Cryptogenic Organising Pneumonia as Main Presenting Feature of Rheumatoid Arthritis
Sunil Kumar1, Amrutha Garikapatti2, Amole Andhale3, Atma Nayak4
1 Professor, Department of Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Wardha, Maharashtra, India.
2 Postgraduate Resident, Department of Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Wardha, Maharashtra, India.
3 Postgraduate Resident, Department of Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Wardha, Maharashtra, India.
4 Postgraduate Resident, Department of Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Wardha, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sunil Kumar, Professor, Department of Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences (Deemed to be University), Wardha, Maharashtra, India.
E-mail: sunilkumarmed@gmail.com
Cryptogenic Organising Pneumonia (COP) has been associated with several connective tissue disorders, but very rarely with rheumatoid arthritis. Here, the present authors report a 60-year-old female who presented with breathlessness on exertion, cough, fever, and multiple joint pains mainly of wrist and fingers as the main symptoms. On investigation, the RA factor and anti-CCP Abs were positive. She was diagnosed as COP on the basis of High Resolution Computed Tomography of thorax.
Connective tissue disorders, Diagnosis, Elderly
Case Report
A 60-year-old female was admitted to the emergency department for breathlessness on exertion. She had fever, dry cough and joint pain in wrist and fingers of both the hands. She was on some irregular pain killer from local general practitioner since six months for joint pain. There was no history of ischaemic heart disease, hypertension, auto-immune disease or pulmonary tuberculosis. She was a non-smoker and non-alcoholic. There was no history of betel nut chewing or domestic animal pet exposure.
Her physical examination revealed pallor and bilateral basal crackles over the both lung field. Her pulse was 98/minute and regular and blood pressure was 140/90 mmHg. There were inflammation and tenderness over both the wrist and second metacarpal phalangeal and third proximal interphalangeal joints.
Her routine investigation revealed Peripheral white blood cell count as 6600 with 64% neutrophils, 22% lymphocytes and 13% monocytes. The haemoglobin value was 8.7 mg%. The erythrocyte sediment rate was 96 mm/hour. Routine biochemical investigations revealed normal renal and liver function tests. Tests for HIV using enzyme-linked immunosorbent assay were negative for both HIV 1 and 2. Her thyroid profile was normal. Blood reports were negative for dengue fever, malarial fever, scrub typhus.
Her chest radiograph showed an alveolar patch in both lower lung fields. Keeping the possibility of atypical pneumonia, she was treated with injectable Amoxycillin and Clavulanic acid 1.2 gm intravenously and oral Azithromycin 500 mg per day for 5 days. Her blood culture was negative. Sputum examination and bronchoalveolar lavage did not reveal any pathogen, acid-fast organisms or fungus.
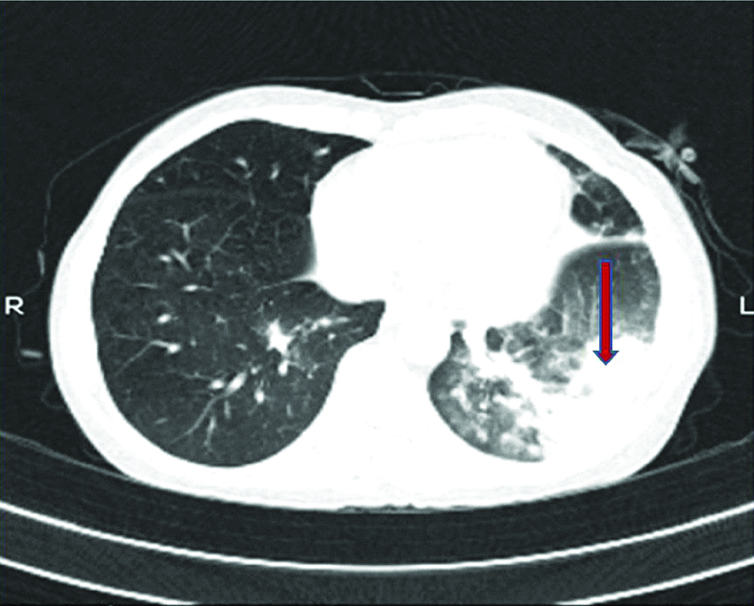
After one-week observation, there was no effect on symptoms of fever, cough, and breathlessness on exertion. Notably, serological examinations revealed positivity for RA factor and anti-Cyclic Citrullinated Peptide antibodies (anti-CCP Abs). Her C-reactive protein was also positive. As there was no response from treatment, High-Resolution Computed Tomography (HRCT) scan of chest was planned which revealed peribronchial and subpleural bilateral ground-glass opacities with air bronchograms. By these findings, possibilities of COP were considered [Table/Fig-1]. Her trans-bronchial lung biopsy examinations couldn’t be performed due to financial and feasibility constraints.
HRCT chest showing peribronchial and subpleural bilateral ground-glass opacities with air bronchograms (arrow).
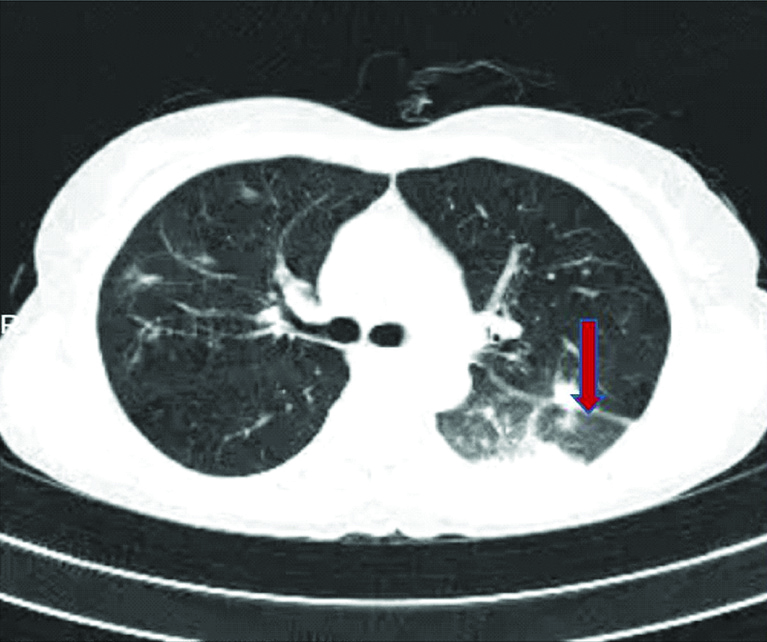
The patient was kept on intravenous methylprednisolone 1 gm daily for 5 days, after this there was marked improvement in her dyspnea on exertion and joint pain of wrist and fingers. The patient was then treated with prednisolone (30 mg/day), methotrexate 15 mg once a week; the prednisolone dose was tapered at the outpatient department to 5-10 mg/day within one month. She was doing well on follow-up clinically as well as radiologically after three months [Table/Fig-2].
HRCT of chest after 3 month showing improvement (arrow).
Discussion
The main characteristics of COP is intra-alveolar organisation while that of bronchiolitis obliterans an extension of such organising lesions to bronchiolar lumens as well as formation of plugs of fibrous tissue in the alveolar ducts, alveoli and the distal bronchiole [1,2]. Various causes of COP were reported to be associated with infection, inhalational exposure to toxins, drugs, collagen vascular diseases and connective tissue diseases like Rheumatoid Arthritis (RA), mixed connective tissue disease, dermatomyositis and polymyositis [2]. Although RA has various pulmonary manifestations, initial presentation with COP is rare [3]. Notably, patients with COP respond well to systemic steroid therapy and moreover by starting such early treatment further complications may be avoided. In this case, the elderly female with RA initially manifested as COP and responded to corticosteroids.
The pathology of the formation of COP may be injury to the alveolar epithelium as this is an inflammatory lung disease rather than a fibrosing process. [1] Patients with RA normally suffer from respiratory complications like bronchopneumonia, interstitial fibrosis, pleural fibrosis, pneumonic-type adenocarcinoma, pulmonary lymphoma, chronic eosinophilic pneumonia and alveolar haemorrhage which may have multiple alveolar densities on CT scan just like COP [4-6]. Out of all, pleural manifestation is most commonly reported (40-60%) [7].
Therefore, diagnosis of COP in association with RA must be carefully made and should be excluded from other pulmonary disorders. The diagnosis of COP is preferably made by lung biopsy. However, pathologic examination is must to exclude other respiratory manifestations as treatment might be ineffective against the wrong type of inflammatory response [8]. A study has shown that there is no evidence of RA in patient of COP without positive RA factor and anti-CCP antibodies [7]. There is also rare case report of COP and RA which occurred at the same time of the disease having high or moderate RA disease activity at the onset [8]. In the present case also, RA disease was moderately active with positive Rheumatoid factor and anti-CCP Abs.
Conclusion
This case report shows that COP may occur during the course of RA, as respiratory complication. Attention should be given to the presence of COP at the same time or before the diagnosis of RA. In such cases, pulmonary symptoms may be the main evidence of RA activity, and Measurement of anti-CCP Abs and Rheumatoid Factor should be advised in such patient. In a patient with RA having respiratory symptoms, HRCT examinations can be used for early differential diagnosis of pulmonary disease such as COP so that treatment can be started early to prevent early morbidity.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Sep 07, 2019
Manual Googling: Sep 23, 2019
iThenticate Software: Oct 25, 2019 (12%)
[1]. Al-Ghanem S, Al-Jahdali H, Bamefleh H, Khan A, Bronchiolitis obliterans organizing pneumonia: Pathogenesis, clinical features, imaging and therapy reviewAnnals of Thoracic Medicine 2008 3(2):67-75.10.4103/1817-1737.3964119561910 [Google Scholar] [CrossRef] [PubMed]
[2]. Mori S, Organizing pneumonia in rheumatoid arthritis patients: A case-based reviewClinical Medicine Insights: Circulatory, Respiratory and Pulmonary Medicine 2015 9(S1):69-80.10.4137/CCRPM.S2332726543387 [Google Scholar] [CrossRef] [PubMed]
[3]. Mori S, Cho I, Koga Y, Sugimoto M, A simultaneous onset of organizing pneumonia and rheumatoid arthritis, along with a review of the literatureMod Rheumatol 2008 18(1):60-66.10.3109/s10165-007-0004-118159567 [Google Scholar] [CrossRef] [PubMed]
[4]. Tanaka N, Kim JS, Newell JD, Rheumatoid arthritis-related lung diseases: CT findingsRadiology 2004 232(1):81-91.10.1148/radiol.232103017415166329 [Google Scholar] [CrossRef] [PubMed]
[5]. Kaushik P, Cooper ES, Banda VR, Vatsavai SR, Kaushik R, Bronchiolitis obliterans with organizing pneumonia in rheumatoid arthritis- A fatal case and short review of literatureRheumatol Int 2005 25(5):391-93.10.1007/s00296-004-0514-515378265 [Google Scholar] [CrossRef] [PubMed]
[6]. Komiya K, Teramoto S, Kurosaki Y, Organizing pneumonia with a positive result for anti-CCP antibodies as the first clinical presentation of rheumatoid arthritisIntern Med 2010 49(15):1605-07.10.2169/internalmedicine.49.360920686298 [Google Scholar] [CrossRef] [PubMed]
[7]. Hoshino C, Satoh N, Narita M, Kikuchi A, Inoue M, Organising pneumonia as the first manifestation of rheumatoid arthritisBMJ Case Rep 2011 35:5810.1136/bcr.11.2010.355822699479 [Google Scholar] [CrossRef] [PubMed]
[8]. Kinoshita Y, Sakamoto A, Hidaka K, Organizing pneumonia preceding rheumatoid arthritisCase Rep Pulmonol 2014 75(8):61910.1155/2014/75861924600522 [Google Scholar] [CrossRef] [PubMed]