Comparison of Two Different Glenoid Bone Loss Calculation Methods using Three-Dimensional Computed Tomography
Abhijit D Pawar1, Varsha P Rangankar2, Priya R Bhole3
1 Professor, Department of Radiology, Smt. Kashibai Navale Medical College and General Hospital, Narhe, Pune, Maharashtra, India.
2 Professor, Department of Radiology, Dr. D. Y. Patil Medical College, Hospital and Research Centre, Sant Tukaram Nagar, Pimpri, Pune, Maharashtra, India.
3 Senior Resident, Department of Radiology, JNU Institute of Medical Sciences and Research Center, Jaipur, Rajasthan, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Varsha P Rangankar, Professor, Department of Radiodiagnosis, Dr. D. Y. Patil Medical College, Hospital and Research Centre, Sant Tukaram Nagar, Pimpri, Pune, Maharashtra, India.
E-mail: varsharangankar@gmail.com
Introduction
An accurate estimation of the glenoid bone loss is an important factor in management of glenohumeral instability. Three-dimensional Computed Tomography (CT) technique is the most widely used modality. Various methods are used for glenoid bone loss calculations on CT.
Aim
To compare the two methods of glenoid bone loss evaluation namely, Griffith’s and Best fit circle method using three-dimensional CT.
Materials and Methods
A retrospective study was conducted in which a total of 34 patients with recurrent shoulder dislocations who underwent computed tomography, were included in the study. Scans were reconstructed using multiplanar reconstructions and bone loss was evaluated using the Griffith’s index and Best fit circle method. Quantitative data were calculated as mean±SD. The chi-squared test was used to determine the p-value.
Results
The mean for percentage glenoid bone loss using Griffith method was 18.8±6.6 and by best fit circle method was 18.8±5.9. The p-value was 1 and the t value was 0, proving that there is no statistical difference between both these tests.
Conclusion
The results of the study showed that best fit circle method is comparable to Griffith’s method for estimation of bone loss (p=1) and can be used alone on the affected glenoid.
Bankart’s lesion, Best fit method, Griffith’s method, Shoulder dislocation
Introduction
Glenohumeral instability with recurrent shoulder dislocation is a commonly encountered problem in clinical practice, requiring both Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) for complete evaluation [1,2]. Two major risk factors include Hill Sachs lesion and Bankart lesion, which can either be a soft tissue Bankart or a bony Bankart lesion. Glenoid bone loss results from a compression of the anterior glenoid rim during shoulder dislocations and represents the glenoid equivalent of a Hill-Sachs deformity [3-5]. Straightening of the anterior glenoid rim is the first finding seen on imaging [6]. As glenoid bone loss progresses, the anterior straight line lengthens and further progresses to become concave [6].
While soft tissue Bankart’s is conservatively managed, bony Bankart’s lesions require either arthroscopic or open surgery (Latarjet procedure) [7,8]. There is a higher incidence of arthroscopic failure with higher bone loss. Therefore, accurate evaluation of the glenoid bone loss is a prerequisite in deciding management of glenohumeral instability. Multiple modalities have been described to calculate the amount of bone loss. These include plain radiography, CT scan and MRI [9]. Many studies have compared the efficacy of these different modalities for evaluation of bone loss [10-13]. CT scan, especially the 3-dimensional CT (3D CT) technique, was proven to be the most accurate and hence widely used modality [4,9-12]. There are various methods to calculate bone loss on CT scan. These include Griffiths’ method [14], Best fit circle method [15], diameter method [16,17], surface area method [17] and Glenoid index [18]. These methods take into account the length, width and the area ratios of glenoid fossa on en-face view. The Griffith’s method is one of the earliest methods devised for bone loss quantification [14] by comparing the abnormal glenoid diameter with normal glenoid diameter and therefore cannot be used in bilateral shoulder dislocation. The Griffith’s method and most other described techniques necessitate scanning of both shoulders in all patients of shoulder dislocation increasing the radiation dose.
There is a need to have an accurate method of bone loss estimation which can be used unilaterally on the affected shoulder. Of all the available methods, Best fit circle method can be used unilaterally [15]. A search of the previously available English research literature did not reveal any study to compare various CT scan methods for evaluation of bone loss. In this study, the present authors compared the results of the two widely used methods for glenoid bone loss: Griffith index and Best fit circle method.
Materials and Methods
A retrospective study was conducted on CT scan examinations of 34 patients, who underwent bilateral shoulder joints CT scan in the institute, between June 2016 to December 2017. The study was carried out in Smt. Kashibai Navale Medical College and GH, Pune, Maharashtra, India. The local ethics committee approved the study (App/2019/547). The patients of unilateral recurrent shoulder dislocations who underwent CT were included in the study. Patients with bilateral shoulder dislocations were excluded from the present study.
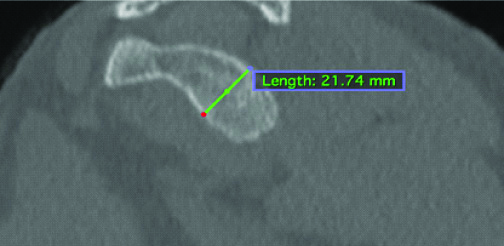
In the study institute, all CT scans are performed on a Multislice scanner (16 slice Revolution ACT, GE). The CT images are obtained with 0.875 collimation and 1 mm thickness using 50-160 mA, and 140 kVp with thin image reconstruction is done using high resolution bone algorithm in the axial plane with matrix size of 512×512. This image data is used to obtain coronal and sagittal reformatted images. The sagittal en-face views along the long axis of the glenoid fossa are obtained on workstation to assess the glenoid bone loss. Both the shoulders are scanned in the axial plane. Multiplanar reconstructions are performed on the axial images to obtain enface images of glenoid fossa. For this study, plane of evaluation was perpendicular to the long axis of glenoid fossa. Anteroposterior measurements of both glenoid fossae were taken for Griffith’s index evaluation [Table/Fig-1] [14].
Griffith’s index: Anteroposterior (AP) measurements were calculated in both glenoid fossae perpendicular to the long axis of glenoid. The difference in AP diameter of affected and unaffected side divided by the AP diameter of the unaffected side was used to calculate percentage bone loss.
The Best fit circle method has been first described by Huijsmans PE et al., [15]. A Best fit circle was made on the inferior two-thirds of the glenoid [Table/Fig-2]. The diameter of the circle and the anteroposterior diameter of the glenoid at the same level were measured [15]. Glenoid bone loss was the difference in these two diameters and expressed both in absolute terms (in millimetres) and as a percentage of the overall Best fit circle diameter.
Best fit circle method (Pico method): Circle was positioned at the inferior two thirds of the glenoid. Transverse diameter of the circle (blue line) and the actual transverse dimension of the glenoid (orange line) was obtained. The difference between the two was divided by the diameter of the circle to calculate percentage bone loss.
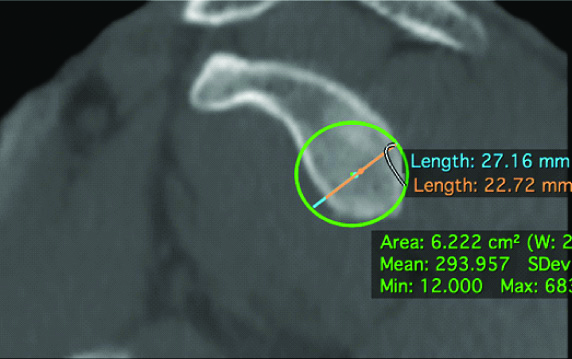
The principle of measuring bone defects on sagittal en-face views along the long axis of the glenoid fossa is due to circular appearance of inferior aspect of glenoid. The circle made to determine the bone loss is made along the posterior, anterior and inferior margins of the glenoid fossa [19].
The percentage bone loss values using Griffith’s method and the Best fit circle method were compared and statistical difference between the use of these two methods was calculated. Severe bone loss was expressed as more than 25% bone loss [20].
Statistical Analysis
Data collected using Griffith’s method and the Best fit circle method was entered in an excel sheet. Statistical analysis was done using PRIMER software. Quantitative data were calculated as mean±SD. The chi-squared test was used to determine the p-value.
Results
The glenoid bone loss was evaluated using the Griffith’s index and Best fit circle methods. The results are presented in [Table/Fig-3]. Out of 34 patients, 14 patients had bone loss of 5-15%, 16 patients had bone loss of 16-25% and 4 patients had bone loss of more than 25% as calculated by both Griffith’s and Best fit circle methods. The mean for percentage glenoid bone loss using Griffith method was 18.8±6.6 and by Best fit circle method was 18.8±5.9 [Table/Fig-4]. The means by both the methods were found to be the same and the t-value was 0 and p-value was 1. Thus, it was proved that results of both the methods were the same and these methods can be used together, either in conjunction or instead of each other for calculation of glenoid bone loss.
Classification of severity of bone loss using Griffith’s and Best fit circle method.
| Amount of bone loss | Number of patients (n=34) |
|---|
| Griffith’s method | Best fit method |
|---|
| 5-15% | 14 | 14 |
| 16-25% | 16 | 16 |
| Severe bone loss >25% | 4 | 4 |
Statistical comparison between Griffith’s and best fit method.
| Mean (CI 95%) | SD | p-value | t value |
|---|
| Griffith’s method | 18.8 | 6.6 | 1 | 0 |
| Best fit circle method | 18.8 | 5.9 |
CI: Confidence interval; SD: Standard deviation
Discussion
Surgical success and type of surgical repair for glenohumeral instability is based on the Glenoid bone loss [8,12,21-24]. In cases of mild to moderate bone loss arthroscopic soft-tissue stabilisation can be done, whereas, severe bone loss requires bone augmentation with open surgery [6-12]. There is higher failure rate of arthroscopic approach with the increase in the size of glenoid loss and Hill-Sachs lesions. Multiple studies have attempted various methods to characterise the glenohumeral bone loss to choose the surgical approach, preoperatively. However, no accepted definition of severe glenoid bone loss was found in the various available studies [25].
Rowe CR et al., described the relationship between amount of bone loss and risk of future redislocation after surgical treatment [25]. Many reports have tried to quantify the cut off values that may be used to decide between arthroscopic repair and open surgery with bone grafting for major glenoid bone loss [8,26]. According to Burkhart SS and De Beer JR, 67% of patients with a bone loss of 25% or more demonstrated redislocation after arthroscopic Bankart’s repair [27]. Also, Bigliani LU et al., reported an osseous loss of 25% of glenoid width as a significant glenoid bone loss in their study [20]. Dislocation frequency has been found to increase if bone loss is more than 15%, though 20%-25% is considered the threshold for severe bone loss [16,23]. The open surgery commonly performed is the Latarjet procedure for glenoid bone loss.
Griffith method is the oldest described method in the evaluation of bone loss [14]. This method assumes that one glenoid is normal and compares abnormal glenoid diameter with normal glenoid diameter. This does not hold true in cases of bilateral shoulder dislocation and hence, Griffith’s method cannot be used in these cases. In these patients, Best fit circle method can be performed. Also, to estimate bone loss using the Griffith’s method, patients need to undergo CT scan of both shoulders which further exposes the patients to additional radiation dose. Most other techniques that are described also take into account the contralateral shoulder, thus giving increased radiation dose. Another drawback of methods estimating bone loss by comparing both shoulders is that they cannot be used in bilateral dislocations.
Griffith’s method is found to be an accurate and reliable method for bone loss estimation [16] and of all the available methods, best fit method can be used unilaterally [15]. Therefore, the present authors compared both these widely used methods to estimate glenoid bone loss in the present study which revealed that results of both the methods were same (p-value=1) and these methods can be used together, either in conjunction or instead of each other. This is an important inference because, instead of scanning both shoulders for Griffith’s method which leads to increased radiation dose, only Best fit circle method can be used on the affected shoulder and get results which are comparable to highly accurate Griffith’s method. Similarly, this method can be used in cases of bilateral shoulder dislocation where Griffith’s method cannot be used.
Limitation
A small sample size, lack of gold standard in evaluation of glenoid bone loss methods and inability to confirm the bone loss intraoperatively are the limitations of the present study.
Conclusion
While a prerequisite for Griffith’s method is scanning bilateral shoulder joints, the Best fit circle method can be used unilaterally obviating the need for scanning of contralateral joint and thus reducing radiation dose. This is important as shoulder dislocation is a common entity in younger age groups where radiation doses have to be kept as low as possible. Best fit circle method also overcomes the drawback of Griffith’s method in bilateral shoulder dislocations.
The results of this study showed that Best fit circle method is comparable to Griffith’s method for estimation of bone loss (p=1) and can be used alone on the affected glenoid. This reduces the radiation dose as scanning of contralateral shoulder joint is not required.
CI: Confidence interval; SD: Standard deviation
Author Declaration:
Financial or Other Competing Interests: No
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jul 30, 2019
Manual Googling: Sep 20, 2019
iThenticate Software: Oct 14, 2019 (15%)
[1]. Bencardino JT, Gyftopoulos S, Palmer WE, Imaging in anterior glenohumeral instabilityRadiology 2013 269(2):323-37.10.1148/radiol.1312192624155283 [Google Scholar] [CrossRef] [PubMed]
[2]. Ruiz Santiago F, Martínez Martínez A, Tomás Muñoz P, Pozo Sánchez J, Zarza Pérez A, Imaging of shoulder instabilityQuant Imaging Med Surg 2017 7(4):422-33.10.21037/qims.2017.08.0528932699 [Google Scholar] [CrossRef] [PubMed]
[3]. Wolf EM, Anterior portals in arthroscopyArthroscopy 1989 5(3):201-08.10.1016/0749-8063(89)90172-2 [Google Scholar] [CrossRef]
[4]. Magarelli N, Milano G, Sergio P, Santagada DA, Fabbriciani C, Bonomo L, Intra-observer and interobserver reliability of the ’Pico’ computed tomography method for quantification of glenoid bone defect in anterior shoulder instabilitySkeletal Radiol 2009 38(11):1071-75.10.1007/s00256-009-0719-519466406 [Google Scholar] [CrossRef] [PubMed]
[5]. Sugaya H, Moriishi J, Dohi M, Kon Y, Tsuchiya A, Glenoid rim morphology in recurrent anterior glenohumeral instabilityJ Bone Joint Surg Am 2003 85-A(5):878-84.10.2106/00004623-200305000-0001612728039 [Google Scholar] [CrossRef] [PubMed]
[6]. Millett PJ, Clavert P, Warner JJ, Open operative treatment for anterior shoulder instability: when and why?J Bone Joint Surg Am 2005 87(2):419-32.10.2106/JBJS.D.0192115687170 [Google Scholar] [CrossRef] [PubMed]
[7]. Piasecki DP, Verma NN, Romeo AA, Levine WN, Bach BR Jr, Provencher MT, Glenoid bone deficiency in recurrent anterior shoulder instability: diagnosis and managementJ Am Acad Orthop Surg 2009 17(8):482-93.10.5435/00124635-200908000-0000219652030 [Google Scholar] [CrossRef] [PubMed]
[8]. Gill TJ, Micheli LJ, Gebhard F, Binder C, Bankart repair for anterior instability of the shoulder. Long-term outcomeJ Bone Joint Surg Am 1997 79:850-57.10.2106/00004623-199706000-000089199382 [Google Scholar] [CrossRef] [PubMed]
[9]. Provencher MT, Bhatia S, Ghodadra NS, Grumet RC, Bach BR Jr, Dewing CB, Recurrent shoulder instability: current concepts for evaluation and management of glenoid bone lossJ Bone Joint Surg Am 2010 92(Suppl 2):133-51.10.2106/JBJS.J.0090621123597 [Google Scholar] [CrossRef] [PubMed]
[10]. Nofsinger C, Browning B, Burkhart SS, Pedowitz RA, Objective preoperative measurement of anterior glenoid bone loss: a pilot study of a computer-based method using unilateral 3-dimensional computed tomographyArthroscopy 2011 27(3):322-29.10.1016/j.arthro.2010.09.00721195579 [Google Scholar] [CrossRef] [PubMed]
[11]. Boileau P, Villalba M, Héry JY, Balg F, Ahrens P, Neyton L, Risk factors for recurrence of shoulder instability after arthroscopic Bankart repairJ Bone Joint Surg Am 2006 88(8):1755-63.10.2106/00004623-200608000-0001016882898 [Google Scholar] [CrossRef] [PubMed]
[12]. Itoi E, Lee SB, Berglund LJ, Berge LL, An KN, The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: a cadaveric studyJ Bone Joint Surg Am 2000 82(1):35-46.10.2106/00004623-200001000-0000510653082 [Google Scholar] [CrossRef] [PubMed]
[13]. Saliken DJ, Bornes TD, Bouliane MJ, Sheps DM, Beaupre LA, Imaging methods for quantifying glenoid and Hill-Sachs bone loss in traumatic instability of the shoulder: a scoping reviewBMC Musculoskelet Disord 2015 16:16410.1186/s12891-015-0607-126187270 [Google Scholar] [CrossRef] [PubMed]
[14]. Griffith JF, Antonio GE, Tong CW, Ming CK, Anterior shoulder dislocation: quantification of glenoid bone loss with CTAJR Am J Roentgenol 2003 180(5):1423-30.10.2214/ajr.180.5.180142312704062 [Google Scholar] [CrossRef] [PubMed]
[15]. Huijsmans PE, Haen PS, Kidd M, Dhert WJ, van der Hulst VP, Willems WJ, Quantification of a glenoid defect with three-dimensional computed tomography and magnetic resonance imaging: a cadaveric studyJ Shoulder Elbow Surg 2007 16(6):803-09.10.1016/j.jse.2007.02.11518061117 [Google Scholar] [CrossRef] [PubMed]
[16]. Griffith JF, Antonio GE, Yung PS, Wong EM, Yu AB, Ahuja AT, Prevalence, pattern, and spectrum of glenoid bone loss in anterior shoulder dislocation: CT analysis of 218 patientsAJR Am J Roentgenol 2008 190(5):1247-54.10.2214/AJR.07.300918430839 [Google Scholar] [CrossRef] [PubMed]
[17]. Sanders TG, Morrison WB, Miller MD, Imaging techniques for the evaluation of glenohumeral instabilityAm J Sports Med 2000 28(3):414-34.10.1177/0363546500028003250110843139 [Google Scholar] [CrossRef] [PubMed]
[18]. Chuang TY, Adams CR, Burkhart SS, Use of preoperative three dimensional computed tomography to quantify glenoid bone loss in shoulder instabilityArthroscopy 2008 24:376-82.10.1016/j.arthro.2007.10.00818375267 [Google Scholar] [CrossRef] [PubMed]
[19]. Sonin A, Manaster BJ, Andrews CL, Diagnostic imaging: Musculoskeletal: Trauma 2011 1st edAmyrsis [Google Scholar]
[20]. Bigliani LU, Newton PM, Steinmann SP, Connor PM, Mcllveen SJ, Glenoid rim lesions associated with recurrent anterior dislocation of the shoulderAm J Sports Med 1998 26:41-45.10.1177/036354659802600123019474399 [Google Scholar] [CrossRef] [PubMed]
[21]. Mologne TS, Provencher MT, Menzel KA, Vachon TA, Dewing CB, Arthroscopic stabilization in patients with an inverted pear gleanoid: Results in patients with bone loss of the anterior glenoidAm J Sports Med 2007 35:1276-83.10.1177/036354650730026217387219 [Google Scholar] [CrossRef] [PubMed]
[22]. Sugaya H, Kon Y, Tsuchiya A, Arthroscopic repair of glenoid fractures using suture anchorsArthroscopy 2005 21:63510.1016/j.arthro.2005.02.00615891740 [Google Scholar] [CrossRef] [PubMed]
[23]. Sugaya H, Moriishi J, Kanisawa I, Tsuchiya A, Arthroscopic osseous Bankart repair for chronic recurrent traumatic anterior glenohumeral instability. Surgical techniqueJ Bone Joint Surg Am 2006 882:159-69.10.2106/00004623-200609001-00001 [Google Scholar] [CrossRef]
[24]. Hamamoto JT, Leroux T, Chahla J, Bhatia S, Higgins JD, Romeo AA, Assessment and evaluation of glenoid bone lossArthroscopy Techniques 2016 5(4):e947-51.10.1016/j.eats.2016.04.02727709063 [Google Scholar] [CrossRef] [PubMed]
[25]. Rowe CR, Patel D, Southmayd WW, The Bankart procedure: A long-term end-result studyJ Bone Joint Surg Am 1978 60:01-16. [Google Scholar]
[26]. Rockwood CA, Matsen FA, The Shoulder 1998 2nd edPhiladelphiaSaunders10.2106/00004623-197860010-00001 [Google Scholar] [CrossRef]
[27]. Burkhart SS, De Beer JF, Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: Significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesionArthroscopy 2000 16:677-94.10.1053/jars.2000.17715 [Google Scholar] [CrossRef]