Typhoid fever is an important health concern across the globe. It is caused by the gram negative bacilli, Salmonella Typhi. The clinical manifestations range from a febrile systemic disease to varied spectrum of serious complications like intestinal perforation, circulatory collapse, meningitis and arthritis. Here, the present authors report one such rare complication; a case of rhabdomyolysis due to Salmonella Typhi. The patient came with chief complaints of fever, loose stools, weakness of limbs and inability to walk. As the case had an unusual presentation of gross motor dysfunction, it was challenging to clinically suspect the condition but laboratory investigations pointed towards the diagnosis of typhoid fever.
Blood culture, Creatine phosphokinase, Hepatomegaly, Myositis, Typhoid fever
Case Report
A 27-year-old female patient presented to the Department of General Medicine with history of fever and loose stools for 15 days, patient also had weakness of all four limbs since 3 days and slurring of speech since 1 day. The fever was intermittent with 39°C recorded during febrile episodes and not associated with chills and rigors. Routine blood checkup at a local health care centre was within normal limits and symptomatic treatment was given before admission at this tertiary care centre. The illness progressed with the patient developing profuse sweating followed by weakness of both lower limbs and inability to walk, imbalance and buckling of knees. It progressed to involve the upper limbs and the patient was unable to raise her arms above her head. Also, there was history of slurring of speech for 1 day. There was no history of similar episodes in the past, no history of seizures, hypertension or diabetes mellitus. There was no history of burning micturition, breathlessness or cough.
On examination, there was no pallor, icterus, cyanosis, lymphadenopathy or clubbing. Pulse rate was 102 beats/minute and Blood Pressure 110/80 mmHg. Abdomen was soft, tender with no organomegaly. Patient was conscious, alert and well oriented. Power in all 4 limbs was 4/5, which was assessed based on Medical Research Council (MRC) scale [1]. Bulk and tone were normal. Higher mental functions were normal. Cardiovascular and respiratory system were within normal limits. A provisional diagnosis of viral myositis was made. A detailed and systematic workup followed to arrive at the final diagnosis. Patient consent was taken for the admission and investigations.
Ultrasonography of the abdomen showed mild hepatomegaly (16 cm) and bilateral Grade I renal parenchymal changes. Cerebral scan results were normal. Chest X-ray and ECG were normal.
Haematology workup revealed a total leucocyte count of 2,200 cells/Cumm and platelet count of 58,000/Cumm. Peripheral smear showed normocytic normochromic blood picture. Biochemical workup revealed, blood urea of 48.7 mg/dL (normal 13-45 mg/dL), bilirubin direct 0.27 mg/dL (normal 0-0.25 mg/dL), Aspartate transaminase 333U/L (normal 0-40 U/L), Alanine aminotransferase 101 U/L (normal 0-40U/L), creatinine 1.44 mg/dL (normal 0.7-1.4 mg/dL), Creatine Phosphokinase (CPK) of 15,821 U/L (normal 0-109 U/L), Lactate dehydrogenase (LDH) 2732U/L (normal <250U/L). All serum electrolytes were lower than normal except sodium levels. Measured values were sodium 136 mmol/L, potassium 3.14 mmol/L, chloride 96.4 mmol/L, bicarbonate 8.6 mmol/L. magnesium 1.6 mg/dL. Urine analysis showed presence of protein and blood in urine. Stool microscopy showed presence of pus cells, no ova or cyst. Stool for occult blood was negative.
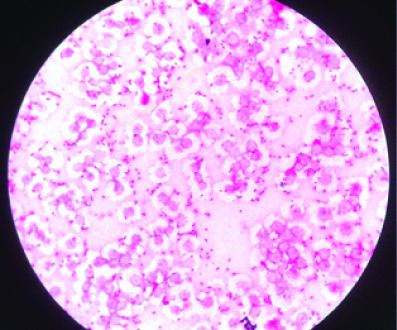
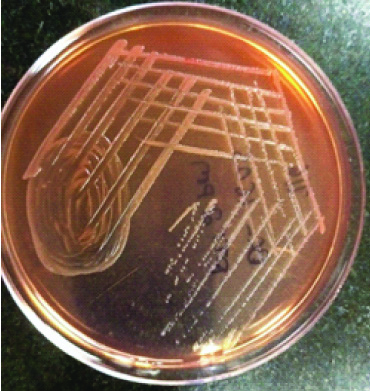
Serological tests for dengue and leptospira were negative. Antinuclear antibody profile was negative. Pair of blood samples were sent to microbiology laboratory for culture on the day of admission. Blood culture by automated BacT Alert system flagged presence of growth in both samples, 14 hours after incubation. Smear from broth revealed gram negative bacilli [Table/Fig-1]. The growth medium was subcultured onto blood agar and MacConkey’s agar. Next day, it revealed growth of non-lactose fermenting colonies [Table/Fig-2]. By conventional biochemical identification and agglutination with Salmonella specific antisera, it was identified as Salmonella Typhi. The organism was sensitive to ampicillin, ceftriaxone, azithromycin, cotrimoxazole and resistant to ciprofloxacin.
Gram stain from blood culture showing gram negative bacilli, Salmonella Typhi.
Non lactose fermenting colonies of the isolate, Salmonella Typhi on MacConkey’s agar.
Widal test was also asked for, when the blood culture yielded non lactose fermenting colonies resembling Salmonella, in order to support the diagnosis. It showed Salmonella Typhi O antibody titre 160 and Salmonella Typhi H antibody titre of >1280.
The findings of hepatomegaly, elevated liver enzymes and slightly elevated direct bilirubin levels indicated the presence of hepatitis. Proteinuria in the patient was more likely due to myoglobin, in the context of renal function tests not showing much abnormality with only slight elevation in blood urea and serum creatinine values. Urine and serum myoglobin could not be investigated as the test was not readily available at the health care centre and the patient got discharged on request. Muscular weakness, grossly elevated serum CPK, LDH levels and proteinuria pointed towards muscle destruction. Slight elevations in blood urea, serum creatinine could be due to bacterial toxin, dehydration or rhabdomyolysis. The patient had low WBC count and low platelet counts. Finally, microbiological isolation of Salmonella Typhi from the blood samples lead to the diagnosis of typhoid septicaemia with rhabdomyolysis and hepatitis.
On the day of admission, the patient had received empirical antibiotic treatment of injection Piperacillin-tazobactam 4.5 gm stat followed by 2.5 gm qid, injection metronidazole 500 mg tid and tablet doxycycline 100 mg bd and supportive therapy. She was treated in the intensive care unit, due to abnormal biochemical markers like very high serum CPK which increased to 28,176 U/L on day 2. Unfortunately, on the previous day of the microbiological diagnosis, the patient was discharged on request as they preferred to get treated at a different health care centre. Though a successful diagnosis was made, the patient was unwilling for treatment and was lost for follow-up.
Discussion
Direct invasion of the muscle by the infecting microorganism, action of a proteolytic toxin, tissue hypoxia due to sepsis, dehydration, electrolyte imbalance are the presumed mechanisms of rhabdomyolysis due to infections [2,3]. In this case, though presence of urine myoglobulin was not investigated, detection of proteins in urine could be due to myoglobulin. This suspicion coupled with very high CPK levels points towards typhoid rhabdomyolysis. The most sensitive laboratory indicator is gross elevation of CPK levels more than 5 times the upper limit of normal. Though the condition may be confirmed by myoglobinuria, following muscle injury plasma myoglobin increases rapidly and is cleared rapidly via renal excretion, with normal levels within 24 hours [4].
Recently a paediatric case of typhoid fever with haematopoetic lymphohistiocytosis and rhabdomyolysis was reported by Akkiz SY et al., [5]. In literature, similar to the present case, there are 16 cases of typhoid rhabdomyolysis; the details of some of them are shown in [Table/Fig-3] [6-11]. Pancreatitis was seen in 4 cases, neurologic complications in 8, cardiovascular in 1, hepatobiliary in 6 and pulmonary in 3 cases. All the cases showed complete recovery [6].
Reported cases of Salmonella Typhi bacteremia with rhabdomyolysis [6-11].
| Reference | Urine findings | Complications | Antibiotic therapy | Peak serum CPK level (IU/L) |
|---|
| Snelling PJ et al., [6] | Myoglobin+ | Encephalopathy, pancreatitis | Cefotaxime, azithromycin | 11,899 |
| Non LR et al., [7] | Blood+ | Hematophagocytic lymphohistiocytosis | Ceftriaxone | 83,550 |
| Ali M, Abdalla H, [8] | Unknown | Pancreatitis, polyneuropathy | Ciprofloxacin, imipenem | 17,000 |
| Jhawar M et al., [9] | Unknown | Acute renal failure | Piperacillin tazobactam, cefoperazone ciprofloxacin | 9473 |
| Al-aqeeda RF et al., [10] | Significant myoglobin, blood+ | Myocarditis, pulmonary oedema, multiorgan failure | Ceftriaxone | 6341 |
| Khan FY et al., [11] | Myoglobin+ | Renal failure, pancreatitis | Ceftriaxone | 5350 |
Paratyphoid fever and Non Typhoidal Salmonellae also can show manifestations like the present case. Sirmatel F et al., reported a fatal case of Salmonella paratyphi B septicaemia complicated by multiple organ dysfunction syndrome [12]. Chappel W et al., reported a case of Salmonella muenchen enteritis causing rhabdomyolysis (peak CPK 9830U/L) and myocarditis which was successfully treated with ceftriaxone [13].
Such cases can be managed by prompt and aggressive fluid replacement, antibiotic therapy like ceftriaxone, ciprofloxacin or azithromycin and close monitoring and prevention of impending complications like acute renal failure [2]. In the present case, symptoms of complications like muscle weakness were seen 12 days after the onset of fever. Early attempts to investigate the cause of fever would have prevented the complications.
Conclusion
Serum CPK levels though not a routine investigation; should be done if enteric fever is a suspicion. In areas of high endemicity, enteric fever must be an important differential diagnosis for fever and laboratory investigations specifically for the diagnosis of enteric fever, like blood culture and Widal test must be attempted so as to prevent the potential complications.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Aug 13, 2019
Manual Googling: Sep 26, 2019
iThenticate Software: Oct 14, 2019 (10%)
[1]. Medical Research Council. Aids to the examination of the peripheral nervous system, Memorandum no.45, Her Majesty’s Stationary Office, London, 1976. Available at https://mrc.ukri.org/documents/pdf/aids-to-the-examination-of-the-peripheral-nervous-system-mrc-memorandum-no-45-superseding-war-memorandum-no-7/ [Google Scholar]
[2]. Kahn FY, Rhabdomyolysis: a review of the literatureNetherlands the Journal of Medicine 2009 67(9):272-83. [Google Scholar]
[3]. Clowes GHA, George BC, Villee CA, Saravis CA, Muscle proteolysis induced by a circulating peptide in patients with sepsis or traumaN Engl J Med 1983 308:545-52.10.1056/NEJM1983031030810016828080 [Google Scholar] [CrossRef] [PubMed]
[4]. Nance JR, Mammen Al, Diagnostic evaluation of rhabdomyolysisMuscle Nerve 2015 51(6):793-810.10.1002/mus.2460625678154 [Google Scholar] [CrossRef] [PubMed]
[5]. Akkiz SY, Kamuram K, Hadi G, Mecnun C, Burcu G, Ahmet OF, Typhoid fever accompanied with hematopoetic lymphohistiocytosis and rhabdomyolysis in a refugee childJournal of Pediatric Hematology/Oncology 2019 41(4):e233-34.10.1097/MPH.000000000000140030608489 [Google Scholar] [CrossRef] [PubMed]
[6]. Snelling PJ, Moriarty P, Vaska VL, Levitt D, Nourse C, Rhabdomyolysis complicating Typhoid fever in a child and review of the literatureThe Pediatric Infectious Disease Journal 2017 36(9):915-16.10.1097/INF.000000000000161628430751 [Google Scholar] [CrossRef] [PubMed]
[7]. Non LR, Patel R, Esmaeeli A, Despotovic V, Typhoid fever complicated by hemophagocytic lymphohistiocytosis and rhabdomyolysisAm J Trop Med Hyg 2015 93:1068-69.10.4269/ajtmh.15-038526324725 [Google Scholar] [CrossRef] [PubMed]
[8]. Ali M, Abdalla H, Salmonella Typhi infection complicated by rhabdomyolysis, pancreatitis and polyneuropathyArab J Nephrol Transplant 2011 4:91-93. [Google Scholar]
[9]. Jhawar M, George P, Pawar B, Salmonella Typhi sepsis and rhabdomyolysis with acute renal failure: a rare presentation of a common diseaseSaudi J Kidney Dis Transpl 2010 21:732-34. [Google Scholar]
[10]. Al-aqeedi RF, Kamha A, Al-aani FK, Al-ani AA, Salmonella myocarditis in a young adult patient presenting with acute pulmonary edema, rhabdomyolysis, and multi-organ failureJ Cardiol 2009 54:475-79.10.1016/j.jjcc.2009.02.01119944325 [Google Scholar] [CrossRef] [PubMed]
[11]. Khan FY, Al-Ani A, Ali HA, Typhoid rhabdomyolysis with acute renal failure and acute pancreatitis: a case report and review of the literatureInt J Infect Dis 2009 13:e282-85.10.1016/j.ijid.2008.11.00919147385 [Google Scholar] [CrossRef] [PubMed]
[12]. Sirmatel F, Balci I, Sirmatel O, Bayazit N, Hocaoglu S, A case of Salmonella Paratyphi B Septicemia complicated by disseminated Intravascular Coagulation, Severe Hepatitis Rhabdomyolysis and Acute Renal FailureJournal of Infection 2001 43(19):i10.1016/S0163-4453(01)90843-6 [Google Scholar] [CrossRef]
[13]. Chapple W, Martell J, Wilson JS, Matsuura Dt, A case report of salmonella muenchen enteritis causing rhabdomyolysis and myocarditis in a previously healthy 26 year old manHawai’I Journal of Medicine and Public Health 2017 76(4):106-09. [Google Scholar]