Tuberculosis of Uterine Cervix Presenting with Recurrent Leucorrhoea in Guise of Carcinoma of Cervix
Rajnandini Prasad1, Mariam Khan2, Fariha Anjum3, Surabhi Bhoyar4, Neema Acharya5
1 Student, Department of Obstetrics and Gynaecology, DMIMSDU, Wardha, Maharashtra, India.
2 Student, Department of Obstetrics and Gynaecology, DMIMSDU, Wardha, Maharashtra, India.
3 Student, Department of Obstetrics and Gynaecology, DMIMSDU, Wardha, Maharashtra, India.
4 Student Department of Obstetrics and Gynaecology, DMIMSDU, Wardha, Maharashtra, India.
5 Professor and Head, Department of Obstetrics and Gynaecology, DMIMSDU, Sawangi Meghe, Wardha, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Neema Acharya, AF 5, Doctors Quarters, Avbr Hosp Campus, DMIMSDU, Wardha, Maharashtra, India.
E-mail: neemasacharya@gmail.com
Leucorrhea is a common gynaecologic symptom which affects quality of life of a women when it becomes recurrent. Tuberculosis (TB) as cause of abnormal looking cervix or growth on cervix is not commonly thought. We present a rare case who presented with recurrent leucorrhea having growth on cervix clinically appearing like cervical malignancy but on histopathology it was found to be TB of cervix.
Cervical cancer, Cervical tuberculosis, Recurrent vaginal discharge
Case Report
A 36-year-old para two lady presented to gynaecological clinic with history of recurrent leucorrhoea since 7-8 months. The discharge was copious and foul smelling, occasionally stained and associated with post coital bleeding. She also gave history of pelvic pain off and on and hypomenorrhea of same duration. Though the menstrual cycle was regular she complained of hypomenorrhea in preceding three months. She had taken treatment in the form of vaginal pessary and systemic antibiotics and antifungal medications but the symptoms persisted. There was no history of fever or loss of appetite or weight. There was no history of TB in the family.
On clinical examination she was well built and nourished. General and systemic examination was normal. Abdomen was soft and there was no lump or doughy feel of abdomen. There was no free fluid in abdomen. On per speculum examination both the lips of cervix were replaced by growth which was 2×2 cm in size, which bled on touch. Cervical os could not be identified. On palpation cervix was hard in consistency, non-tender, uterus was anteverted, anteflxed normal in size and shape and was mobile. The fornices were free of the disease as there was no puckering or growth felt through them. Per rectum examination revealed normal rectal mucosa not adherent to uterus or cervix. Colposcopy revealed irregularly raised area on both lips of cervix [Table/Fig-1] which became dense ace to-white [Table/Fig-2] and showed abnormal vascular pattern on green filter [Table/Fig-3].
Colposcopy findings showing both lips of cervix replaced by growth.

Dense ace to-white area (arrow) on colposcopy.
Cervix replaced by growth and abnormal vascular pattern.
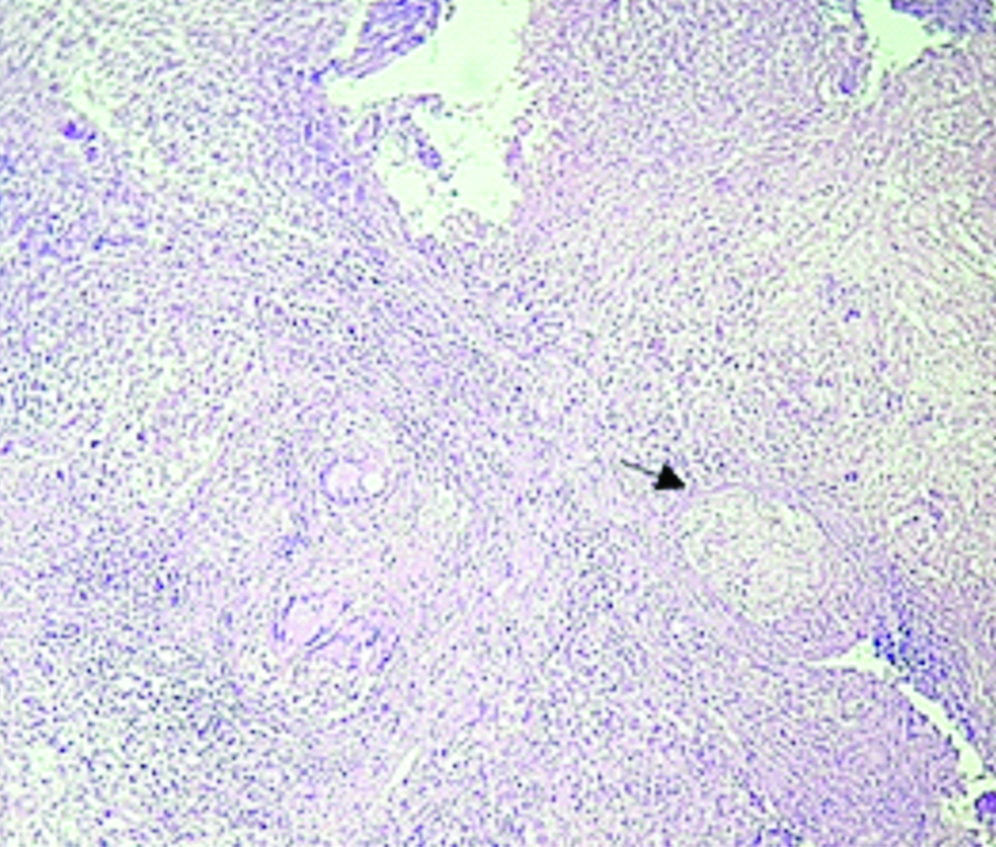
Cervical biopsy was taken and histopathology report revealed ulcerated overlying cervical epithelium composed of central areas of necrosis consisting of epithelod cells and surrounded by plasma cells and lymphocytes. All these features were suggestive of tubercular cervicitis [Table/Fig-4]. Dilatation and curettage was done but could not retrieve endometrial sample as it may have been scanty due to infective destruction as patient had evident hypomenorrhea too.
Granulomata (arrow) with central areas of caseous necrosis (H&E stain 10X Magnification).
Tests for HIV antibody and VDRL infections were carried out and it was negative. Chest radiograph was normal. Ultrasonography of the pelvis showed a normal sized uterus and normal bilateral adnexa not having any focal collection or mass. Acid Fast Bacilli (AFB) stain and culture was done on sputum, urine and cervical specimens, which was found to be negative. The Erythrocyte Sedimentation Rate (ESR) at 2 hours was 85 mm/hour and Mantoux test was positive. Patient was not willing for further testing for diagnosis due to financial constraints. She was then registered for DOTS (Directly Observed Treatment, Short- course) and started on anti-tubercular drugs as advised by respiratory physician. She has completed intensive phase of Anti-tubercular treatment and is currently on follow-up with remarkable improvement of symptoms.
Discussion
Leucorrhea is common in sexually active women. Most of the women receive treatment on basis of clinical judgment based on syndromic approach to symptoms. Recurrent or persistent leucorrhea is defined when patient has symptoms ≥4 episodes per year [1]. Our patient had more than four episodes of leucorrhea in preceding six months. She also had developed hypomenorrhea which could be due to thinning of endometrium associated with genital TB.
TB as a cause of leucorrhea and unhealthy cervix could be missed; though it is a common bacterial infection seen in developing countries. It is a frequent cause of upper genital tract infection leading to tubal infertility and chronic pelvic pain but rarely a cause of recurrent leucorrhoea. Almost 13% of the cases of pulmonary TB develop genital infection. The reported incidence of genital TB in India is about 3 to 16% among infertility cases. In upper genital tract infection, fallopian tubes are affected most commonly (90%), followed by the endometrium (50%) and the ovaries (10-30%). The cervix is rarely involved and accounts for 5% of the cases of genital tract TB and vagina-vulva in 1-2% cases. Genital TB in almost all cases is secondary to extra genital TB. TB of cervix is rare and clinical presentation may be misguiding as it appears like malignancy [2]. Patients don’t present with typical symptoms of TB and hence diagnosis could be missed or delayed [3]. The purpose of reporting this case is to highlight this rare presentation of common chronic infection in India and should be ruled out when patient has history of recurrent leucorrhoea and abnormal looking cervix. Mostly genital tract TB involvement may be through blood (90%), spread from other organs (e.g., Tuberculous peritonitis), lymph node involvement, and “vertical” spread through intercourse with an infected partner [4]. It has also been suggested that saliva and/or sputum, used as a sexual lubricant, might be a possible route of transmission [5].
TB of the female genital tract commonly presents with amenorrhoea, menstrual irregularities, infertility, chronic pelvic pain. Patients are generally young and present with foul smelling thick copious vaginal discharge, post coital bleeding. The gross appearances of the tuberculous cervix is of variable forms. May present as polypid, papillary, ulcerative, interstitial, endocervical or miliary [6]. As seen in our case colposcopy findings revealed dense aceto-white area with vegetative growth patterns on cervix suggestive of carcinoma cervix. As seen in [Table/Fig-4] in present case histopathology revealed caseating granuloma. Though the presence of granuloma does not confirm the diagnosis of TB, therefore it is essential to rule out possiblity of any other causes of granulomatous inflammation like foreign body reaction, schistosomiasis, amoebiasis, and sarcoidosis [6]. Gupta B et al., also reported two cases of unusual presentations of genital TB. Out of two cases they reported one had aceto-white raised areas on cervix and other case had similar findings with abnormal vascular pattern and cervical biopsies revealed granulomatous inflammation in both cases. They further stated that though separation of the Mycobacterium remains the gold standard for diagnosis, but in about one third of cases the culture obtained was found to be negative. Therefore, the presence of typical granulomata is sufficient for diagnosis; if other causes of granulomatous cervicitis are excluded or a primary focus is identified [5].
Bharani V et al., reported two cases where TB was diagnosed on cytology. They report that routine cervical cancer screening with cytology may reveal dyskaryosis and may also show the evidence of sparsely scattered Langhans’ type giant cells and granulomatous inflammation. These subtle findings should alert the pathologists to rule out TB [7]. Histopathological evaluation of punch biopsy specimen is important. Chronic inflammatory component with characteristic central necrosis i.e. caseating or non caseating is evident in most of the cases. In our case cytology of cervical smear was not done as there was profuse discharge covering the growth. Patient has completed intensive phase of anti-tubercular treatment and was relieved of symptoms.
As mentioned by Mandato VD et al., although rare, women without risk factors may also get affected by genital TB and hence it should be taken into account in the differential diagnosis of cervical cancer or growth on cervix [8]. Since TB of cervix is rare, its recognition and prompt diagnosis are very important because it can be mistaken for malignant or premalignant cervical neoplasia especially when it presents with growth.
As described by Jayakumar NKB most of the histopathology reports mention chronic inflammation as ‘nonspecific cervicitis’. They further suggest effort should be made to encourage specific reporting and thereby avoiding the term ‘nonspecific’ so that correct diagnosis and treatment can be offered specially in cases where symptoms keep recurring [2].
Sharma JB et al., mentioned that the treatment of TB is through multi-drug anti-tubercular treatment for adequate time period. The drugs used are rifampicin, isoniazid, pyrazinamide, ethambutol daily for 60 days followed by rifampicin, isoniazid, ethambutol daily for 120 day. Treatment is given for 18-24 months using the second-line drugs for Drug-Resistant (DR) cases. With the advent of increased access to rapid diagnostics and newer drugs the prognosis of most of the cases is good [9]. Surgery is rarely required except in cases resistant to medical treatment.
Conclusion
TB should be ruled out in cases of recurrent leucorrhoea or unhealthy non-malignant cervix and in low resource settings. Diagnosis can be based on clinical and histopathology findings as seen in our case for timely initiation of treatment.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Aug 22, 2019
Manual Googling: Oct 11, 2019
iThenticate Software: Oct 23, 2019 (15%)
[1]. discharge.pdf [Internet]. [cited 2019 Oct 6]. Available from: https://www.ouh.nhs.uk/microbiology/diagnostic-tests/atoz/documents/discharge.pdf [Google Scholar]
[2]. Jayakumar NKB, Cervicitis: How often is it non-specific!J Clin Diagn Res JCDR 2015 9(3):EC11-12.10.7860/JCDR/2015/11594.567325954624 [Google Scholar] [CrossRef] [PubMed]
[3]. Bekele D, Bekuretsion Y, Tuberculosis of the cervix mimicking cervical cancerEthiop Med J 2014 52(2):87-89. [Google Scholar]
[4]. Current Diagnosis and Management of Female Genital Tuberculosis [Internet]. [cited 2019 Aug 11]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4666212/ [Google Scholar]
[5]. Gupta B, Shree S, Rajaram S, Goel N, Genital tuberculosis: Unusual presentationsInt J Mycobacteriology 2016 5(3):357-59.10.1016/j.ijmyco.2016.06.01727847026 [Google Scholar] [CrossRef] [PubMed]
[6]. Kumari R, Vaishya V, Khanna G, Chauhan M, Sharma JB, Kriplani A, Tuberculosis of the cervix: An uncommon cause of vaginal discharge in a post-menopausal womanNatl Med J India 2018 31(3):149-50.10.4103/0970-258X.25575731044761 [Google Scholar] [CrossRef] [PubMed]
[7]. Bharani V, Gupta N, Suri V, Rajwanshi A, Tuberculosis in Pap samples with emphasis on LBC: Caught only when thoughtDiagn Cytopathol 2018 46(5):425-28.10.1002/dc.2386529193907 [Google Scholar] [CrossRef] [PubMed]
[8]. Mandato VD, Sacchetti F, Costagliola L, La Sala GB, Primary tuberculosis of the uterine cervix: Keep it in mindJ Low Genit Tract Dis 2014 18(2):E29-33.10.1097/LGT.0b013e31829a557223994952 [Google Scholar] [CrossRef] [PubMed]
[9]. Sharma JB, Sharma E, Sharma S, Dharmendra S, Female genital tuberculosis: RevisitedIndian J Med Res 2018 148(Suppl):S71-83. [Google Scholar]