC3096148 [Google Scholar]
[37]. Cleland J, Durall CJ, Physical therapy for adhesive capsulitis: Systematic reviewPhysiotherapy 2002 88(8):450-57.10.1016/S0031-9406(05)60847-4 [Google Scholar] [CrossRef]
[38]. Jason JI, Sundaram S G, Subramani M V, Physiotherapy interventions for adhesive capsulitis of shoulder: A systematic reviewInt J Physiother Res 2015 3(6):1318-25.Available from: http://www.ijmhr.org/ijpr.3.6/IJPR.2015.198.html10.16965/ijpr.2015.198 [Google Scholar] [CrossRef]
[39]. Alsubheen SA, Nazari G, Bobos P, MacDermid JC, Overend TJ, Faber K, Effectiveness of nonsurgical interventions for managing adhesive capsulitis in patients with diabetes: A systematic review. Vol. 100Archives of Physical Medicine and Rehabilitation 2019 W.B. Saunders:350-65.10.1016/j.apmr.2018.08.18130268804 [Google Scholar] [CrossRef] [PubMed]
[40]. Hsu JE, Anakwenze OA, Warrender WJ, Abboud JA, Current review of adhesive capsulitisJ Shoulder Elb Surg 2011 20(3):502-14.Available from: http://dx.doi.org/10.1016/j.jse.2010.08.02310.1016/j.jse.2010.08.02321167743 [Google Scholar] [CrossRef] [PubMed]
[41]. Hanchard NCA, Goodchild L, Thompson J, Brien TO, Davison D, Richardson C, Evidence-based clinical guidelines for the diagnosis, assessment and physiotherapy management of contracted (frozen) shoulder: Quick reference summaryPhysiotherapy 2012 98(2):117-20.Available from: http://dx.doi.org/10.1016/j.physio.2012.01.00110.1016/j.physio.2012.01.00122507361 [Google Scholar] [CrossRef] [PubMed]
[42]. Dawson J, Shepperd S, Carr A, An overview of factors relevant to undertaking research and reviews on the effectiveness of treatment for frozen shoulderShoulder Elb 2010 2(4):232-37.Available from: http://sel.sagepub.com/lookup/doi/10.1111/j.1758-5740.2010.00067.x10.1111/j.1758-5740.2010.00067.x [Google Scholar] [CrossRef]
[43]. Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M, Reliability of the PEDro scale for rating quality of randomized controlled trialsPhys Ther 2003 83(8)):713-21.Available from: http://www.ncbi.nlm.nih.gov/pubmed/12882612 [Google Scholar]
[44]. NIH National Heart, Lung and Blood Institute . Study quality assessment tools. Available from: https://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools [Google Scholar]
[45]. Lewit K, Manipulative Therapy in Rehabilitation of the Locomotor System 1991 2nd edButterworth Heinemann:204-205. [Google Scholar]
[46]. Kostopoulos D, Rizopoulos K, Effect of topical aerosol skin refrigerant (Spray and Stretch technique) on passive and active stretchingJ Bodyw Mov Ther 2008 12(2):96-104.10.1016/j.jbmt.2007.11.00519083662 [Google Scholar] [CrossRef] [PubMed]
[47]. Jeyakumar S, Alagesan J, Jayashree PR, A comparative study on the effectiveness of myofascial trigger point release and maitland techniques in adhesive capsulitis of shoulder jointInternational Journal of Medicine & Health Research 2016 2(1):01-07. [Google Scholar]
[48]. Kumar S, AP. Research Report AbstractsPhysiotherapy 2011 97(97):eS18-1415.Available from: https://linkinghub.elsevier.com/retrieve/pii/S003194061100069110.1016/j.physio.2011.04.002 [Google Scholar] [CrossRef]
[49]. Niel-Asher S, Hibberd S, Bentley S, Reynolds J, Adhesive capsulitis: Prospective observational multi-center study on the Niel-Asher technique (NAT)Int J Osteopath Med 2014 17(4):232-42.Available from: http://dx.doi.org/10.1016/j.ijosm.2014.06.00210.1016/j.ijosm.2014.06.002 [Google Scholar] [CrossRef]
[50]. Clewley D, Flynn TW, Koppenhaver S, Trigger point dry needling as an adjunct treatment for a patient with adhesive capsulitis of the shoulderJ Orthop Sport Phys Ther 2014 44(2):92-101.Available from: http://www.jospt.org/doi/10.2519/jospt.2014.491510.2519/jospt.2014.491524261931 [Google Scholar] [CrossRef] [PubMed]
[51]. Jankovic D, van Zundert A, The frozen shoulder syndrome. Description of a new technique and five case reports using the subscapular nerve block and subscapularis trigger point infiltrationActa Anæsthesiologica Belgica 2006 (3):137-43.Available from: http://www.sarb.be/nl/tijdschrift/artikels_acta_2006/artikels_acta_57_2/07-jankovic.pdf [Google Scholar]