Case Report
A 53-year-old male presented to the OPD of Sreedhareeyam Ayurvedic Eye Hospital and Research Center, Koothattukulam, Kerala, India, with a one-month complaint of foggy vision and inability to see during the morning hours in his left eye (OS). He was apparently well before one month. When he experienced the symptoms one month ago, he took some allopathic medicine, which gave symptomatic relief. When he developed the same symptoms later on in the month, he Consulted at Sreedhareeyam and was prescribed Ayurvedic medicines.
The patient had diabetes, hypertension and hypothyroidism for 7 years, which were under control after the treatment. He was prescribed Metformin (1000 mg), Thyrox (75 mg), and Ecosprin for the same. His personal history showed normal appetite, sleep, and micturition, and constipated bowel. He was addicted to tobacco and alcohol.
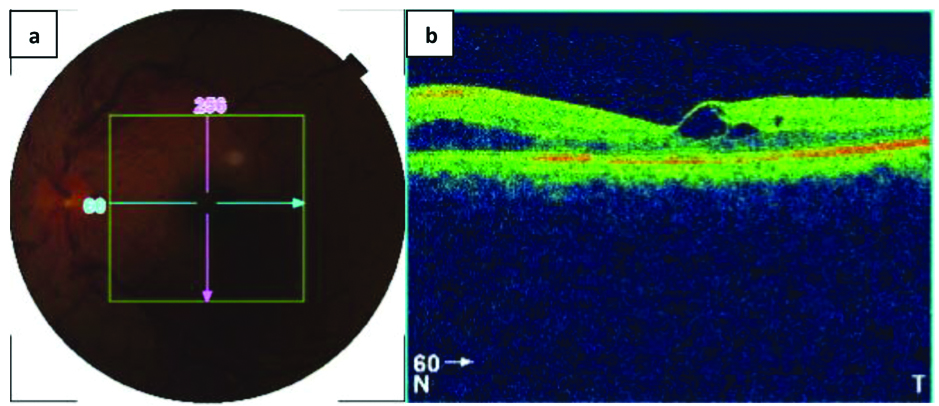
Unaided Distant Visual Acuity (DVA) was 6/60 Snellen (LogMAR 1) in both eyes (OU) and aided DVA was 6/6 Snellen (LogMAR 0) OU. Near Visual Acuity (NVA) was N12 in the right eye (OD) and N18 in the left eye (OS). Posterior segment examination OS on September 9th, 2018 showed tortuous blood vessels, haemorrhages, and cotton wool spots in the superior quadrant of the fundus [Table/Fig-1a]. Optical Coherence Tomography (OCT) scanning OS showed collection of fluid in the macular region. [Table/Fig-1b].
(a) Fundus photograph OS showing haemorrhages, tortuous blood vessels, and cotton-wool spots in the superior quadrant. (b) OCT scan OS showing oedema in the macular region.
A provisional diagnosis of central retinal vein occlusion was made based on the history, examination, and ancillary diagnosis. The disease Timira (blurring of vision), a Drishtigata Roga (disease of vision) according to Ayurveda, was explored for this patient based on his symptoms.
The patient was managed on an outpatient basis, with consultations on 09/09/2018, 24/09/2018, 10/12/2018, 01/04/2019, and 27/05/2019. Oral medicines Samirapancakam Kashaya*, optha Cap*, Bilvadi Gutika [1], and Chimiun Co. Tablet. A Lepa (paste) with Cyperus rotundus Linn. and Emblica officinalis Gaertn. was prescribed for application over the forehead [Table/Fig-2]. He was also advised strict rest.
| Medicine | Ingredients | Preparation | Dosage |
|---|
| Samirapancakam Kashaya* | Cyperus rotundus Linn., Hordeum vulgare Linn., Picorrhiza kurroa Royle ex. Benth, Santalum album Linn., Tinospora cordifolia Miers. | 1 part of the ingredients are boiled in 4 parts of water and reduced to 1/4. | 15 mL with 45 mL boiled and cooled water |
| Ophtha Cap* | Adathoda vasica Nees., Cyperus rotundus Linn., Azadirachta indica A. Juss., Tinospora cordifolia Miers., Picorrhiza kurroa Royle ex. Benth. | 1 part of all ingredients is powdered. This is then made into a capsule. | 1 tablet twice a day after food |
| Bilvadi Gutika [1] | Aegle marmelos Corr., Ocimum sanctum Linn., Pongamia pinnata Kerr., Cedrus deodara Linn., Terminalia chebula Retz., Terminalia bellerica Linn., Emblica officinalis Gaertn., Zingiber officinale Rosc., Piper nigrum Linn., Piper longum Linn., Cucurma longa Linn., Berberis aristata D. C., Cedrus deodara Linn. | 1 part of all ingredients is powdered. This is macerated with water and rolled into a pill. | 1 tablet twice a day before food |
| Chimium-Co | Rheum emodi Wall., Picorrhiza kurroa Royle ex. Benth., Cinnamomum zeylanicum Linn., KAl (SO4)2 | 1 part of all ingredients is powdered. This is macerated with water and made into a tablet. | 1 tablet twice a day after food |
| Lepa (paste) | Cyperus rotundus Linn., Emblica officinalis Gaertn. | 1 part of both ingredients is taken and powdered. This is mixed with water to obtain a paste. | External application over the forehead |
Ingredients for all medicines (except Chimium-Co Tablet) were obtained at Sreedhareeyam’s own herbal gardens, and the medicines were prepared at Sreedhareeyam Ayurvedic Medicines, Pvt. Ltd., the hospital’s GMP-certified drug manufacturing unit. Chimium-Co tablet was prepared by J&J Dechane Laboratories.
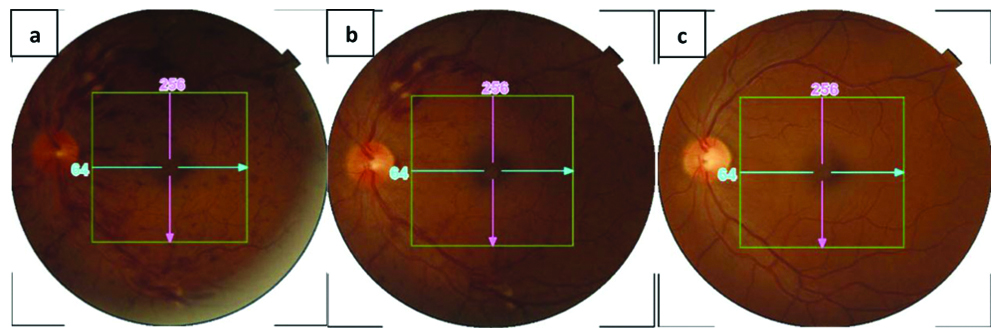
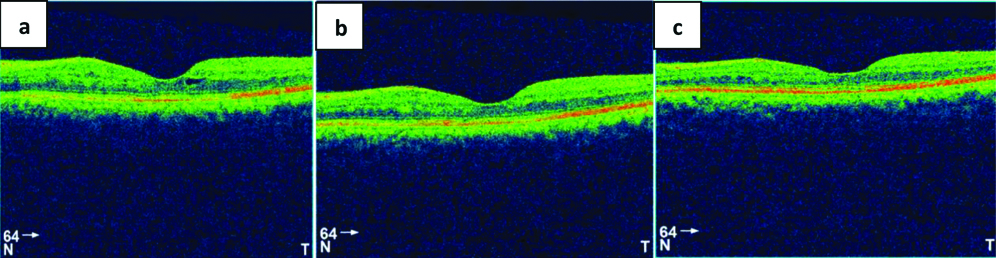
Assessment was done for both unaided and aided DVA, posterior segment examination, and OCT scanning. Unaided DVA improved to 6/36 Snellen (LogMAR 0.78) OU at the second OP consultation and was maintained for the subsequent visits. Fundus examination at each subsequent visit showed reduction in bleeding, tortuous blood vessels and cotton-wool spots [Table/Fig-3a-c]. OCT scanning at subsequent visits showed reduction in fluid accumulation and reappearance of the foveal contour [Table/Fig-4a-c].
Fundus examination OS (a) taken on 24/09/2018 and showing reduction in tortuous blood vessels and haemorrhages, (b) taken on 10/12/2018 and showing reduction in tortuous blood vessels, (c) taken on 27/05/2019 and showing complete resolution of haemorrhages, tortuous blood vessels, and cotton-wool spots.
OCT scanning OS (a) taken on 24/09/2018 and showing reduction in the fluid collection at the macula, (b) taken on 10/12/2018 and showing further reduction of fluid buildup, and (c) taken on 27/05/2019 and showing resolution of the macula.
This patient’s case is chronicled in a timeline of events [Table/Fig-5].
| Date | Event |
|---|
| 08/2018 | The patient first experiences fogginess of vision and inability to see in the morning hours. He is administered allopathic medicines, which provide symptomatic relief
|
| 09/09/2018 | Consults at Sreedhareeyam Eye Hospital.
|
| Visual Acuity (VA) | Posterior Segment | OCT | Medicines |
Unaided DVA: 6/60 Snellen (LogMAR 1) OU Aided DVA: 6/6 Snellen (LogMAR O) OU NVA: N12 OD, N18 OS
| Haemorrhages, tortuous blood vessels, and cotton-wool spots | Macular oedema | Samirapancakam Kashaya* Ophtha Cap* Bilvadi Gutika Lepa with Musta and Amalaki
|
| 24/09/2018 | Unaided DVA: 6/36 Snellen (LogMAR 0.78) OU Aided DVA: 6/6 Snellen (LogMAR O) OU NVA: N12 OD, N18 OS
| Reduction in haemorrhages and tortuous blood vessels | Reduction in macular oedema | Samirapancakam Kashaya* Cimium Co. Tablet Bilvadi Gutika Lepa with Musta and Amalaki
|
| 10/12/2018 | Unaided DVA: 6/36 Snellen (LogMAR 0.78) OU Aided DVA: 6/6 Snellen (LogMAR O) OU NVA: N12 OD, N18 OS
| Reduction in haemorrhages and tortuous blood vessels | Reduction in macular oedema | Samirapancakam Kashaya* Cimium Co. Tablet Bilvadi Gutika Lepa with Musta and Amalaki
|
| 01/04/2019 | Unaided DVA: 6/36 Snellen (LogMAR 0.78) OU Aided DVA: 6/6 Snellen (LogMAR O) OU NVA: N12 OD, N18 OS
| Reduction in tortuous blood vessels | Complete absorption of macular oedema | Samirapancakam Kashaya* Cimium Co. Tablet Bilvadi Gutika Lepa with Musta and Amalaki
|
| 27/05/2019 | Unaided DVA: 6/36 Snellen (LogMAR 0.78) OU Aided DVA: 6/6 Snellen (LogMAR O) OU NVA: N12 OD, N18 OS
| Complete resolution of haemorrhages, tortuous blood vessels, and cotton-wool spots | Reappearance of the foveal contour | Samirapancakam Kashaya* Cimium Co. Tablet Bilvadi Gutika Lepa with Musta and Amalaki
|
*Patented medicines of Sreedhareeyam Ayurvedic Eye Hospital and Research Center
Discussion
Central retinal vein occlusion, the second most common retinal pathology after diabetic retinopathy, is divided into ischaemic and non-ischaemic varieties. It is generally a unilateral disease, with the risk of developing vascular occlusion in the fellow eye at 1%. About 7% of persons may develop CRVO in the fellow eye after 5 years of onset in the first eye [2].
Etiological factors of CRVO include pressure on the central retinal vein by an atherosclerotic artery, diabetes mellitus, hypertension, and orbital tomours. Macular oedema is the most common cause of defective vision in CRVO [3].
Patients with ischaemic CRVO are usually past middle age and present with decreased VA, usually ranging between 6/60 to hand movements, especially upon waking up in the morning. A marked relative afferent pupillary defect is also present. Ophthalmoscopy shows extensive haemorrhages involving the periphery and the posterior pole, optic disc oedema, marked tortuosity and engorgement of the retinal veins, cotton wool spots and frequent macular oedema. The site of occlusion is at or near the retrolaminar region of the fundus. 60% of patients develop anterior segment neovascularization and neovascular glaucoma [4].
Non-ischaemic CRVO is characterised by mild-to-moderate loss of VA, which may be due to macular haemorrhage or oedema. Afferent pupillary defects are mild if present. Fundus examination reveals dot and flame-shaped retinal haemorrhages, optic disc swelling, tortuous and engorged retinal veins and a few cotton-wool spots. Many of the findings resolve completely. The optic disc may return to its normal appearance or have the presence of optico-ciliary shunts. Macular oedema can also resolve completely, although persistent cystoid macular oedema may be permanent [5].
A study conducted identified several systemic risk factors for CRVO, which included separately-diagnosed hypertension and diabetes mellitus [6]. A descriptive study conducted on 65 patients with diagnosed RVO showed that 34% of the patients had hypertension, while 23% had diabetes [7]. Other probable systemic risk factors include cardiovascular diseases, carotid insufficiency, systemic lupus erythematosus, and thrombolytic/bleeding disorders [8].
The pathogenesis of CRVO is believed to adhere to Virchow’s triad of stasis, vascular damage, and hyper-coagulation. A thrombus at or posterior to the lamina cribrosa, the sieve-like structure at the posterior-most aspect of the sclera through which fibres of the optic nerve pass, is believed to occlude the central retinal vein. Hematological factors including raised erythrocyte sedimentation rate and increased levels of hematocrit, homocysteine, fibrinogen, and blood viscosity have been postulated as a pathogenic factor, but their role in the pathogenesis of CRVO and whether they themselves can initiate occlusion remains obscure. Another theory postulates that primary factors such as inflammatory orbital or optic nerve problems, structural anomalies in the lamina cribrosa, and hemodynamic changes induce the end-stage phenomenon of thrombosis [9]. Arteriosclerosis of the central retinal artery and endothelial cell damage has also been postulated as a possible factor of pathogenesis.
Timira, considered as a dreadful disease according to Acarya Susruta [10], encompasses symptoms that range from Avyakta Rupa (indistinct vision) to Andha (blindness). It warrants immediate management to prevent progression into Kacha (diminished vision) and Linganasa (complete blindness) [11].
As the condition is a vascular pathology, the role of RaktaDhatu (blood) in the Samprapti (pathogenesis) was also explored. Indulgence in diets and activities that are harmful for the eye caused Pitta (bile) and Kapha (phlegm) to vitiate. Rakta got vitiated along with Pitta because of the above factor and the fact that Rakta and Pitta share a homologous relationship with each other (Asraya-Asrayi Bhava).
Mandagni (impaired digestion) and increased Doshas resulted in compromised nutrition to the eye due to Sanga (obstruction) and Vimarga Gamana (pathological diversion of flow) of the Raktavaha Srotas (channels transporting blood). Cotton-wool spots, a direct result of hypoxia due to compromised nutrition that causes infarction of the tissue, is caused by Sanga. Oedema and tortuous blood vessels are due to Sanga and Vimarga Gamana, in the fact that the blood vessels become pathologically affected and leak serum into the retina.
In light of the above factors and the fact that available modes of management in modern medicine may not always prove effective, exploration to find an effective Ayurvedic protocol to treat CRVO is warranted. Two case studies of management of CRVO using Ayurvedic therapies were analysed. Both of them utilised Pancakarma (purificatory therapy), oral medicines, and Kriyakalpa (local ocular therapies). One case showed improvement in DVA from counting fingers (CF+ve) to 6/18 Snellen (LogMAR 0.477) OD and 6/9 Snellen (LogMAR 0.17) to 6/6 Snellen (LogMAR 0) OS; NVA improvement from N60 to N6 OD and maintenance of N6 before and after treatment OS; and reduction in flame-shaped haemorrhages and macular oedema on fundus examination OD [12]. The other case showed improvement in DVA from 6/36 Snellen (LogMAR 0.778) to 6/12 Snellen (LogMAR 0.3) OS and 6/12 Snellen (LogMAR 0.3) to 6/6 Snellen (LogMAR O) OD. Fundus examination showed reduction of tortuous blood vessels and flame-shaped haemorrhages [13].
The ingredients of Bilvadi Gutika possess the properties of Vata-Kapha Samaka (pacifiers of Vata (wind) and Kapha (phlegm)), Stambhaka (inducing hemostasis), Dipana (carminative), Pacana (digestive), and Rakta Sodhaka (purifying blood). With antioxidant, analgesic, anti-inflammatory, cardio-protective, wound-healing, and neuro-protective properties, the ingredients of Bilvadi Gutika aid digestion, resolve infarction, absorb excess fluid, and restore vasculature and circulation to the target tissue [14].
Cyperus rotundus Linn. possesses anti-inflammatory, anti-pyretic, anti-bacterial, hemodynamic and anti-hemorrhagic properties. It improves all hemorrheological indices such as plasma viscosity and erythrocyte electrophoresis. A blood-stagnating model built with adrenaline and cold stimulation showed characteristics of increased viscosity, thickness and liability to coagulate [15]. Alcohol extracts produced gradual and persistent fall in blood pressure and increased respiratory stimulation. With these properties, it prevented haemorrhages and further vascular pathology in the retina, bringing the retinal blood vessels back to normal. Emblica officinalis Gaertn. showed anti-inflammatory, cytotoxic, wound-healing, anti-oxidant, anti-diabetic and hypoglycemic activities [16]. These helped to prevent further pathology and induce healing in the retina.
Application of paste to the forehead allowed the essential elements to be absorbed through the skin and thus bypass barriers such as blood-brain barrier and blood-retinal barrier. Topical applications inhibit metabolism of the drugs by the liver, thus increasing their bio-availability and providing its effects directly to the site of action [17]. The molecules of the drug exert their pharmacologic action after absorption through the stratum corneum into the epidermis and dermis.
Samirapancakam Kashaya is indicated in Raktaja (blood-related) and Pittaja (Pitta-related) disorders. Ophtha Cap is indicated in disorders of the eye. Some of their key ingredients, viz., Tinospora cordifolia Miers., Terminalia chebula Retz., Terminalia bellerica Linn., Emblica officinalis Gaertn., Azadirachta indica A. Juss., Adathoda vasica Nees., and Santalum album Linn., have cooling properties, hence they manage both Pitta and Rakta. They also have the property of purifying blood and promoting vision.
Chinium-Co is made from Rheum emodi Wall., Picorrhiza kurroa Royle ex. Benth., Ouercus infectoria Oliv., Cinnamomum zeylanicum Linn., Digitalis purpurea Linn., and alum (KAl(SO4)2). The ingredients are potent hemostats, and the medicine is indicated in all bleeding and vascular disorders.
The most challenging aspect of managing CRVO is restoration of vision, but it was improved to an extent and vigilantly maintained in this case. The medicines were able to bring the fundus and OCT scanning to near-normal findings by correcting digestion, passage of Srotas, and absorbing subretinal fluid. Hence, the approach for normalising physiology while treating the condition can make an Ayurvedic protocol a suitable option for management of CRVO. The results obtained from this study may be validated using large-scale sample trials.
Conclusion
The key aspects of this case were the timely consultation of the patient and the mode of action of the medicines. Visual acuity improved at the 2nd consultation and was maintained through the subsequent consultations, and the fundus and Optical coherence tomography scanning substantially improved by the end of the last consultation.
*Patented medicines of Sreedhareeyam Ayurvedic Eye Hospital and Research Center
[1]. Murthy KR, Srikantha, AshtangaHrdaya of Vagbhata: Text, English Translation, Notes, Appendices, and Index, Vol. 3: UttaraSthana 1994 VaranasiKrishnadas Academy:357 [Google Scholar]
[2]. Hayreh SS, Zimmerman MR, Podhajsky P, Incidence of various types of retinal vein occlusion and their recurrence and demographic characteristicsAm J Ophthalmol 1994 117(4):429-41.10.1016/S0002-9394(14)70001-7 [Google Scholar] [CrossRef]
[3]. Yanoff M, Duker J, Ophthalmology: 3rdEdition, 2009 Philadelphia, PennsylvaniaMosby, an Imprint of Elsevier, Inc.:599 [Google Scholar]
[4]. Agarwal S, Agarwal A, Apple DJ, Buratto L, Alió J L, Pandey SK, Textbook of Ophthalmology 2002 Vol. 4New DelhiJaypee Brothers Medical Publishers, Pvt. Ltd.:2532-33.10.5005/jp/books/10931 [Google Scholar] [CrossRef]
[5]. Yanoff M, Duker J, Ophthalmology: 3rd Edition 2009 Philadelphia, PennsylvaniaMosby, an Imprint of Elsevier, Inc.:597 [Google Scholar]
[6]. Kolar P, Risk factors for central and branch retinal vein occlusion: A meta-analysis of published clinical dataJournal of Ophthalmology, Hindawi Publishing Corporation 2014 :01-05.10.1155/2014/72478025009743 [Google Scholar] [CrossRef] [PubMed]
[7]. Rekha P S, Padmavathi P, Nova S, Vaikkakara S, Study on clinical profile of patients with retinal vein occlusionJournal of Evolution of Medical and Dental Sciences 2017 51(6):3885-89.10.14260/Jemds/2017/840 [Google Scholar] [CrossRef]
[8]. Maharana PK, Sharma N, Kumar A, Ophthalmology Clinics for Postgraduates 2017 New DelhiJaypee Brothers Medical Publishers (P) Ltd.:216 [Google Scholar]
[9]. Pichi F, Linn JI, Tripathy K, Shah VA, Central Retinal Vein Occlusion, American Academy of Ophthalmologyhttps://eyewiki.aao.org/Central_Retinal_Vein_Occlusion [Google Scholar]
[10]. Sharma P V, SusrutaSamhita: Text with English Translation and Dalhana’s Commentary along with Critical Notes, Vol. III: Kalpasthana and Uttaratantra, 2005 VaranasiChaukhambhaVishwabharati:108 [Google Scholar]
[11]. Murthy KR, Srikantha, AshtangaHrdaya of Vagbhata: Text, English Translation, Notes, Appendices, and Index, Vol. 3: UttaraSthana 1994 VaranasiKrishnadas Academy:113 [Google Scholar]
[12]. Gupta SP, Vaghela DB, Kumar S, Management of central retinal vein occlusion through ayurveda: A case studyInternational Journal of Health Sciences and Research 2019 9(5):448-52. [Google Scholar]
[13]. Majagaiyan P, MJ Aswini, Management of central retinal vein occlusion through kriyakalpa procedures- A case reportInternational Ayurvedic Medical Journal 2018 6(9):2238-42. [Google Scholar]
[14]. Shubha PU, Honwad VS, Ballal SR, A Review on Bilvadi GutikaInternational Ayurvedic Medical Journal 2017 (5):501-06. [Google Scholar]
[15]. Singh N, Pandey BR, Verma P, Bhalla M, Gilca M, Phyto-pharmacotherapeutics of Cyperusrotundus Linn (Motha): An overviewIndian Journal of Natural Products and Resources 2012 3-4:467-76. [Google Scholar]
[16]. Hasan R, Islam N, Islam R, Phytochemistry, pharmacological activities and traditional uses of Emblicaofficinalis: A reviewInternational Current Pharmaceutical Journal 2016 5(2):14-21.10.3329/icpj.v5i2.26441 [Google Scholar] [CrossRef]
[17]. Mehar M, Chavhan KR, Suryawanshi SS, A review article on LepaKalpana and VishaghnaLepa in Different bite conditionsInternational Ayurvedic Medical Journal 2017 5(4):1279-86. [Google Scholar]