Vaginal Rhabdomyoma: A Rare Occurrence
Varsha Shree Rajanna1, Kalyani Raju2, Gomathi Ethiraj3, Hajra Khursheed Mehdi4
1 Resident, Department of Pathology, Sri Devaraj URS Medical College, Sri Devaraj Urs Academy of Higher Education and Research, Kolar, Karnataka, India.
2 Professor and Head, Department of Pathology, Sri Devaraj Urs Medical College, SRI Devaraj Urs Academy of Higher Education and Research, Kolar, Karnataka, India.
3 Professor, Department of Obstetrics and Gynaecology, Sri Devaraj URS Medical College, Sri Devaraj Urs Academy of Higher Education and Research, Kolar, Karnataka, India.
4 Resident, Department of Pathology, Sri Devaraj URS Medical College, Sri Devaraj URS Academy of Higher Education and Research, Kolar, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kalyani Raju, Professor and Head, Department of Pathology, Sri Devaraj Urs Medical College, SRI Devaraj Urs Academy of Higher Education and Research, Kolar, Karnataka, India.
E-mail: drkalyanir@rediffmail.com
Rhabdomyomas represent ≤2% of all striated muscle tumours. Among the extracardiac subtypes, genital rhabdomyoma is most uncommon. The vaginal type commonly presents as a polypoidal mass. Benign and malignant mimickers should be differentiated from vaginal type of genital rhabdomyoma for appropriate treatment. Here, the present authors report a case of a 48-year-old nulliparous woman who presented with the history of bleeding per vagina. Clinical examination revealed pedunculated polyp in anterior vaginal wall. Followed by, histopathological examination confirmed diagnosis of vaginal rhabdomyomas.
Female genital tract, Striated muscle tumour, Soft tissue tumour
Case Report
A 48-year-old nulliparous woman presented with a history of bleeding per vagina and was not associated with urinary or gastrointestinal symptoms. Medical history revealed hysterectomy 20 years back. Personal and family history was not significant. Per speculum examination showed features of vascular polyp measuring 4 cm×3 cm. Per-vagina examination showed features of pedunculated polyp measuring 4 cm×3 cm, arising from middle third of anterior vaginal wall. A clinical diagnosis of vaginal polyp was offered with a differential diagnosis of squamous papilloma and vaginal rhabdomyoma.
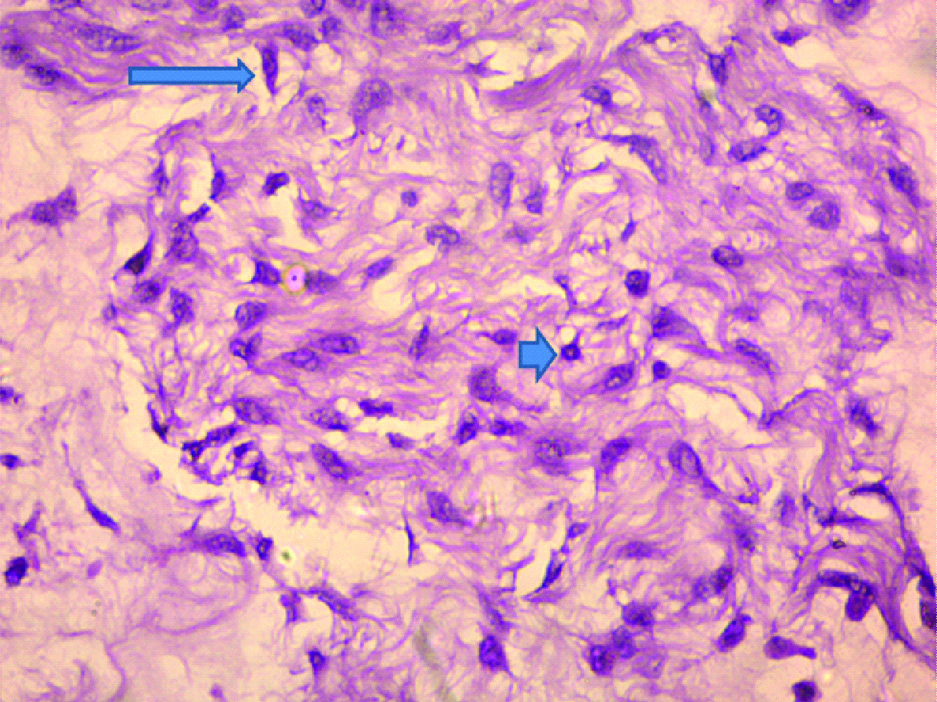
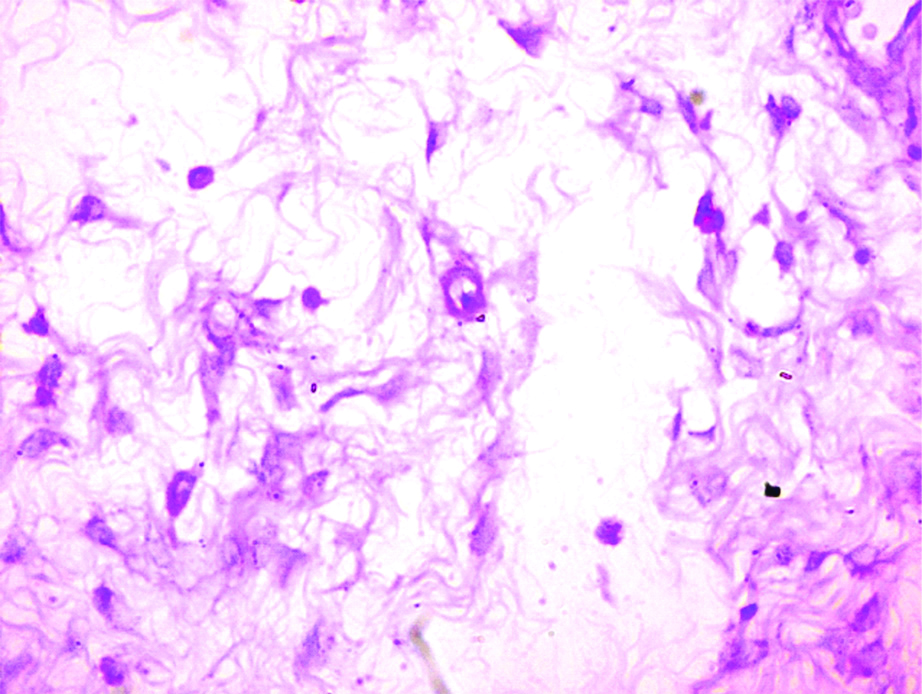
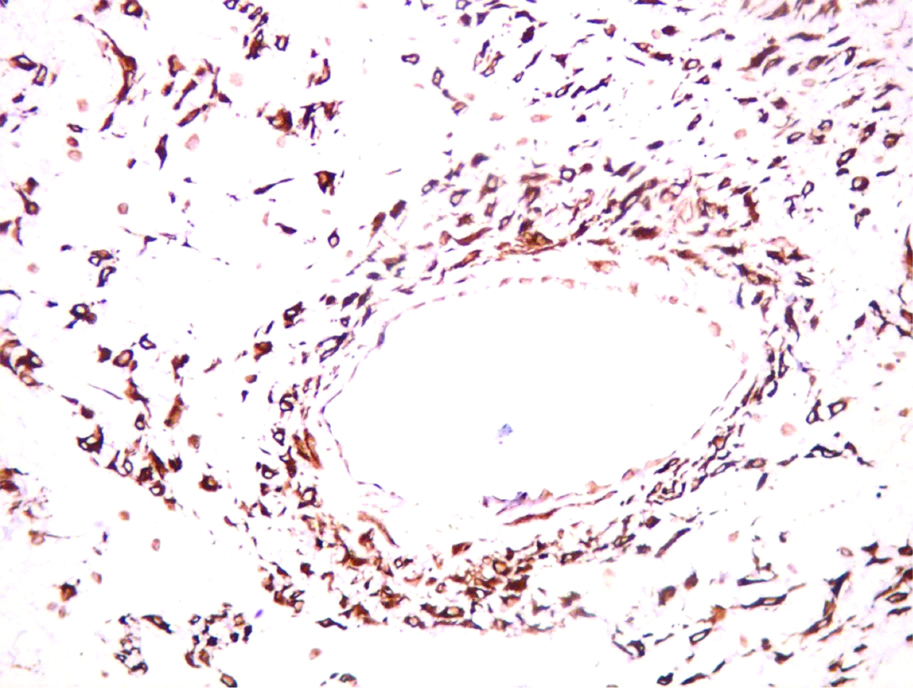
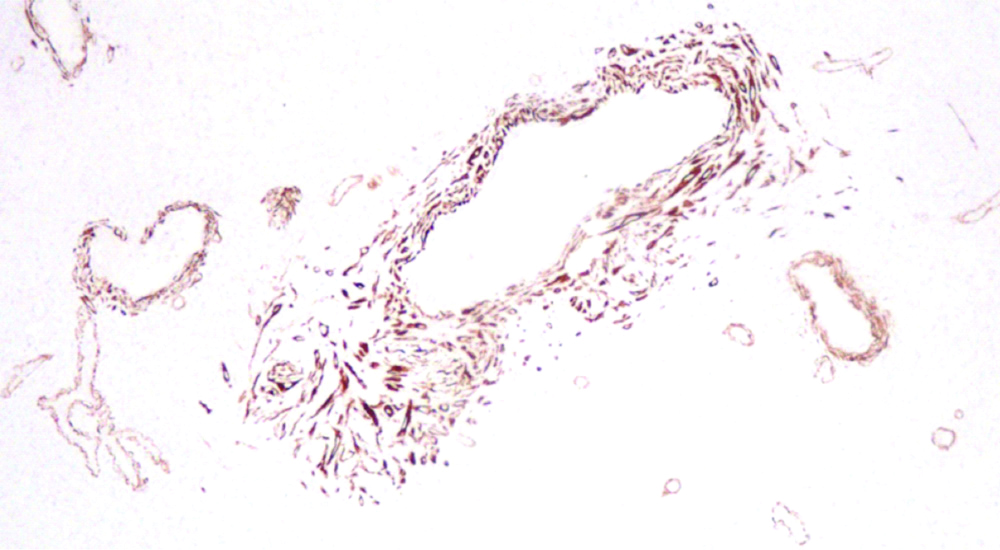
Local excision was done and subjected to histopathological examination. The specimen consisted of grey-white soft tissue mass measuring 3 cm×3 cm. Cut section was grey-white [Table/Fig-1]. Microscopy showed stratified squamous epithelium with focal ulceration and granulation tissue. Subepithelial stroma showed strap cells and spider cells with elongated and bland nucleus in a myxoid background. Some round-to-oval cells with definite cytoplasmic border, dark eosinophilic cytoplasm and hyperchromatic nuclei were seen [Table/Fig-2]. However cellular atypia and mitotic activity were absent. Sections stained with PAS showed cytoplasmic positivity of tumour cells indicating presence of glycogen [Table/Fig-3]. Immunohistochemistry (IHC) showed strong positivity for desmin in the tumour cells which demonstrates striations and confirm the diagnosis of rhabdomyoma [Table/Fig-4]. IHC for Smooth Muscle Actin (SMA) showed focal positivity of tumour cells. SMA demonstrates actin filaments of muscle tissue [Table/Fig-5]. Based on histopathological features and IHC markers a diagnosis of vaginal rhabdomyoma was given. Follow-up of the patient for 3-months was uneventful.
Gross photograph shows gray white mucosa covered tumour.

Microphotograph shows tumour tissue consisting of strap cells [Long arrow], spider cells [Short arrow] and myxoid stroma. (H&E X400).
Microphotograph shows tumour cells with PAS positive cytoplasm indicating the presence of glycogen. (PAS X400).
Microphotograph shows diffuse positivity of Desmin in tumour cells demonstrating striations.(Desmin X400).
Microphotograph showing focal positivity of smooth muscle actin demonstrates the actin filaments in tumour cells (SMA X100).
Discussion
Rhabdomyoma is a benign neoplasm showing well-formed skeletal muscle differentiation [1]. It represents ≤2% of all striated muscle tumours [2]. These are classified into cardiac and extracardiac type. The extracardiac type is further subdivided into adult, fetal and genital rhabdomyoma [1]. Of these, genital rhabdomyoma is an extremely rare neoplasm. There are <30 cases reported in the literature [2]. The vaginal rhabdomyomas have to be distinguished from other mimickers by clinical presentation and histological features.
Mostly, rhabdomyoma involves head and neck regions. The cardiac rhabdomyoma presents most commonly in paediatric age group and is seen in both males and females [3]. While among the extracardiac rhabdomyoma, adult type occurs usually in males of middle age group. The fetal type presents in males from birth to age of 3 years. And genital type is observed in young and middle aged women [4]. In the literature, 14 cases of adult head and neck rhabdomyoma are reported. Less than 30 cases of vaginal rhabdomyoma are reported by the time of writing this case report [5].
Patients with cardiac rhabdomyoma present with shortness of breath and have heart murmurs. Most cases are associated with tuberous sclerosis and they present as cerebral palsy features. Patients with adult type present with a round or polypoid mass in the region of neck, while fetal type of rhabdomyoma present as subcutaneous masses in head and neck region [5].
Genital rhabdomyoma present as a polypoidal mass and most of the patients are asymptomatic who are diagnosed incidentally on routine examination. In some cases, patient presents with dyspareunia or vaginal bleeding [6]. The diagnosis is purely made by histopathological features which shows strap like cells in a myxoid background. Cells also show abundant eosinophilic cytoplasm with glycogen and cross-striation. Cellular atypia or mitotic activity is not seen. Special stains like PAS, Masson trichrome and PTAH are done which highlights cross-striations [1]. IHC markers which show positivity are Desmin, myoglobin and specific muscle actin which are done for confirmation and to differentiate it from other vaginal polyps. Keratin, CD 68, S100 stains are negative in these cases [5]. In the present case, the patient presented with vaginal bleeding and polypoidal mass. PAS stain showed cytoplasmic positivity of tumour cells. IHC markers desmin and SMA showed positive in tumour cells. The [Table/Fig-6] shows the cases reported in various studies and in the present study.
Shows the Cases reported in various studies and in present study.
| Author | Site | No. of cases | Age of patient | Follow-up |
|---|
| Attafi S et al., [2] | Vagina | 1 | 24 years | - |
| Patrelli TS et al., [4] | Vagina | 1 | 38 years | - |
| Schoolmeester JK et al., [6] | 9 cases-vagina3 cases-cervix | 12 | 43-65 years | 7 cases- no recurrence2 cases- recent3 cases- lost for follow-up |
| Losi L et al., [7] | Vagina-recurrence | 1 | 49 years | Recurrence after 4 yrs |
| Andrade NN et al., [8] | Extracardiac-tongue | 1 | 11 years | No recurrence upto 2 years of follow-up |
| Present case | Vagina | 1 | 48 years | Followed-up for 3 months, uneventful |
The differential diagnosis includes benign vaginal polyps and botryoid embryonal Rhabdomyosarcoma (RMS) [1,2]. Benign vaginal polyp does not show the classic strap cells with striations which are seen in vaginal rhabdomyoma. Unlike genital rhabdomyoma, botryoid embryonal RMS is a rapidly growing lesion that occurs in young children. The subepithelial cambium layer is characteristic of botryoid embryonal RMS. Also, nuclear pleomorphism and mitotic figures are prominent in RMS [7]. In the present case, the differential diagnosis was not entertained.
The overall prognosis of patients with rhabdomyoma after surgery (local excision) is fair to good depending on the part of body involved. The cardiac rhabdomyoma has highest risk. Overall the vaginal rhabdomyoma has a benign behaviour and complete excision is curative. The recurrence rate is very low [7]. In the present case follow-up of the patient for 3 months was uneventful.
Conclusion
Genital rhabdomyoma in general and vaginal rhabdomyoma specifically is an extremely rare neoplasm. This entity should be known to both reporting pathologist and treating gynaecologist for timely diagnosis and the knowledge of recurrences.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jul 17, 2019
Manual Googling: Sep 27, 2019
iThenticate Software: Oct 17, 2019 (14%)
[1]. Goldblum JR, Folpe AL, Weiss SW, Enzinger and Weiss’s Soft Tissue Tumours 2014 6th edPhiladelphiaElsevier [Google Scholar]
[2]. Attafi S, Boujelbene N, Abbes I, Doghri R, Hamida NB, Ghorbel R, Vaginal Rhabdomyoma: A case report of an uncommon and misleading neoplasmaPathological 2007 109:382-83. [Google Scholar]
[3]. Kwiatkowska J, Waldoch A, Meyer Szary J, Potaz P, Grzybiak M, Cardiac tumours in children: A 20 year review of clinical presentation, diagnostics and treatmentAdv Clin Exp Med 2017 26:319-26.10.17219/acem/6212128791852 [Google Scholar] [CrossRef] [PubMed]
[4]. Patrelli TS, Franchi L, Gizzo S, Rhabdomyoma of the vagina. Case report and short literature reviewAnn Pathol 2012 32:53-57.10.1016/j.annpat.2011.08.01922325314 [Google Scholar] [CrossRef] [PubMed]
[5]. Kelekci S, Yazicioglu HF, Yilmaz B, Aygun M, Omeroglu RE, Cardiac rhabdomyoma with tuberous sclerosis: a case reportJ Reprod Med 2005 50:550-52. [Google Scholar]
[6]. Schoolmeester JK, Xing D, Keeney GL, Sukov WR, Genital rhabdomyoma of lower female genital tract: A study of 12 cases with molecular cytogenetic findingsInt J Gynecol Pathol 2017 0:01-07. [Google Scholar]
[7]. Losi L, Choreutaki T, Nascetti D, Recurrence in a case of rhabdomyoma of the vaginaPathologica 1995 87:704-08. [Google Scholar]
[8]. Andrade NN, Gandhewar T, Aggarwal N, Mathai P, Adult rhabdomyoma of the tongue in a child: Report of a case and a literature appraisalContemp Clin Dent 2018 9:02-04. [Google Scholar]