Different types of glandular lesions may be seen in the urinary bladder and they pose a significant diagnostic dilemma as these lesions range from entirely benign to aggressive malignant tumours. The lesions with no premalignant potential may include various proliferative and reactive processes such as cystitis cystica and cystitis glandularis [1]. Cystitis cystica and cystitis glandularis are chronic inflammatory disorders with slight male predominance [2]. Occasionally, these lesions can be confused with infiltrative neoplasms. Rarely, Mullerian tissue may be seen in the urinary bladder and one needs to be careful while differentiating from the true glandular neoplasms.
There is variety of morphological variants available with varying degree of glandular differentiation that may lead to the development of adenocarcinoma. Confirmed diagnosis of primary adenocarcinoma of the bladder from other urothelial carcinomas may be difficult due to glandular differentiation; however, recognition of glandular lesions is important as the treatment of each type of lesion may vary.
Histological differentiation of these lesions is vital for pathologists as well as clinicians because they may affect prognostic consequences, may need different modalities compared to conventional ones and may aid to avoid diagnostic misinterpretations [3]. A recent Indian study by Singh JP et al., highlighted the use of different treatment modalities (TURBT and radical cystectomy) in patients with bladder tumours [4]. As there are limited Indian literature related to the diagnosis and management of patients with glandular lesions of the bladder, the present study was aimed to report our experience of diagnosis, management and follow-up of patients with glandular lesions of the bladder.
Materials and Methods
This was a retro-prospective study of 16 consecutive patients with urinary bladder glandular lesions who were hospitalised at the MS Ramaiah Medical College and Hospital, Bangalore, Karnataka, India, from October 2009 to March 2013. The data were obtained from hospital records and records from the Department of Pathology. The study was conducted in accordance with the approved protocol and ethical principles that have their origin in the Declaration of Helsinki. Each patient provided written informed consent for participation in the study.
The demographic (age, gender, residence) and clinical characteristics including symptoms, physical signs, site of lesion, urine cytology, cystoscopy, imaging, treatment were noted. All patients underwent routine preoperative examination followed by cystoscopy and proceed under anaesthesia. The preoperative examination included routine blood and urine tests, renal function tests, electrolytes and coagulation profile.
These patients underwent urine cytology, ultrasonography and Contrast-Enhanced Computed Tomography (CECT) of Kidney Ureter and Bladder (KUB) region. All patients underwent cystoscopy with biopsy of the lesion or TURBT and histopathological examination of the resected specimen. These patients were followed-up for 6-34 months after surgery with ultrasonography, urine cytology and cystoscopy to look for any recurrence of tumour and if resected, to know the type of histology. Ultrasonography was done to know the recurrence of the tumour. Urine cytology was performed on the centrifuged sample to identify the malignant cells in the urine. Cystoscopy was done to know the recurrence of disease or appearance of any new lesion. Re-resection of tumour with histopathological examination was done for recurrent growths.
Statistical Analysis
The data were collected and analysed, presented as number and percentage.
Results
A total of 16 patients were enrolled in this study who were admitted from October 2009 to March 2013 who were diagnosed with glandular lesions of the urinary bladder. The median (range) age was 34 (17-48) years and a total of 11 (68.7%) patients were females [Table/Fig-1]. The most common symptoms were dysuria, frequency, and nocturia (n=12, 75% each) followed by suprapubic pain and difficulty in voiding (n=10, 62.5% each), intermittent urination, hematuria, hesitancy and sensation of incomplete voiding (n=8, 50.0% each) [Table/Fig-1].
Demographic and clinical characteristics.
| Parameter | N=16 |
|---|
| Age (years), median (range) | 34 (17-48) |
| Gender |
| Male | 5 (31.2) |
| Female | 11 (68.7) |
| Residence |
| Urban | 12 (75.0) |
| Rural | 4 (25.0) |
| Clinical symptoms |
| Dysuria | 12 (75.0) |
| Frequency | 12 (75.0) |
| Nocturia | 12 (75.0) |
| Suprapubic pain | 10 (62.5) |
| Difficulty in voiding | 10 (62.5) |
| Intermittent urination | 8 (50.0) |
| Hematuria | 8 (50.0) |
| Hesitancy | 8 (50.0) |
| Sensation of incomplete voiding | 8 (50.0) |
| Flank pain | 4 (25.0) |
| Fever | 3 (18.8) |
Data presented as n (%), unless otherwise specified
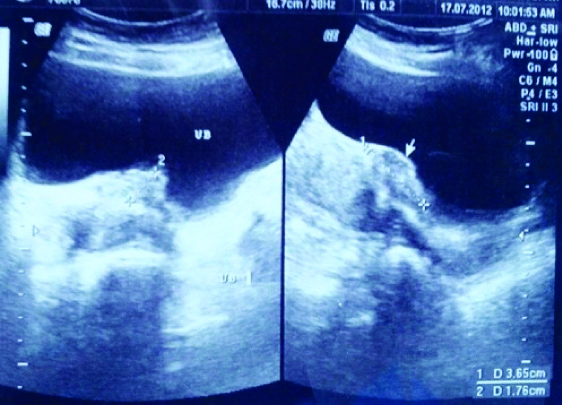
Preoperative USG [Table/Fig-2] was done in all 16 cases and was diagnostic in 12 cases (75.0%). Computed tomography was carried out in nine cases, which identified the lesions in eight cases (88.9%). None of these nine cases showed positivity for urine cytology. The most common site of the tumor was at the trigone in 11 patients followed by lateral wall in four patients and dome in one patient. The most common type of macroscopic appearance of the lesion was papillary in 11 patients followed by polypoidal in three patients and flat lesions in two patients. Seven patients had tumor sizes ranging from 3-5 cm followed by six patients with tumor sizes of 1-3 cm. Only one case had a large tumor measuring more than 5 cm in size [Table/Fig-3].
Ultrasound image demonstrating a lesion in the bladder which was later demonstrated to be a glandular lesion.
Summary of cystoscopic findings at surgery (n=16).
| Parameter | N=16 |
|---|
| Location of tumours |
| Trigone | 11 (68.8) |
| Lateral wall | 4 (25.0) |
| Dome | 1 (6.3) |
| Type of lesion |
| Papillary | 11 (68.8) |
| Polypoidal | 3 (18.8) |
| Flat | 2 (12.5) |
| Size of lesion |
| <1 cm | 2 (12.5) |
| 1-3 cm | 6 (37.5) |
| 3-5 cm | 7 (43.8) |
| >5 cm | 1 (6.3) |
Data presented as n (%)
In the study, 14 (87.5%) patients underwent TURBT for the bladder tumour. One patient (7.1%) post TURBT developed bleeding, which was treated conservatively with irrigation and blood transfusions. Two patients (14.3%) who underwent TURBT developed recurrence of tumour after 1.5 and 2 years, respectively. Bladder biopsy was done in two cases (12.5%) where there were flat lesions and one of these patients developed recurrence of the lesion after nine months.
[Table/Fig-4] summarises the histopathological findings. The most common abnormality seen was a combination of cystitis cystica with cystitis glandularis in five (31.3%) patients followed by cystitis glandularis in four (25.0%) patients. Three patients had a combination of cystitis glandularis with intestinal metaplasia, two patients had cystitis cystica and one patient each had florid intestinal metaplasia and polypoidal cystitis.
Summary of histopathological findings (n=16).
| Types | n (%) |
|---|
| Cystitis cystica | 2 (12.5) |
| Cystitis glandularis | 4 (25.0) |
| Cystitis cystica with cystitis glandularis | 5 (31.3) |
| Cystitis glandularis with intestinal metaplasia | 3 (18.7) |
| Intestinal metaplasia | 1 (6.3) |
| Polypoidal cystitis | 1 (6.3) |
Discussion
This retro-prospective study experience of diagnosis, management and follow-up of patients with glandular lesions of the bladder is in a real-world setting. Though the sample size was small, the study provides important information on the prognosis of patients with glandular lesions of the bladder and adds significant information to the literature.
Urinary bladder lesions may have various benign proliferating processes. These lesions are thought to be the outcome of irritation to urothelium. Sometimes these proliferative processes characterise true heterotopia such as endometriosis which is composed of readily identifiable endometrial glands and stroma. However, to determine the origin of the lesion cytological features or a superficial biopsy specimen could be necessary [1]. Glandular lesions of the bladder are difficult to diagnose clinically as they have subtle clinical manifestations and for the rarity of the lesion.
In the present study, among 16 patients with glandular lesions of the bladder, the most common symptom was dysuria, frequency and nocturia in 12 patients each, followed suprapubic pain and difficulty in voiding in 10 patients each. Haematuria was seen in eight patients and fever in three patients. Lower urinary tract symptoms were the main feature in these patients. These symptoms were non-specific and hence diagnosis of the glandular lesion was often overlooked. Although glandular lesions of the urinary bladder have a relatively low incidence, delay in diagnosis may possibly have a major health consequence.
Radiological imaging techniques including USG or CT scan have a major role in the diagnosis of the bladder lesions and urine cytology helps to rule out or to confirm the possibility of malignant bladder tumour. In the present study, the diagnostic accuracy of CT scan was slightly higher (88.9%) than the B-mode ultrasound (75%) which suggests that radiological diagnostic findings corroborate the histopathological findings. B-mode ultrasound is accepted as the initial diagnostic tool for the bladder lesion. However, we found that ultrasound and CT had almost similar diagnostic accuracy. The advantages of ultrasound are that it is simple, inexpensive and provides instant results. However, CT scan also has several advantages for the diagnosis of bladder lesion {e.g., flat lesions (in contrast-enhanced mode) are better visualised}.
Trigone was the most common site of involvement (68.8%) by glandular lesions in bladder followed by the lateral wall. Papillary lesions were the most common macroscopic type of lesions followed by polypoidal lesions. The size of the glandular lesions may vary from a few millimeters to more than 5 centimeters in size. In the present study, the majority of the tumours were in the range of 1-5 cm (81.2%) with the exception of three cases where the lesion was either less than 1 cm or more than 5 cm in size. The most common pathological finding seen in our series was concomitant cystitis cystica with cystitis glandularis in five patients followed by cystitis glandularis. Concomitant cystitis glandularis with intestinal metaplasia was seen in three patients, cystitis cystica in two patients.
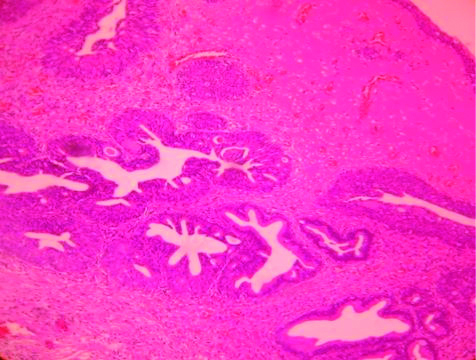
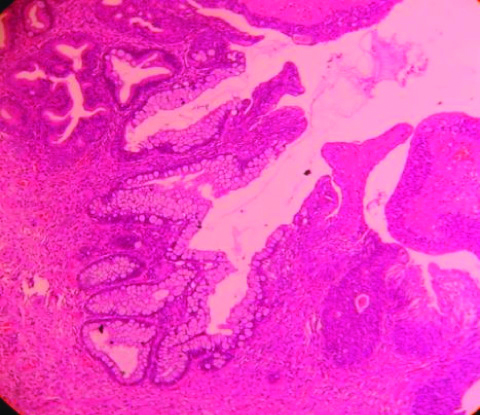
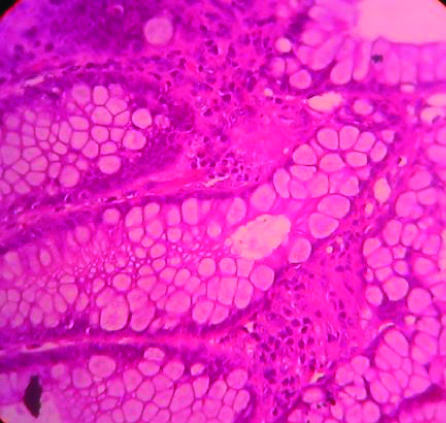
There are different variants of benign glandular lesions of bladder including cystitis cystica, cystitis glandularis and intestinal metaplasia. Von Brunn’s nests are well defined nests of urothelial cells which encompasses the lamina propria. These nests generally seem to be separated from the overlying epithelium and show central cystic degeneration resulting in gland-like lesion known as cystitis cystica [Table/Fig-5]. Cystitis cystica can be visible cystoscopically and may look like translucent submucosal cysts containing clear fluid [5]. A study by Volmar KE et al., evaluated Ki 67 (MIB-1), p53, p27 and CK 20 as a possible immunohistochemical marker, which could differentiate florid Von Brunn’s nests from nested urothelial carcinoma; however, these were not very useful [5]. Cystitis glandularis is an apical glandular differentiation along with the central cystic degeneration in cystitis cystica and also characterised by a central lining of cuboidal or columnar cells surrounded by layers of urothelial cells [Table/Fig-6] [6]. Owing to chronic inflammation or irritation to urothelial lining it leads to metaplastic alteration. There is an evidence that recurrent urinary tract infection, chronic bladder outlet obstruction, neurogenic bladder, calculi and indwelling catheters may be associated with the cystitis glandularis [7,8]. Intestinal metaplasia is composed of glandular proliferation within the lamina propria similar to typical cystitis glandularis. The intestinal metaplasia nests contain abundant mucin-secreting goblet cells [Table/Fig-7]. These lesions may have positive immunohistochemistry staining with CDX2 and CK20 coupled with the absence of staining for CK7 [6]. In a study by Morton MJ et al., authors found an association between bladder intestinal metaplasia and telomere shortening relative to adjacent normal urothelial cells. Additionally, telomere shortening was also seen in urothelial carcinomas [9].
Cystitis cytica with central cystic degeneration and Von Brunn’s nests extending into the lamina propria (H&E stain, High power view).
Cystitis glandularis with Von Brunn’s nests demonstrating apical glandular differentiation and cystitis cystica (H&E stain, High power view).
Intestinal metaplasia with glandular proliferation within the lamina propria with abundant mucin-secreting goblet cells (H&E stain, High power view).
In a retrospective review of 89 patients with intestinal metaplasia, the majority of intestinal metaplasia were located on or near the trigone (n=67) [10]. In another study, telomerase reverse transcriptase promoter mutations were found to be helpful in distinguishing urothelial carcinoma with glandular differentiation from other bladder glandular lesions [11].
Limitation
Authors acknowledge the following limitations of the study. First, the study was retro-prospective which may have an inherent selection bias. Second, the study was conducted at a single center, and third, the sample size was very low; hence, caution must be taken when generalising these results.
Conclusion
This report suggests that a combination of various investigation modalities with a high index of suspicion is required in establishing the diagnosis. The accurate diagnosis could be established after histopathological examination of the resected specimen or bladder biopsy. Considering the risk of progression from cystitis glandularis or intestinal metaplasia to adenocarcinoma annual cystoscopy and bladder biopsy can be recommended. Studies with large sample size and longer duration of follow-up are warranted to assess the true malignant potential of the benign glandular lesions of the bladder.
Data presented as n (%), unless otherwise specified
Data presented as n (%)