Vernal Keratoconjunctivitis (VKC) is a chronic conjunctival inflammatory condition predisposed to atopic disease. It usually starts before the age of ten years and affects individuals in warm climates. It generally resolves after puberty. The disease is more common among male. Generally, most cases are bilateral (98%), with symmetrical involvement. Routine treatment to start with involves topical corticosteroids, mast cell stabilisers and cyclosporine. In recalcitrant cases supratarsal triamcinolone injection is also given. Hereby, three cases of grossly asymmetrical vernal keratoconjunctivitis has been reported. All cases were young boys with history of recurring severe itching and use of topical steroids along with topical mast cell stabilisers and cyclosporine. All cases in the recent episode of ocular allergy developed corneal involvement and treated with supratarsal triamcinolone and bandage contact lens.
Case Presentation
Case 1
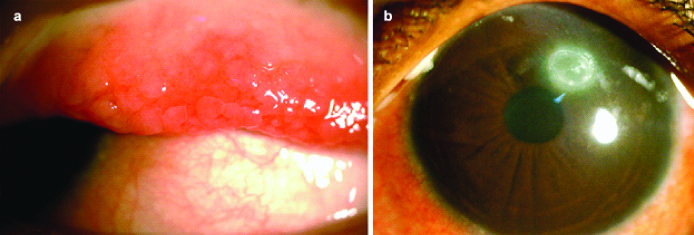
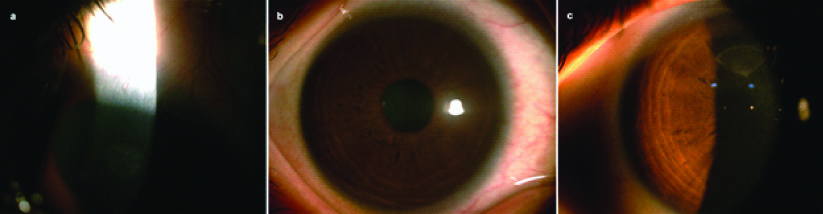
An eight-year-old young Indian boy residing in hot and humid coastal area, presented in tertiary eye hospital with irritation, photophobia, marked itching and ropy discharge in left eye from last two weeks. He had a history of recurrent itching in both eyes, more in left eye, from last 3 years. He was treated with topical steroids and mast cell stabilisers for every episode of allergy in last 3 years. From last one year he was also prescribed topical cyclosporine (CsA) 0.05%. There was history of skin allergy and wheezing suggestive of atopy in child from last three years. No similar history of ocular allergy and atopy was noted in family. There was no history of wearing contact lenses or ocular prosthesis in the child. Also, there was no past history of any type of ocular surgery done. His Best Corrected Visual Acuity (BCVA) was 20/20 in the right eye and 20/40 in the left. Intraocular Pressure (IOP) by Non-Contact Tonometer (NCT) in both eyes was 18 (Normal IOP is 12-22 mmHg). Clinical examination by slit lamp biomicroscopy of the right eye revealed micropapillae (Grade 1) [1], tarsal and limbal papillae with conjunctival congestion and clear cornea. He had Grade 2 shield ulcer [2] on cornea and Grade 4 tarsal or cobblestone papillae in left eye. Rest examination of the anterior and posterior segment was normal [Table/Fig-1].
Case 1- Vernal keratoconjuntivitis of left eye (pre supra-tarsal triamcinolone injection): a) Cobblestone papillae at upper tarsal conjunctiva; b) Shield ulcer on cornea.
Case 2
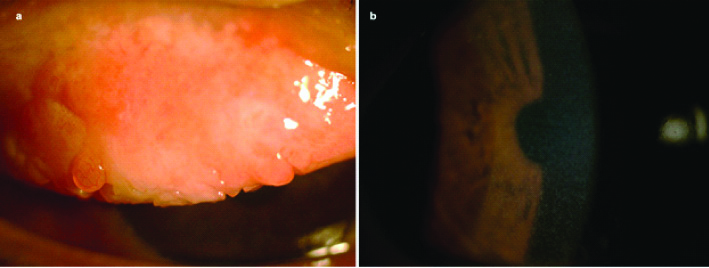
A six-year-old Indian boy residing in hot and dry area presented in tertiary eye hospital with increased itching, ropy discharge and rubbing in right eye from last one month. Patient had history of recurrent itching in both eyes from last two years. It was always more symptomatic in right eye. Patient also complained of recurrent skin allergy and wheezing from three years. There were no significant family history of ocular allergy or atopy. There was no history of wearing contact lenses or ocular prosthesis in the child. Also, there was no past history of any type of ocular surgery done. He has been intermittently using topical steroids, mast cell stabilisers and cyclosporine 0.05% from last two years. His BCVA was 20/40 in right eye and 20/20 in left eye. IOP by NCT in right eye was 14 and left eye was 18. On examination, his right eye had Grade 4 tarsal or cobblestone papillae with mucus discharge and severe grade of superficial punctate epitheliopathy [Table/Fig-2] while left eye had Grade 1 tarsal papillae and clear cornea. Rest of the anterior and posterior segment was within normal limits.
Case 2- Vernal keratoconjuntivitis right eye (pre supra-tarsal triamcinolone injection): a) Cobblestone papillae at upper tarsal conjunctiva; b) Generalised superficial punctate epitheliopathy on cornea.
Case 3
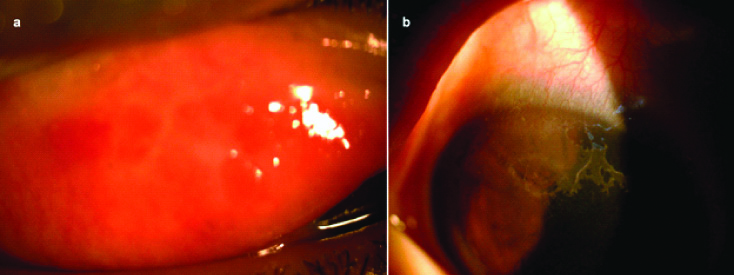
A seven-year-old Indian boy from hot and dry place presented in tertiary eye hospital with itching in both eyes with right more symptomatic from last one year. Recently, patient presented with marked itching and rubbing followed by tearing and blurring of vision in right eye. Patient was on topical steroids, mast cell stabilisers and cyclosporine 0.05% from last one year intermittently. There was no history of atopy. No positive family history was reported. His BCVA in right eye was 20/60 and left eye 20/40. IOP by NCT in both eyes was 16. On clinical examination with slit lamp, his right eye had macroerosion (coalescent epithelial loss) on superior part of cornea and Grade 4 tarsal or cobblestone papillae along with superficial punctate epitheliopathy [Table/Fig-3]. In left eye, clear cornea and Grade 1 papillae were present. Rest of the anterior and posterior segment was normal.
Case 3- Vernal keratoconjuntivitis right eye (pre supra-tarsal triamcinolone injection): a) Cobblestone or giant papillae with mucus; b) Macroerosion in superior part of cornea.
All cases were diagnosed as asymmetric vernal keratoconjunctivitis clinically.
Treatment and Follow-up of all Three Cases
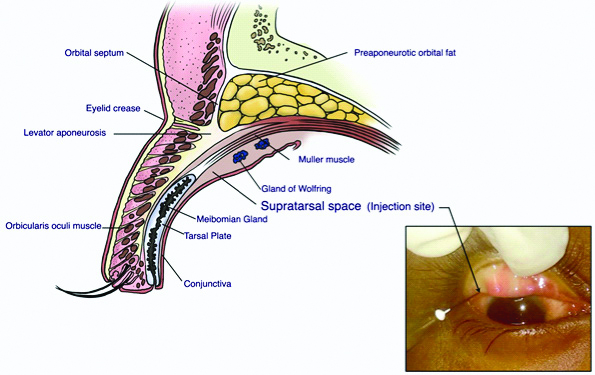
All patients were treated previously by topical steroids, mast cell stabilisers and cyclosporine 0.05% intermittently. VKC being intractable in nature was never fully cured and further episodes kept on occurring in all patients. In the latest episode of VKC of all three cases, as cornea was involved, planning for an alternative treatment was done. In all three patients, supratarsal injection of 20 mg triamcinolone acetonide was advised. It was injected in potential space between conjunctiva and Muller’s muscle with 27 gauge needle in the respective eyes under topical anaesthesia (eyedrop proparacaine 0.5%) followed by bandage contact lens application [Table/Fig-4]. Post supratarsal injection, all three children were advised topical lubricating eye drops (preservative free), topical fluorometholone 0.1% for one month and topical moxifloxacin 0.5% for one week.
Diagram of upper lid section and image of everted upper lid showing supratarsal space, the site of injection.
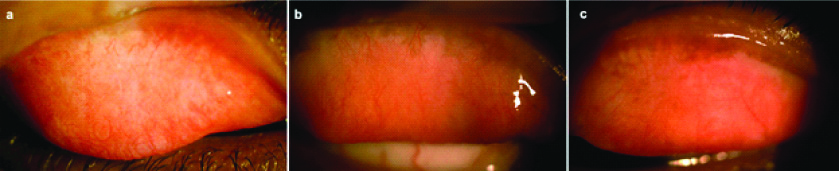
After 1 week of supratarsal injection, superficial punctate epitheliopathy cleared completely and after 6 weeks, shield ulcer healed leaving nebular grade corneal opacity [Table/Fig-5]. Cobblestone papillae resolved in 4 to 6 weeks [Table/Fig-6]. All patients were followed-up for one-year. None of them got any recurrences. Intraocular pressure on every visit was normal.
Healed keratopathies (post supra-tarsal triamcinolone injection and bandage contact lens application): a) Case 1- Healed shield ulcer (nebular grade corneal opacity); b) Case 2- Resolved superficial punctate epitheliopathy; c) Case 3- Healed macroerosion (nebular grade corneal opacity).
Post supra-tarsal triamcinolone injection: a-c) Resolved cobblestone or giant papillae.
Discussion
VKC is a chronic conjunctival inflammatory condition predisposed to atopic disease. It usually starts before the age of 10 years and affects individuals in warm climate. It generally resolves after puberty. The disease is more common in males with male to female ratio of 4:1 to 2:1. The disease though is seasonal can be perennial or persistent in tropical and subtropical climate [3]. It is traditionally considered as a type 1 hypersensitivity reaction [4]. Recent studies describe more complex and multifactorial pathogenesis mediated by Th2 lymphocytes, eosinophils, IgE, mast cells, interleukin and other mediators [1].
Diagnosis is mainly clinical with typical signs and symptoms including intense itching, photophobia, ropy discharge, giant papillae on the upper tarsal conjunctiva and/or at the limbus, superficial keratopathy and corneal shield ulcer [1]. All three cases were diagnosed clinically due to presence of typical clinical features.
VKC is usually chronic, bilateral and symmetrical eye disease. However, asymmetrical cases can be found but unilateral cases are extremely rare [5,6]. Bonini S et al., in their study stated that 98% of 195 patients with VKC were bilateral [1]. A demographic and epidemiologic study by Leonardi A et al., described that 96.7% of 406 cases of VKC were bilateral [7]. Bilateral involvement was seen in 100% cases in study by Kansakar I [8]. Similarly, Koki G et al., noted bilaterality in all patients of VKC in their study [9].
In grossly asymmetric cases, Giant Papillary Conjunctivitis (GPC) should be ruled out. This condition occurs primarily in contact lens wearers but can also occur in patients using ocular prosthesis and exposed suture [10]. All the three cases had no history of wearing of contact lenses or ocular prosthesis and undergoing any ocular surgery. Sometimes conjunctival tumors can mimic allergic conjunctivitis [11]. Incisional biopsy should be advised if there is no improvement in clinical condition with routine treatment. However, in this study incisional biopsy was not advised in any of the cases because diagnosis of VKC was clear due to typical clinical features.
The currently available drugs to treat VKC include antihistamines, mast cell stabilisers, dual acting agents, corticosteroids and immunomodulators. But none is enough to treat all aspects of this multifactorial disease. Apart from pharmacological treatment, surgical treatment are needed which include giant papillae removal by surgical excision, cryocoagulation, CO2 laser, debridement of ulcer base, surgical removal of plaque, excimer laser phototherapeutic keratectomy and amniotic membrane transplantation for vernal shield ulcer [3]. But in this case series, surgical treatment was not opted both for giant papillae and shield ulcer, thus avoiding need for intravenous or general anaesthesia.
Supratarsal steroid injection has appeared to be an efficacious and comparatively safe treatment for refractory VKC [12-14]. Both short acting dexamethasone and intermediate acting triamcinolone are equally effective with low risk of increased intraocular pressure [13,14]. Previous studies have reported a 50% decrease in papillae size with complete healing of shield ulcer [12]. In addition, a case report by Thanathanee O et al., showed asymmetric VKC treated by supratarsal triamcinolone injection in a six-year-old girl with 100% decrease in papillae in two months. The report observed no recurrence of VKC in child for 18 months after two supratarsal injections [15]. Qamar MR et al., found 100% effectiveness of supratarsal triamcinolone in their study with infrequent side effects [16]. Similarly, McSwiney TJ et al., in their study on 25 patients found supratarsal triamcinolone injection to be 100% effective in severe cases of VKC, refractory to topical medications, but gross asymmetry in the cases was not mentioned [17]. In this case series, all three young boys were given supratarsal injection only once with complete resolution of giant papillae, epitheliopathy and shield ulcer within 6 weeks. None of them developed any recurrence over the year. In addition, bandage contact lens were used for fast healing of shield ulcer and epitheliopathy.
Reported ocular complications of VKC include steroid-induced cataract, glaucoma, corneal scarring, microbial keratitis and limbal tissue hyperplasia [18]. None of the cases showed complications like steroid induced glaucoma, cataract or infectious keratitis due to injection per se.
Though topical steroids are the mainstay treatment for acute episode of VKC, steroid sparing therapies including immunomodulators like CsA (0.05-2%) and tacrolimus (0.03-0.1%) are also effective for refractory VKC. Topical CsA 0.05% is most frequently studied and is safe and effective in controlling symptoms and signs of VKC on long term basis [19-21]. But in this study, topical CsA was found to be less effective during acute episodes of VKC. Topical Tacrolimus is yet another immunomodulator similar to CsA in action and its ointment formulations of 0.1% and 0.03% have been found to be safe and effective for severe allergic conjunctivitis. The studies done by Chatterjee S and Agrawal D, and Al-Amri AM et al., showed significant improvement in symptoms and signs of refractory VKC with 0.1% and 0.03% tacrolimus eye ointment respectively. Both the studies showed transient stinging sensation as the only side effect of tacrolimus eye ointment [22,23]. Furthermore, future Randomised Control Trials (RCT’s) are required before considering tacrolimus as safe first line therapy for VKC. In this study tacrolimus was not advised to the patients. There are few case reports suggesting effectiveness of systemic immunosuppressive drugs for refractory severe VKC. Gokhale NS et al., has reported dramatic response to oral cyclosporine in a refractory case of severe VKC [24]. Also, Doan S et al., and Santamaria L and Sanchez J, in their respective case reports found systemic omalizumab to be effective for severe VKC, refractory to traditional treatments [25,26]. Long-term therapy and systemic side effects are not making systemic immunosuppressive therapy a feasible choice in severe and refractory VKC. Hence, for severe cases of VKC refractory to topical therapy or with involvement of cornea, supratarsal triamcinolone injection is a quick and effective treatment choice with effect of one injection lasting for about 10 months.
Conclusion
VKC is usually chronic, bilateral and symmetrical eye disease. Gross asymmetry of the disease is not that common. Supratarsal steroid injection is an effective therapeutic approach to treat refractory vernal keratoconjunctivitis especially when cornea is involved. It can be given under topical anaesthesia as an outdoor procedure even in young children. Since the treatment is quite effective, there is a decreased chance of corneal scarring, leading to good visual rehabilitation.
[1]. Bonini S, Bonini S, Lambiase A, Marchi S, Pasqualetti P, Zuccaro O, Vernal keratoconjunctivitis revisited. A case series of 195 patients with Long term Follow-upOphthalmology 2000 107(6):1157-63.10.1016/S0161-6420(00)00092-0 [Google Scholar] [CrossRef]
[2]. Cameron JA, Shield ulcers and plaques of the cornea in vernal keratoconjunctivitisOphthalmology 1995 102(6):985-93.10.1016/S0161-6420(95)30925-6 [Google Scholar] [CrossRef]
[3]. Kumar S, Vernal keratoconjunctivitis: a major reviewActa Ophthalmol 2009 87(2):133-47.10.1111/j.1755-3768.2008.01347.x18786127 [Google Scholar] [CrossRef] [PubMed]
[4]. Allansmith MR, Ross RN, Ocular allergyClin Allergy 1988 18:01-36.10.1111/j.1365-2222.1988.tb02837.x3280160 [Google Scholar] [CrossRef] [PubMed]
[5]. Awwad ST, Najjar DM, Arlette A, Haddad RS, Vernal keratoconjunctivitis presenting unilaterallyJ Pediatr Ophthalmol Strabismus 2006 43(3):179-80.10.1177/11206721070170061718050126 [Google Scholar] [CrossRef] [PubMed]
[6]. Keklikci U, Soker SI, Soker Cakmak S, Ozkul S, Sakalar YB, Unlu K, Unilateral vernal keratoconjunctivitis: a case reportEur J Ophthalmol 2007 17(6):973-75. [Google Scholar]
[7]. Leonardi A, Busca F, Motterle L, Cavarzeran F, Fregona IA, Plebani M, Case series of 406 vernal keratoconjunctivitis patients: a demographic and epidemiological studyActa Ophthalmologica Scandinavica 2006 84:406-10.10.1111/j.1600-0420.2005.00622.x16704708 [Google Scholar] [CrossRef] [PubMed]
[8]. Kansakar I, Profile of vernal keratoconjunctivitis in Nepal: a hospital based studyNepal Med Coll J 2011 13(2):92-95. [Google Scholar]
[9]. Koki G, Omgbwa Eballe A, Epee E, Njuenwet Njapdunke SB, Souleymanou Wadjiri Y, Bella Assumpta L, Tropical endemic limboconjunctivitis (vernal conjunctivitis) in northern CameroonJ Fr Ophthalmol 2011 34(2):113-17.10.1016/j.jfo.2010.09.02121183244 [Google Scholar] [CrossRef] [PubMed]
[10]. Friedlaender MH, Ocular allergyCurr Opin Allergy Clin Immunol 2011 11(5):477-82.10.1097/ACI.0b013e32834a965221822130 [Google Scholar] [CrossRef] [PubMed]
[11]. Lee DH, Sohn HW, Park SH, Kang YK, Bilateral conjunctival mucosa-assisted lymphoid tissue lymphoma misdiagnosed as allergic conjunctivitisCornea 2001 20(4):427-29.10.1097/00003226-200105000-0001911333335 [Google Scholar] [CrossRef] [PubMed]
[12]. Singh S, Pal V, Dhull CS, Supratarsal injection of corticosteroids in the treatment of refractory vernal keratoconjunctivitisIndian J Ophthalmol 2001 49:241-45. [Google Scholar]
[13]. Saini JS, Gupta A, Pandey SK, Gupta V, Gupta P, Efficacy of supratarsal dexamethasone versus triamcinolone injection in recalcitrant vernal keratoconjunctivitisActa Ophthalmol Scand 1999 77(5):515-18.10.1034/j.1600-0420.1999.770505.x10551290 [Google Scholar] [CrossRef] [PubMed]
[14]. Holsclaw DS, Whitcher JP, Wong IG, Margolis TP, Supratarsal injection of corticosteroid in the treatment of refractory vernal keratoconjunctivitisAm J Ophthalmol 1996 121(3):243-49.10.1016/S0002-9394(14)70271-5 [Google Scholar] [CrossRef]
[15]. Thanathanee O, Bhoomibunchoo C, Suwan-apichon O, Treatment of asymmetrical vernal conjunctivitis with supratarsal corticosteroid injectionBMJ Case Rep 2014 2014:bcr201420640110.1136/bcr-2014-20640125410033 [Google Scholar] [CrossRef] [PubMed]
[16]. Qamar MR, Latif E, Arain TM, Ullah E, Supratarsal injection of triamcinolone for vernal keratoconjunctivitisPak J Ophthalmol 2010 26(1):28-31. [Google Scholar]
[17]. McSwiney TJ, Power B, Murphy CC, Brosnahan D, Power W, Safety and Efficacy of Supratarsal Triamcinolone for Treatment of Vernal Keratoconjunctivitis in IrelandCornea 2019 38(8):955-58.10.1097/ICO.000000000000196331276459 [Google Scholar] [CrossRef] [PubMed]
[18]. Sridhar MS, Gopinathan U, Rao GN, Fungal keratitis associated with vernal keratoconjunctivitisCornea 2003 22(1):80-81.10.1097/00003226-200301000-0002012502957 [Google Scholar] [CrossRef] [PubMed]
[19]. Coban-karatas M, Ozkale Y, Altan-Yaycioglu R, Efficacy of topical 0.05% cyclosporine treatment in children with severe vernal keratoconjunctivitisTurk J Pediatr 2014 56(4):410-17. [Google Scholar]
[20]. Keklikci U, Dursun B, Cingu AK, Topical cyclosporine a 0.05% eyedrops in the treatment of vernal keratoconjunctivitis- randomised placebo -controlled trialAdv Clin Exp Med Off Organ Wroclaw Med Univ 2014 23(3):455-61.10.17219/acem/3714524979519 [Google Scholar] [CrossRef] [PubMed]
[21]. Yucel OE, Ulus ND, Efficacy and safety of topical cyclosporine A 0.05% in vernal keratoconjunctivitisSingapore Med J 2016 57(9):507-10.10.11622/smedj.201516126768065 [Google Scholar] [CrossRef] [PubMed]
[22]. Chatterjee S, Agrawal D, Tacrolimus in Corticosteroid Refractory Vernal KeratoconjunctivitisCornea 2016 35(11):1444-48.10.1097/ICO.000000000000091827310883 [Google Scholar] [CrossRef] [PubMed]
[23]. Al-Amri AM, Mirza AG, Al-Hakami AM, Tacrolimus ointment for treatment of vernal keratoconjunctivitisMiddle East Afr J Ophthalmol 2016 23(1):135-38.10.4103/0974-9233.16461626957853 [Google Scholar] [CrossRef] [PubMed]
[24]. Gokhale NS, Samant R, Sharma V, Oral cyclosporine therapy for refractory severe vernal keratoconjunctivitisIndian J Ophthalmol 2012 60(3):220-23.10.4103/0301-4738.9587822569387 [Google Scholar] [CrossRef] [PubMed]
[25]. Doan S, Amat F, Gabison E, Saf S, Cochereau I, Just J, Omalizumab in severe refractory vernal keratoconjunctivitis in children: case series and review of the literatureOphthalmol Ther 2017 6(1):195-206.10.1007/s40123-016-0074-227909980 [Google Scholar] [CrossRef] [PubMed]
[26]. Santamaria L, Sanchez J, Long term efficacy of omalizumab in patients with conventional treatment-resistant vernal keratoconjunctivitisRev Alerg Mex 2018 65(2):192-96.10.29262/ram.v65i2.29229983017 [Google Scholar] [CrossRef] [PubMed]