Introduction
Diabetes Mellitus (DM) is a multisystem metabolic disorder. The techniques of anaesthesia, specifically the usage of general and regional anaesthesia can change (or) modify any residual insulin secretion and catabolic hormones secretion.
Aim
To compare and determine the perioperative and postoperative changes in the blood glucose, Blood Pressure (BP), Heart Rate (HR) and Visual Analog Scale (VAS) pain score among the diabetic patients under regional and general anaesthesia.
Materials and Methods
A retrospective study of 100 diabetic patients who had undergone surgeries under general and regional anaesthesia was performed. The patients were divided into two groups based on the type of anaesthesia used during surgery. Information pertaining to the level of blood glucose, BP and HR of the diabetic patients under general and regional anaesthesia were retrieved and analysed. Statistical analyses was performed to determine the significance of any differences observed between the two groups.
Results
The study revealed that the blood glucose level among the diabetic patients under general and regional anaesthesia was found to be higher in post surgery period when compared to the blood glucose level among the patients in pre surgery period under general and regional anaesthesia. The study also reported that the level of Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP) and HR among the diabetic patients during surgery under general and regional anaesthesia decreased when compared to the level of SBP among the patients at pre surgery under both general and regional anaesthesia. The level of the SBP post surgery under regional anaesthesia remained the same as pre surgery level. VAS pain score among the patients in general anaesthesia group was found to increase almost instantly after the completion of surgery while that among the regional anaesthesia group was found to increase only after the 3rd or 4th hour of post-surgery.
Conclusion
The study concludes that there was an increased intraoperative blood glucose fluctuation, alterations in the BP and HR level among the diabetic patients upon administration of both general and regional anaesthesia.
Blood glucose, Diastolic blood pressure, Heart rate, Systolic blood pressure, Visual analog scale
Introduction
DM is a multisystem metabolic disorder, and number of diabetic patients are increasing strongly in recent years [1]. According to a study performed in a community-based sample of 51,117 persons ageing 20 years and above in over 14 states and 1 union territory in India in 3 different phases, there is a widespread of DM in rural and urban India with few areas reporting prevalence rate of 13% [2]. An examination demonstrated 2 to 4% of surgical patients have diabetes. Perioperative patients who have diabetes could prompt a sharp rise in blood glucose, causing the expanded occurrence of acute complications and infections, postoperative mortality and delayed wound healing related to diabetes [3]. Despite enormous advances in management, diabetes patients may in any case experience microvascular and cardiovascular complications, which may clarify their requirement for surgery more frequently than non-diabetes patients. For example, diabetes associated microvascular complications includes retinopathy, neuropathy and nephropathy which tends to have a long-term effect on the small blood vessels. Cardiovascular complications of diabetes involve complete blockade of blood vessels leading to increased risk for myocardial infarction, gangrene and stroke [4,5]. It has been reported that there is an increased perioperative risk during surgery, infusions, administration of anaesthesia and various associated problems among diabetic patients. Consequently, diabetes patients should be given special attention before, during and after surgery [6].
The pervasiveness of DM in both children and adults have been rising all through the world for the past 20-30 years [7]. Current alterations in diagnostic criteria, if broadly adopted, will probably also lead to more patients being named as having diabetes [8]. Unsurprisingly, diabetic patients posted for surgery due to their disease, or incidental surgery, will put a rising problem on anaesthetic services. To decrease the traditional tactics and hospital stay for managing preoperative diabetic patients inclined on a term of inpatient perioperative ‘stabilisation’ that battle between the economic needs.
The techniques of anaesthesia, specifically the usage of general and regional anaesthesia can change (or) modify any residual insulin secretion and catabolic hormones secretion. Mainly during cataract surgery the local anaesthesia is preferred for some measures in patients with diabetes. The patients with diabetes, the basic one to be noted is that the risk of nerve injury is higher when compared to anaesthetic requirements. Early mobilisation is facilitated by local anaesthesia (after and before surgery), and also avoids metabolic and hormonal alterations that takes place during general anaesthesia. Therefore, local anaesthesia promotes least intrusion of the usual daily repetitive of diet, and treatment for patients with diabetes. However, there is a threat of epidural abscess, profound hypertension and vascular damages [9]. The alteration arises due to the combined effect of decreased insulin secretion as well as insulin resistance. The increased secretion of catecholamines growth hormone and cortisol that leads to transformed post-receptor insulin binding and subsequent decrease in trans-membrane glucose transport creates resistance in insulin. Previous study has reported that there is a perioperative increase in the concentration of circulating glucose, epinephrine and cortisol concentrations observed among patients when they are exposed to surgical stress under anaesthesia [10]. The stress response during surgery itself may lead to diabetic crisis such as diabetic ketoacidosis, hyperglycaemic hyperosmolar syndrome perioperatively or postoperatively, with negative prognostic outcomes. Therefore, it is very crucial that utmost attention to be paid to the metabolic status of diabetic patients undergoing surgery [11]. According to a study, administration of general anaesthesia, among hypertensive patients may lead probably to increase in HR and BP because of the agents that are often used for hypotension [12]. However, till date there are no concrete reports on the mortality and major complications associated with the use of general or regional anaesthesia among diabetic patients during minor surgeries. McAnulty GR et al., reported that surgery performed in diabetic patients with neural blockade were found to resume oral intake much before than after general anaesthesia. It has also been reported that diabetic patients with autonomic neuropathy may carry an increased risk if performed using regional anaesthesia [10]. However, there is no evidence that whether regional anaesthesia alone, or combined with general anaesthesia, provide any advantage among the diabetic patients during surgery, in regard of mortality and major complications. Therefore, this study has been undertaken to retrospectively compare amid general anaesthesia and regional anaesthesia in diabetic patients, the changes in the blood glucose level during pre and postoperative procedures and to determine if there are any differences observed among them. The study would also compare the BP and HR level during preoperative, intraoperative and postoperative procedures. Lastly, the study would also focus on the postoperative VAS pain score among the diabetic patients during general and regional anaesthesia.
Materials and Methods
The present study was retrospective where the records of every diabetic patient who had undergone surgeries between June 2017 to May 2019 in the Department of Orthopedics and General Surgery were retrieved. The records of patients suffering from both Type 1 and 2 diabetes mellitus were retrieved for the study. From the records the data relating to several demographic information, type of anaesthesia used and every clinical parameter such as BP, HR, blood glucose level during surgery, pre and postsurgery was retrieved. Since it was retrospective study so ethical clearance was not required. For the study, the data of 100 diabetic patients were chosen among each and every record of the patients retrieved. From the records, the data related to types of diabetic drugs such as Metformin and Glimepride were administered to the type 2 diabetic patients to maintaining the normal blood sugar level amid patients before surgery were also collected. Patients with type 1 diabetes mellitus were treated with human insulin (actrapid) according to level of blood sugar. The study cases were branched into two groups. Based on the anaesthesia type, study cases were classified in either one of the two groups. The first group consisted of 51 diabetic patients (Type 1=5, Type 2=46) undergoing surgery under general anaesthesia while the second group consisted of 49 diabetic patients (Type 1=4, Type 2=45) undergoing surgery under regional anaesthesia. Before performing the surgery, every patient was directed to the anaesthetic consultation in the study. For each and every patient the SBP, DBP, blood sugar level (%) and HR were recorded before surgery, during surgery and after surgery. For all the patients’ blood sugar was measured on the day of surgery (both diabetes type 1 and type 2). For the study, the VAS pain score of postsurgery among the patients of both the groups were retrieved. For the study, various aetiological habits (smoking, alcohol consumption) and demographic characteristics of the study cases were also recorded and retrieved.
Inclusion Criteria
Patients with type 1 and 2 diabetes mellitus as comorbidity who have undergone surgeries between June 2017 to May 2019 in the Department of Orthopedics and General Surgery, ACS Medical College and Hospital were included.
Exclusion Criteria
Patients with incomplete clinical data record were excluded from the study.
Anaesthetic Management and Intraoperative Care
For the study, the cases selected includes diabetic patients who were operated for femoral hernia, inguinal hernia, circumcision, hydrocele, calcaneal fracture, fracture fibula, metatarsal fracture, fracture fibula under regional anaesthesia and those who were operated for lipoma over chest wall, fibroadenoma, infected sebaceous cyst over back, infected sebaceous cyst over chest wall, fracture proximal humerus, lipoma over back under general anaesthesia. All patients were premedicated with inj midazolam 1-1.5 mg, inj glycopyrolate 0.2 mg. Insulin and oral hypoglycaemic drugs (metformin and glimepride) were omitted on the day of surgery. With fentanyl 2 μg kg-1 and propofol 2.5 mg kg-1 the general anaesthesia was initiated. After orotracheal intubation encouraged by atracurium 0.5 mg kg-1 the anaesthesia level was maintained up to 0.7-1.5% end-tidal sevoflurane. Between the L3-L4 intervertebral spaces, using a 25 Gauge spinal needle with spinal block the regional anaesthesia was administered. Regional anaesthesia was administered with injection of 3.2-3.6 mL hyperbaric bupivacaine [13].
Statistical Analysis
All the statistical analyses for the study were performed using the SPSS ver 24 software. The significant data from the study were given either as percentages or mean/median. In the study subjects the statistical significance among the aetiological and demographic limits was evaluated using Chi-square test in order to determine any variability. By using t-test, the statistical significance of the difference in the VAS pain score between the general and regional anaesthesia group were calculated. For p<0.05 each and every test were considered as significant.
Results
The study was performed using the medical records of 100 patients with diabetes retrieved from the Department of Orthopedics and General Surgery undergoing surgery either under regional or general anaesthesia. It has been observed from the study that in 49% of the study subjects’ surgeries were performed under regional anaesthesia while in 51% of the study subjects’ surgeries were performed under general anaesthesia. The mean age ±SD of the study subjects for surgeries performed under regional and general anaesthesia was observed to be 24.9±2.4 and 25.9±2.6 years respectively. The mean value±SD of BMI of the study subjects in the regional and general anaesthesia group was observed to be 23.2±2.3 and 24±1.8, respectively [Table/Fig-1].
Demographic, aetiological and clinical characteristics of the study subjects with hypertension.
| General anaesthesia (mean±SD/percentage) | Regional anaesthesia (mean±SD/percentage) | p-valueab |
|---|
| Age | 25.9±2.6 | 24.9±2.4 | 0.05b |
| Gender | Male | 60.4% | 39.6% | 0.07a |
| Female | 42.3% | 57.7% |
| BMI | 24±1.8 | 23.2±2.3 | <0.05b |
| Alcohol | Yes | 35% | 65% | 0.1a |
| No | 55% | 45% |
| Smoking | Yes | 65.6% | 34.4% | <0.05a |
| No | 44.1% | 55.9% |
aChi-square test; bt-test
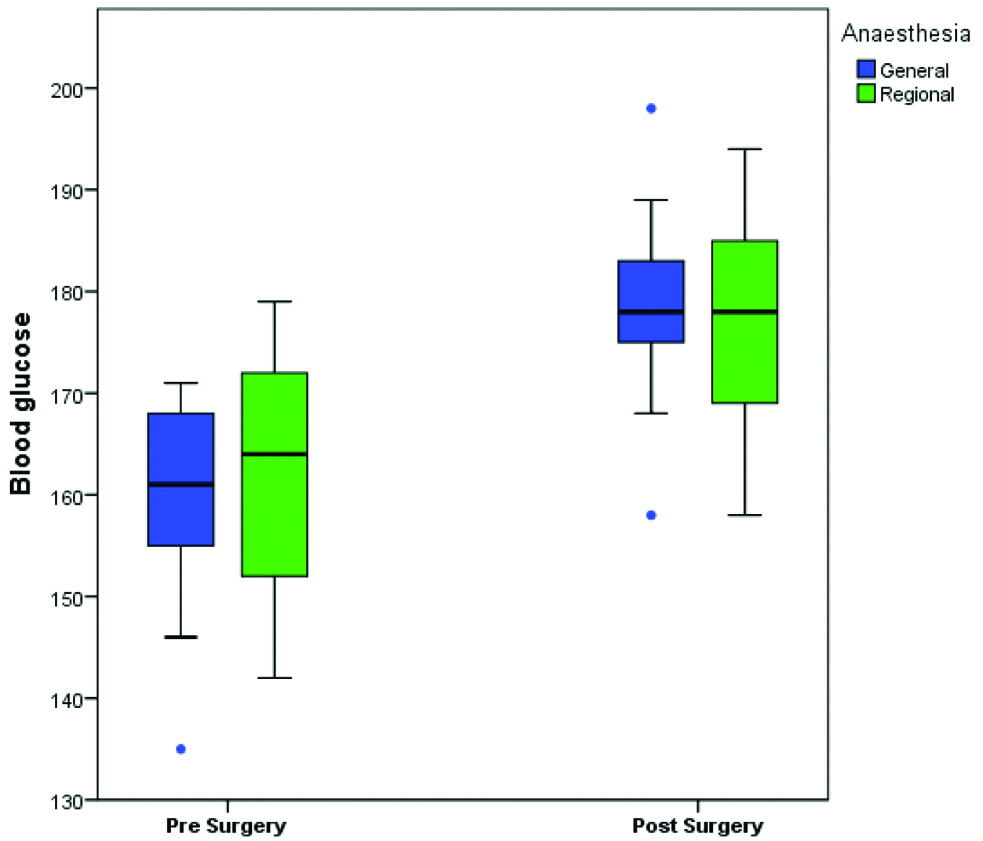
The differences in the level of the blood glucose pre surgery and post surgery among the cases of both the general anaesthesia and regional anaesthesia groups were found to be statistically significant (p<0.01).
It was observed from the study that the blood glucose level among the diabetic patients under general and regional anaesthesia was found to be higher in post surgery when compared to the blood glucose level among the patients in pre surgery under general and regional anaesthesia [Table/Fig-2].
Blood glucose level of the study subjects pre and post surgery under general and regional anaesthesia.
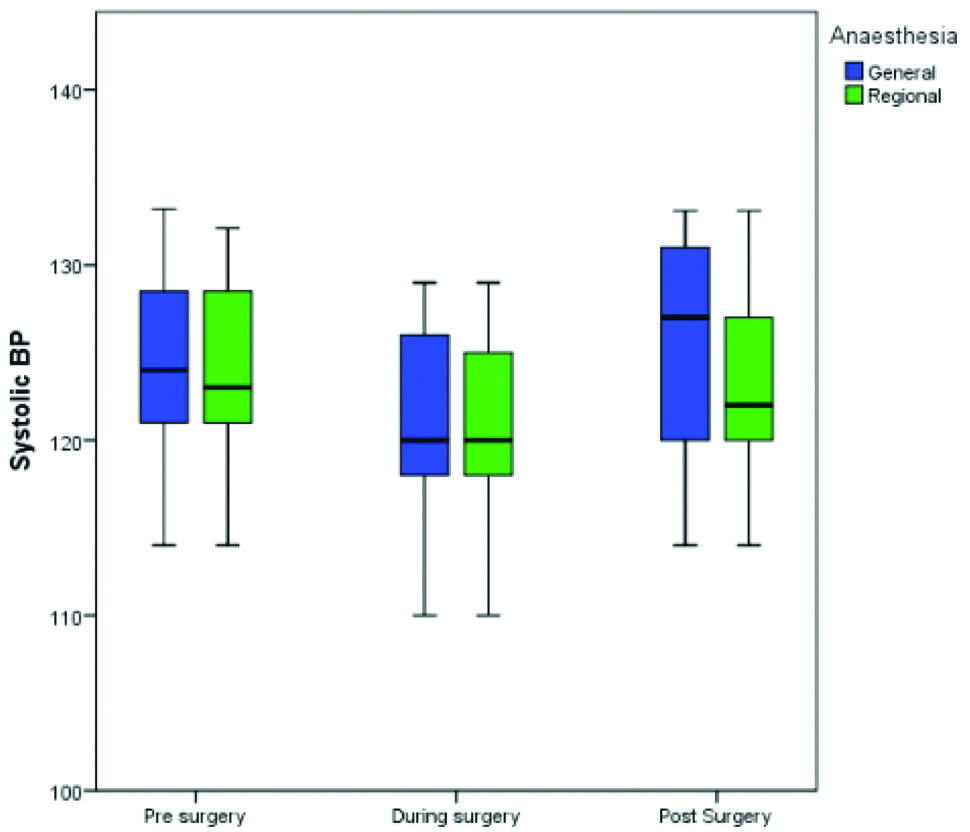
It was observed from the study that the level of SBP among the diabetic patients during surgery under general and regional anaesthesia decreased in comparison to pre surgery levels. However, the level of SBP at post surgery under general anaesthesia increased in comparison to pre surgery level. The level of the SBP at post surgery under regional anaesthesia remains the same as pre surgery level [Table/Fig-3].
Systolic blood pressure among the diabetic cases pre, during and post surgery performed using either general or regional anaesthesia.
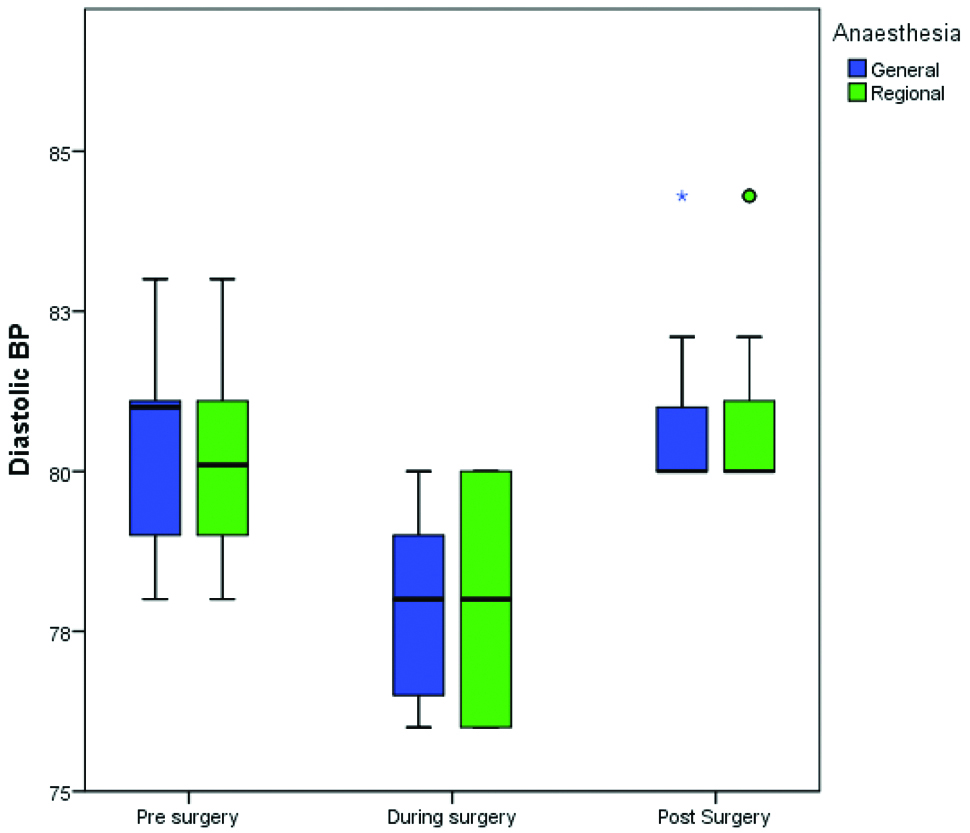
It was observed from the study that the level of DBP among the diabetic patients during surgery under general and regional anaesthesia decreased in comparison to pre surgery level. The level of DBP at post surgery under general and regional anaesthesia remained the same as the pre surgery level [Table/Fig-4].
Diastolic blood pressure among the diabetic cases pre, during and post surgery performed using either general or regional anaesthesia.
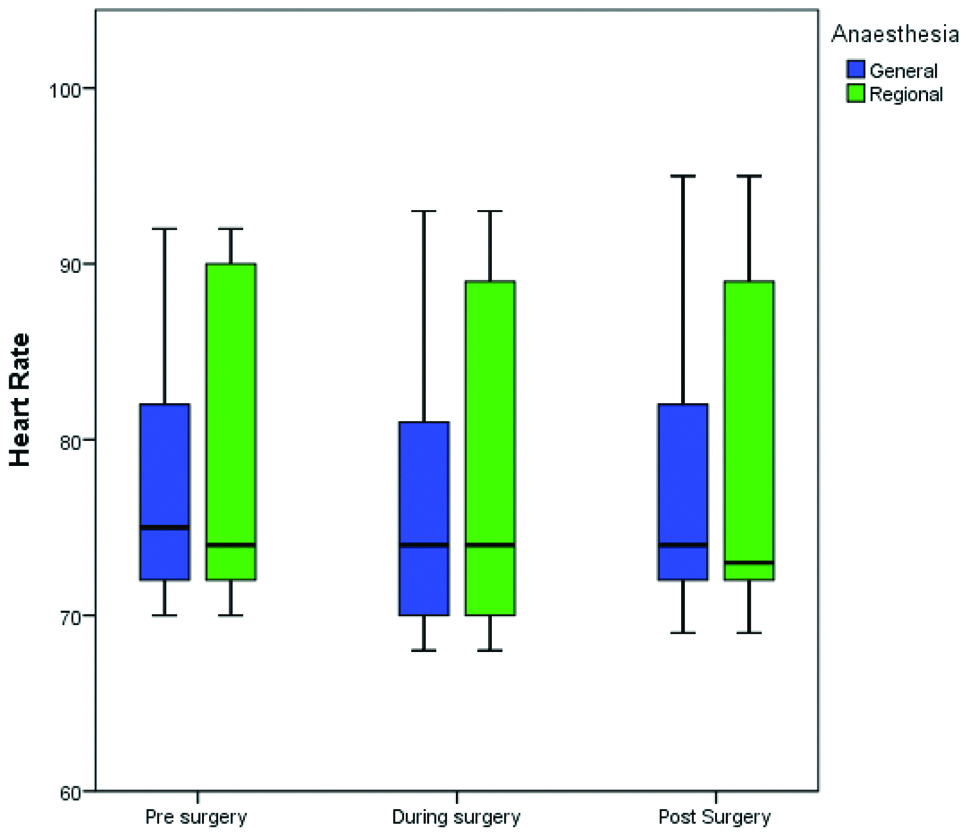
It was observed that HR among the diabetic patients during surgery decreased in comparison to pre surgery levels under general and regional anaesthesia. The level of HR among the patients at post surgery remained the same with the pre surgery levels under both general and regional anaesthesia [Table/Fig-5].
Heart rate among the diabetic cases pre, during and post surgery performed using either general or regional anaesthesia.
According to the study subjects, it was observed that the median of VAS pain score amid the patients in general anaesthesia group was found to increase almost instantly after the completion of surgery attaining a peak during the 3rd hour of post surgery. However, only after the 3rd or 4th hour of post surgery the VAS pain score among the patients of the regional anaesthesia group was found to increase by reaching a peak post 6 hours of surgery. Among the patients of the general and regional anaesthesia group, there was a significant difference observed in the VAS pain score before the administration of analgesic drug [Table/Fig-6]. As per the case records, among the patients the rescue analgesic was administered when the VAS score was found to be more than 5 post surgery. In post rescue analgesic the VAS pain score was found to be reduced among both the analgesic group.
Median VAS pain score among the diabetic cases post surgery performed using either general or regional anaesthesia.
| Time post-surgery | Median value of VAS pain score among General Anaesthesia patients | Median value of VAS pain score among Regional Anaesthesia patients | p-value |
|---|
| 0 hr | 2 | 1 | <0.05 |
| 1 hr | 3 | 1 | <0.05 |
| 2 hr | 5 | 1 | <0.05 |
| 3 hr | 6 | 2 | <0.05 |
| 4 hr | 4 | 3 | - |
| 5 hr | 2 | 4 | - |
| 6 hr | 1 | 6 | - |
| 7 hr | 1 | 3 | - |
| 8 hr | 1 | 2 | - |
| 9 hr | 1 | 1 | - |
| 10 hr | 1 | 1 | - |
| 11 hr | 1 | 1 | - |
| 12 hr | 1 | 1 | - |
Discussion
Diabetes is rapidly progressing as a potential epidemic in India where it is estimated that over 62 million individuals are currently being diagnosed with diabetes. As per Wild S et al., it is anticipated that the pervasiveness of diabetes among people universally would double from an expected 171 million in the year 2000 to 366 million in the year 2030 where the maximum rise would be detected in India [14]. Due to the increased prevalence of diabetes in the general population, anaesthetists must understand that a large percentage of patients with diabetes would show up during surgeries. Therefore, the anaesthetists are not only expected to have adequate knowledge of the various complications and comorbidities found to be associated with diabetes but should also have proper knowledge of the pharmacokinetics and pharmacodynamics of different diabetic medicines [15]. Anaesthetic techniques, such as spinal, epidural, splanchnic or other regional blockade, might play a role in modulating catabolic hormones secretion as well as residual insulin secretion. It has been reported that epidural anaesthesia blocks the increased glucose circulation, epinephrine and concentrations of cortisol among non-diabetic patients lying under the surgical strain is not seen in the patients under general anaesthesia [10]. This study on the effect of type of anaesthesia on revealed that the blood glucose level among the diabetic patients under general and regional anaesthesia was found to be higher in post surgery when compared to the blood glucose level among the patients in pre surgery under general and regional anaesthesia indicating that the role of anaesthesia in increasing the blood glucose level among the patients post surgery irrespective of the type of anaesthesia administered. The results of a study done by Norman JG and Fink GW, demonstrates that the preference of anaesthesia technique affects intraoperative stress response and thus drastically affects the outcome and morbidity of surgical patients and the reduction of post operative pain [16]. This study was found to be consistent with Sudhakaran S and Surani SR, where it was reported that anaesthesia combined with surgical stress might lead to hyperglycaemia among diabetic patients [17]. However, in a study by Rehman HU and Mohammed K, it was reported that general anaesthesia was found to be more often associated with increased blood glucose level and increased catecholamines, cortisol, and glucagon levels in comparison to regional anaesthesia [18]. In another study done by Scherpereel P and Tavernier B, illustrated that the general anaethesia results in high blood glucose concentration than local and epidural analgesia [19]. The increase in the blood glucose level in the study can be explained by the fact that sympathoadrenal stimulation are observed in previuos studies due to the consequence of stress reponse and general anaesthetic agents like sevoflurane which may result in severe metabolic changes such as inhibition of insulin secretion leading to increased blood glucose level [20,21].
The study also reported that the level of SBP, DBP and HR among the diabetic patients during surgery under general and regional anaesthesia decreased when compared to the level of SBP among the patients at pre surgery under both general and regional anaesthesia. The level of the systolic BP at post surgery under regional anaesthesia remains the same as pre surgery level. The level of the DBP and level of the HR among the patients from both the general and regional anaesthesia group post surgery were found to be comparable to that at the pre surgery level. In a study by Sato M et al., it was reported that the BP of the individuals were found to get reduced under general anaesthesia due to which there is an induction in propofol with a depression in the response of the cardiac baroreflex [22]. It was also reported that the decrease of the BP among the patients was reported to be less pronounced under the influence of regional anaesthesia. The findings were found to be consistent with the present study where the patieints under regional anaesthesia were obersved to normal level of DBP similar to the baseline values post surgery. The possible explaniation for the observed results can be explained form the fact that after the induction dose of propofol during general anaesthesia, there is an observed drop of BP in majority of the cases which may require therapy post surgery to bring down the BP to the normal levels [23].
The VAS pain score among the patients in general anaesthesia group was found to increase almost instantly after the completion of surgery while that among the regional anaesthesia group was found to increase only after the 3rd or 4th hour of post surgery. This observation was found to be consistent with Wang XX et al., it was reported that spinal regional anaesthesia may be associated with less post operative pain and post operative nausea and vomiting compared with general anaesthesia [24].
Limitation
The limitation of the study was that it was constrained to a small sample size among both the general and regional anaesthesia group due to which the study failed to notice any minor differences in the various clinical parameters between the groups. It is therefore recommended to conduct the study in a larger sample size in future research.
Conclusion
The study concludes that there was an increased intraoperative blood glucose fluctuation, alterations in the BP and HR level among the diabetic patients upon administration of both general and regional anaesthesia. However, there was a reduced post operative pain among the patients in the regional anaesthesia group in comparison to those under general anaesthesia group.
aChi-square test; bt-test
Author Declaration:
Financial or Other Competing Interests: No
Was Ethics Committee Approval obtained for this study? No
Was informed consent obtained from the subjects involved in the study? NA
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Aug 16, 2019
Manual Googling: Oct 04, 2019
iThenticate Software: Oct 28, 2019 (7%)
[1]. Li X, Wang J, Chen K, Li Y, Wang H, Mu Y, Effect of different types of anaesthesia on intraoperative blood glucose of diabetic patients: A PRISMA-compliant systematic review and meta-analysisMedicine 2017 96(13):e645110.1097/MD.000000000000645128353577 [Google Scholar] [CrossRef] [PubMed]
[2]. Rajadhyaksha V, Managing diabetes patients in India: Is the future more bitter or less sweet?Perspectives in Clinical Research 2018 9(1):01-03.Epub 2018/02/1310.4103/picr.PICR_161_1729430410 [Google Scholar] [CrossRef] [PubMed]
[3]. Wei J, Li C, Zhang J, Zhang B-H, Li J, Yin H-Q, Related polymorphism and logistic analysis of surgical anaesthesia in diabetes patientsProg Modern Biomed 2011 11:3721-23. [Google Scholar]
[4]. Pantalone KM, Hobbs TM, Wells BJ, Kong SX, Kattan MW, Bouchard J, Clinical characteristics, complications, comorbidities and treatment patterns among patients with type 2 diabetes mellitus in a large integrated health systemBMJ open Diabetes Research & Care 2015 3(1):e000093Epub 2015/07/2910.1136/bmjdrc-2015-00009326217493 [Google Scholar] [CrossRef] [PubMed]
[5]. Vinik AI, Vinik E, Prevention of the complications of diabetesAmerican Journal of Managed Care 2003 9(3; SUPP):S63-S80. [Google Scholar]
[6]. Cosson E, Catargi B, Cheisson G, Jacqueminet S, Ichai C, Leguerrier A, Practical management of diabetes patients before, during and after surgery: A joint French diabetology and anaesthesiology position statementDiabetes Metab 2018 44:200-16.10.1016/j.diabet.2018.01.01429496345 [Google Scholar] [CrossRef] [PubMed]
[7]. Gardner SG, Bingley PJ, Sawtell PA, Weeks S, Gale EA, Rising incidence of insulin dependent diabetes in children aged under 5 years in the Oxford region: time trend analysisBMJ 1997 315(7110):713-17.10.1136/bmj.315.7110.7139314756 [Google Scholar] [CrossRef] [PubMed]
[8]. Borch-Johnsen K, DECODE study group on behalf of the European Diabetes Epidemiology Study Group. Will new diagnostic criteria for diabetes mellitus change phenotype of patients with diabetes? Reanalysis of European epidemiological dataBMJ 1998 317:371-75.10.1136/bmj.317.7155.3719694750 [Google Scholar] [CrossRef] [PubMed]
[9]. Joshi GP, Chung F, Vann MA, Ahmad S, Gan TJ, Goulson DT, Society for Ambulatory Anaesthesia consensus statement on perioperative blood glucose management in diabetic patients undergoing ambulatory surgeryAnaesthesia & Analgesia 2010 111(6):1378-87.10.1213/ANE.0b013e3181f9c28820889933 [Google Scholar] [CrossRef] [PubMed]
[10]. McAnulty GR, Robertshaw HJ, Hall GM, Anaesthetic management of patients with diabetes mellitusBritish Journal of Anaesthesia 2000 85(1):80-90.Epub 2000/08/0610.1093/bja/85.1.8010927997 [Google Scholar] [CrossRef] [PubMed]
[11]. Dagogo-Jack S, Alberti KGM, Management of diabetes mellitus in surgical patientsDiabetes Spectrum 2002 15(1):44-48.10.2337/diaspect.15.1.44 [Google Scholar] [CrossRef]
[12]. Goldman L, Caldera DL, Risks of general anaesthesia and elective operation in the hypertensive patientAnaesthesiology 1979 50(4):285-92.Epub 1979/04/0110.1097/00000542-197904000-00002434530 [Google Scholar] [CrossRef] [PubMed]
[13]. Acikel A, Ozturk T, Goker A, Hayran GG, Keles GT, Comparison of patient satisfaction between general and spinal anaesthesia in emergency caesarean deliveriesTurkish Journal of Anaesthesiology and Reanimation 2017 45(1):41-46.Epub 2017/04/0610.5152/TJAR.2017.3815928377839 [Google Scholar] [CrossRef] [PubMed]
[14]. Wild S, Roglic G, Green A, Sicree R, King H, Global prevalence of diabetes: Estimates for the year 2000 and projections for 2030Diabetes care 2004 27(5):1047-53.Epub 2004/04/2810.2337/diacare.27.5.104715111519 [Google Scholar] [CrossRef] [PubMed]
[15]. Cornelius BW, Patients With Type 2 Diabetes: Anaesthetic management in the ambulatory setting: part 2: Pharmacology and guidelines for perioperative managementAnaesthesia Progress 2017 64(1):39-44.Epub 2017/01/2810.2344/anpr-64-01-0228128657 [Google Scholar] [CrossRef] [PubMed]
[16]. Norman JG, Fink GW, The effects of epidural anaesthesia on the neuroendocrine response to major surgical stress: a randomized prospective trialThe American Surgeon 1997 63(1):75-80. [Google Scholar]
[17]. Sudhakaran S, Surani SR, Guidelines for perioperative management of the diabetic patientSurgery Research and Practice 2015 2015:284063Epub 2015/06/1710.1155/2015/28406326078998 [Google Scholar] [CrossRef] [PubMed]
[18]. Rehman HU, Mohammed K, Perioperative management of diabetic patientsCurrent Surgery 2003 60(6):607-11.Epub 2004/02/2010.1016/j.cursur.2003.07.00214972202 [Google Scholar] [CrossRef] [PubMed]
[19]. Scherpereel P, Tavernier B, Perioperative care of diabetic patientsEuropean Journal of Anaesthesiology 2001 18(5):277-94.10.1097/00003643-200105000-00002 [Google Scholar] [CrossRef]
[20]. Kazmi MN, Assessment of blood glucose levels under general anaesthesia in diabetic patientsInternational Journal of Medical and Health Research 2017 3(3):138-40. [Google Scholar]
[21]. Kumar M, Tripathi M, Malviya D, Malviya P, Kumar V, Tyagi A, Influence of two anaesthetic techniques on blood sugar level in head injury patients: A Comparative StudyAnaesthesia, Essays and Researches 2016 10(2):20710.4103/0259-1162.17233527212748 [Google Scholar] [CrossRef] [PubMed]
[22]. Sato M, Tanaka M, Umehara S, Nishikawa T, Baroreflex control of heart rate during and after propofol infusion in humansBr J Anaesth 2005 94(5):577-81.Epub 2005/02/2210.1093/bja/aei09215722386 [Google Scholar] [CrossRef] [PubMed]
[23]. Janssen H, von Stosch R, Pöschl R, Büttner B, Bauer M, Hinz JM, Blood pressure response to combined general anaesthesia/interscalene brachial plexus block for outpatient shoulder arthroscopyBMC Anaesthesiology 2014 14(1):5010.1186/1471-2253-14-5025002832 [Google Scholar] [CrossRef] [PubMed]
[24]. Wang XX, Zhou Q, Pan DB, Deng HW, Zhou AG, Guo HJ, Comparison of postoperative events between spinal anaesthesia and general anaesthesia in laparoscopic cholecystectomy: a systemic review and meta-analysis of randomized controlled trialsBioMed Research International 2016 2016:948053910.1155/2016/948053927525282 [Google Scholar] [CrossRef] [PubMed]