Multidrug Resistance in an Emerging Group of Enterobacteriaceae: A Retrospective Analysis at a Tertiary Hospital in Haryana, India
Shalini Upadhyay1, Sharmila Sengupta2, Kaitlin F Mitchell3, Nasia Safdar4
1 DNB, Department of Microbiology, Medanta-The Medicity, Gurgaon, Haryana, India.
2 Head, Department of Microbiology, Medanta-The Medicity, Gurgaon, Haryana, India.
3 PhD, Department of Medicine, Division of Infectious Diseases, University of Wisconsin, Madison, WI, USA.
4 PhD, Department of Medicine, Division of Infectious Diseases, University of Wisconsin, Madison, WI, USA.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shalini Upadhyay, Department of Microbiology and Infection Control, Medanta-The Medicity, Gurgaon, Haryana, India.
E-mail: shalini.upd@gmail.com
Introduction
The SPICE group of Enterobacteriaceae (Serratia, Providencia, ‘Indole positive’ Proteus and other common species of Proteus, Citrobacter, and Enterobacter species) have emerged as causes of infection in otherwise healthy patients, and are especially concerning due to their intrinsic resistance to several last-resort antibiotics.
Aim
To estimate the trend of incidence and resistance pattern among SPICE group organisms and its association with the increased use of antibiotics.
Materials and Methods
This was a single center, retrospective study conducted over a period of five years (January 2011 to December 2015). Clinical specimens from patients were collected and bacterial organisms were identified and tested for antibiotic susceptibility. The level of antibiotic usage was also analysed throughout the study period.
Results
Levels of all SPICE group organisms has increased over the course of the study, with several genera exhibiting notable increases when each year of the study period and was compared to the baseline year. Most of the SPICE organisms exhibited decreased sensitivity to each of nine tested antibiotics. Usage of several antibiotics was also found to increase over the study period.
Conclusion
This study demonstrates the rising incidence of SPICE group Enterobacteriaceae, which coincided with increased dispensing of antibiotics at our institution. In institutions with limited resources, the monitoring of antibiotic usage is especially important in curtailing the emergence of drug resistant infections.
Amp C β-lactamase, Gram negative infection, Inducible resistance, SPICE group
Introduction
Pathogens within the Enterobacteriaceae family are the cause of diverse infections, and several members pose significant challenges in the global fight against antibiotic resistance. Enterobacteriaceae that produce Extended Spectrum Beta-Lactamases (ESBLs) have led to the increased use of broad-spectrum antibiotics including beta-lactam/beta-lactamase-inhibitors, third and fourth generation cephalosporins, carbapenems, tigecycline, and colistin [1]. The carbapenems-resistant Enterobacteriaceae (CRE) are associated with significant morbidity and mortality, and have been ranked by the Centers for Disease Control and Prevention as an urgent issue for antibiotic resistance [2]. Within this family, Klebsiella and Escherichia coli have been the most closely studied as they are most prevalent and major causes of illness, especially in the hospital setting [3].
However, other members of the Enterobacteriaceae are emerging as causes of healthcare-associated infections, including those in the SPICE group (Serratia, Providencia, ‘Indole positive’ Proteus and other common species of Proteus, Citrobacter, and Enterobacter species) [4,5]. Infections with these organisms have historically been limited to immuno-compromised patients or those with severe illness, but have become increasingly common in otherwise healthy patients over the past two decades [1,2,6].
SPICE organisms pose several challenges in terms of drug resistance. They exhibit inducible resistance to β-lactam antibiotics, and some species in this group have intrinsic resistance to colistin [4,5,7]. This leaves clinicians with very few treatment options, since colistin and tigecycline are the only two last-resort antibiotics that typically have in-vitro activity against CREs [8,9]. At one tertiary facility, increasing frequency of CRE organisms prompted high usage of colistin, which was linked to subsequent increase in Providencia stuartii [3].
During the past five years, the incidence of MDR SPICE organisms has increased at our institution in Haryana, India, and in response broad spectrum antibiotics have been utilised with increasing frequency. The present study aimed to estimate if the incidence of SPICE group organisms has also increased during this time period, and if this is associated with the use of these last-resort antibiotics.
Materials and Methods
Study Location
The authors performed a retrospective descriptive study to estimate the incidence of SPICE group of Enterobacteriaceae over a five-year period (January 2011 to December 2015). The study was conducted at an acute care, tertiary center located in Haryana, India. Data were obtained from the hospital’s microbiology Laboratory Information System (LIS), and the data regarding the consumption of antibiotics was taken from pharmacy. The following information was collected: number of samples received in the laboratory for culture, number of positive cultures, micro-organisms detected, their antimicrobial susceptibility, and consumption of antibiotics over the period of the study. The isolation of the microorganisms included in the SPICE group was the inclusion criteria and any other microorganism or no growth was excluded from the study.
Sample and Data Collection
Cultures for in-patients were obtained from blood, urine, lower respiratory tract specimens, and from any other site with a clinical suspicion of infection. Apart from the above mentioned samples, pus samples were also included if there were clinical sign and symptoms of Infection (eg., fever, inflammation etc.,). Bacteria were cultured using standard microbiological methods. Organism identification was performed by an automatic VITEK 2 system (bioMe’rieux, Marcy I’Etoile, France) using the Gram Negative (GN) Card according to the manufacturer’s guidelines. Antimicrobial susceptibility testing was also done using the VITEK 2 system with customised antimicrobial susceptibility testing cards. These tests were interpreted according to the criteria of the Clinical and Laboratory Standards Institute [10].
The number of positive samples for each genus in the SPICE group and their antibiotic susceptibility rates were computed for each year of the study. Consumption of each antibiotic, during the study period was also reported. To remove any bias associated with repeated sampling, only the first positive culture from each patient was included in the assessment of incident cases. Since laboratory data were studied without reviewing personal and individual clinical records, specific institutional ethics review was not required.
Statistical Analysis
To determine if there was an association between levels of antibiotic susceptibility and consumption, two-sample tests for proportions were performed between each combination of consecutive years. A p-value <0.05 was considered statistically significant. Data were analysed using SPSS software Version 20.0.
Results
Patient samples were tested for growth of microorganisms and antibiotic susceptibilities during the five-year study period. The percentage of positive samples remained stable throughout the study period. During the first year (2011), there were 7,553 positive samples out of 41,203 tested (18.3%). In the last year of the study (2015), there were 14,483 positive samples out of 81,024 tested (17.8%). The distribution of SPICE group Enterobacteriaceae and their antibiotic susceptibility results are shown in [Table/Fig-1]. All SPICE organisms were more abundant at the end of the study period compared to the beginning [Table/Fig-1]. Four genera exhibited statistically significant increases when comparing each year of the study to the initial study year (2011): Serratia in 2014 (p=0.018), Proteus in 2013 (p=0.034), Providencia in 2013 (p=0.007), and Enterobacter in 2014 (p=0.001). All SPICE organisms also showed a decreasing susceptibility phenotype to each tested antibiotic, with only three exceptions (Providencia with ceftriaxone, Citrobacter with gentamicin, and Enterobacter with doripenem).
Incidence of the SPICE group of Enterobacteriaceae with their susceptibility pattern (2011-2015).
| Year | No. of isolates | Susceptibility rate (%) |
|---|
| | AMK %S | CRO %S | CIP %S | DOR %S | ETP %S | GEN %S | IPM %S | MEM %S | TZP %S |
|---|
| Serratia species |
| 2011 | 44 | 90.7 | 83.7 | 81.8 | NA | 100 | 84.1 | 90.9 | 90.9 | 88.6 |
| 2012 | 43 | 83 | 79.1 | 81.4 | NA | 90.9 | 88.4 | 88.4 | 90.7 | 76.7 |
| 2013 | 102 | 78.2 | 50.8 | 64.4 | 78.4 | 88.9 | 55.4 | 63.4 | 78.2 | 59 |
| 2014 | 121 | 80.2 | 40 | 67.8 | 73.1 | 76.9 | 64.5 | 66.1 | 70.2 | 72.6 |
| 2015 | 87 | 89.5 | 41.2 | 67 | 70.1 | 81.2 | 67.4 | 75 | 70.9 | 70 |
| Proteus species |
| 2011 | 45 | 82.2 | 52.3 | 28.9 | NA | NA | 48.9 | NA | 97.1 | 91.8 |
| 2012 | 91 | 78.2 | 47.8 | 18.7 | NA | NA | 43.3 | NA | 94.5 | 88.9 |
| 2013 | 99 | 69.7 | 46.4 | 16.3 | NA | NA | 38.4 | NA | 84.8 | 83.8 |
| 2014 | 83 | 51.8 | 33.3 | 18.1 | NA | NA | 24.1 | NA | 71.1 | 74.7 |
| 2015 | 104 | 47.1 | NA | 17.3 | NA | NA | 30.8 | NA | 57.7 | 71.6 |
| Providencia species |
| 2011 | 33 | NA | 9.4 | 6.1 | NA | NA | NA | NA | 18.2 | 9.1 |
| 2012 | 65 | NA | 9.1 | 5.5 | NA | NA | NA | NA | 16.2 | 9.1 |
| 2013 | 101 | NA | 10 | 4 | NA | NA | NA | NA | 10.9 | 8.9 |
| 2014 | 53 | NA | NA | 3.8 | NA | NA | NA | NA | 13.8 | 7.5 |
| 2015 | 80 | NA | NA | 2.5 | NA | NA | NA | NA | 11.2 | NA |
| Citrobacter species |
| 2011 | 14 | 77.1 | 38.6 | 40 | NA | 63.6 | 42.9 | 78.6 | 88.6 | 48.6 |
| 2012 | 21 | 71.4 | 33.8 | 42.9 | NA | 65 | 47.6 | 66.7 | 85.7 | 43.3 |
| 2013 | 38 | 76.3 | 28.9 | 23.7 | NA | 65.6 | 60.5 | 60.5 | 68.4 | 39.5 |
| 2014 | 47 | 73.2 | 31 | 25.5 | 40 | 53.6 | 31.9 | 31.9 | 36.2 | 31.9 |
| 2015 | 40 | 70 | 36.4 | 30 | 28.6 | 54.8 | 57.5 | 42.5 | 48.7 | 32.5 |
| Enterobacter species |
| 2011 | 125 | NA | 44.4 | 52.8 | NA | 73 | 58.4 | 68.8 | 67.2 | 50 |
| 2012 | 162 | NA | 30.2 | 37.7 | NA | 50.8 | 39.1 | 45.3 | 46.9 | 32.1 |
| 2013 | 191 | NA | 20.6 | 36.8 | 50 | 45.2 | 31.2 | 37 | 43.5 | 27.5 |
| 2014 | 254 | NA | 14.9 | 32.1 | 49.6 | 38.1 | 33.9 | 35.9 | 39.7 | 27.4 |
| 2015 | 201 | NA | 26.5 | 36.8 | 51.2 | 55.7 | 41.9 | 40.3 | 50.2 | 37.4 |
AMK: Amikacin; CRO: Ceftriaxone; CIP: Ciprofloxacin; DOR: Doripenem; ETP: Ertapenem; GEN: Gentamicin; IPM: Imipenem; MEM: Meropenem; TZP: Pipercillin-tazobactam; %S-Percentage-sensitivity; NA: Not applicable
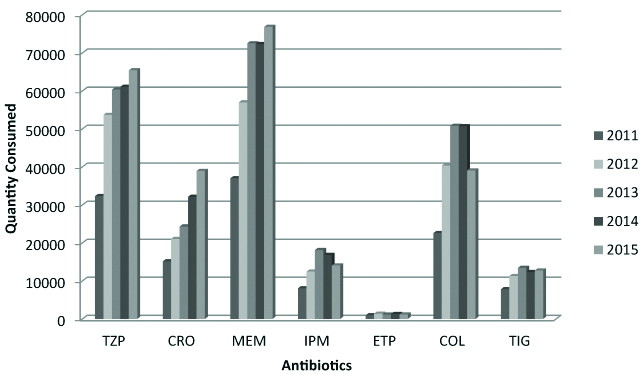
Antibiotic usage was found to increase over the study period [Table/Fig-2]. The quantity of antibiotic use significantly increased at several points of time compared to the start of the study: piperacillin-tazobactam, meropenem, and ceftriaxone at 2015, and imipenem and colistin at 2013 (p-value <0.05).
Consumption of antibiotics during each year of the study period.
TZP: Pipercillin-tazobactam; CRO: Ceftriaxone; MEM: Meropenem; IPM: Imipenem; ETP: Ertapenem; COL-Colistin; TIG: Tigecycline
Discussion
The increased frequency of CRE isolation at our facility has resulted in greater utilisation of broad-spectrum antibiotics during the study period. This study demonstrated that the incidence of SPICE group of Enterobacteriaceae has also increased. As tigecycline and colistin are not active against Serratia,Proteus, and Providencia, we hypothesised that there would be an association between increased usage of last-resort antibiotics and increased recovery of these micro-organisms due to selective antimicrobial pressure. The results of this study are in coherence with the above hypothesis.
Healthcare facilities in low or middle-income countries face many challenges in addressing drug resistance, which might help to explain the findings of the present study [11]. Most patients at our tertiary care facility have been prescribed at least one antibiotic prior to admission. Community pharmacies and self-prescription can also contribute to inappropriate antibiotic use in this region [12]. Resistance in the SPICE group can be attributed to a chromosomal β-lactamase gene known as AmpC [7], which is induced after a period of exposure to β-lactam antibiotics.
The findings highlight the importance of monitoring antibiotic usage and resistance at healthcare facilities, especially at those caring for large numbers of immuno-compromised and severely ill patients. In addition to the better-known CRE species, Enterobacteriaceae in the SPICE group should also be closely tracked for their frequency as well as carbapenemase production [1,3]. In regions where inappropriate use of antibiotics is common, it is especially important to consider these factors to ensure judicious dispensing of last-resort antibiotics and the possible treatment options for patients.
Limitation
As an observational study, the antibiotic type, dose, and duration were not manipulated, and may have varied based on the prescribing physician. In addition, not much attention has historically been given to these pathogens in reporting because of their rarity and low potential for nosocomial epidemics. Also, our study was conducted in a single center, and the findings may not be generalizable to other healthcare facilities with different rates of antibiotic usage or resistance. A larger study on transmission dynamics of the rising resistance amongst SPICE group of Enterobacteriaceae in hospitals will perhaps help in better prevention of these organisms within healthcare settings.
Conclusion
The present study draws attention to the rising incidence of SPICE group of pathogens in healthcare systems with high prevalence of multidrug resistant organisms. These seemingly milder pathogens are generally sensitive to a broad range of antibiotics, though intrinsically resistant to higher antibiotics such as colistin. Since not much work is being done in new antibiotic development; therefore, we need to preserve the currently available antibiotics for use in future. Failure of proper antimicrobial stewardship and breach in infection control practices can give rise to emergence of resistance in this group, leading to higher incidence of nosocomial infections with fewer options of treatment in acute care settings.
Future Recommendations
SPICE Group of Enterobacteriaceae should not be discarded as contaminants if significant counts are seen in the culture and they correlate with the clinical profile of the patient. Their empiric treatment should be based on the antibiogram of the facility. Further modifications should be done upon receiving the identification and antibiotic susceptibility test results from the clinical laboratory. A multicenter study needs to be done to know the trends in the susceptibility pattern of the SPICE group. Such studies will help in optimisation of treatment for these intrinsically resistant organisms.
AMK: Amikacin; CRO: Ceftriaxone; CIP: Ciprofloxacin; DOR: Doripenem; ETP: Ertapenem; GEN: Gentamicin; IPM: Imipenem; MEM: Meropenem; TZP: Pipercillin-tazobactam; %S-Percentage-sensitivity; NA: Not applicable
Author Declaration:
Financial or Other Competing Interests: No
Was Ethics Committee Approval obtained for this study? NA
Was informed consent obtained from the subjects involved in the study? NA
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Aug 12, 2019
Manual Googling: Sep 24, 2019
iThenticate Software: Oct 05, 2019 (14%)
[1]. Xu Y, Gu B, Huang M, Liu H, Xu T, Xia W, Epidemiology of carbapenem resistant Enterobacteriaceae (CRE) during 2000-2012 in AsiaJ Thorac Dis 2015 7(3):376-85. [Google Scholar]
[2]. Centers for Disease Control and Prevention. Antibiotic Resistance Threats in the United States; 2013. Available from: https://www.cdc.gov/drugresistance/threat-report-2013/index.html [Google Scholar]
[3]. Morrissey I, Hackel M, Badal R, Bouchillon S, Hawser S, Biedenbach D, A review of ten years of the study for monitoring antimicrobial resistance trends (SMART) from 2002 to 2011Pharmaceuticals 2013 6(11):1335-46.10.3390/ph611133524287460 [Google Scholar] [CrossRef] [PubMed]
[4]. Hayakawa K, Marchaima D, Divine GW, Pogue JM, Kumar S, Lephart P, Growing prevalence of Providencia stuartii associated with the increased usage of colistin at a tertiary health care centerInt J Infect Dis 2012 16(9):e646-48.10.1016/j.ijid.2012.05.102922818111 [Google Scholar] [CrossRef] [PubMed]
[5]. Bedenic B, Firis N, Gašparović VE, Krilanović M, Matanovíć K, Štimac I, Emergence of multidrug-resistant Proteus mirabilis in a long-term care facility in CroatiaWien Klin Wochenschr 2016 128(11-12):404-13.10.1007/s00508-016-1005-x27220339 [Google Scholar] [CrossRef] [PubMed]
[6]. Garbati MA, Bin Abdulhak A, Baba K, Sakkijha H, Infection due to colistin-resistant Enterobacteriacae in critically-ill patientsJ Infect Dev Ctries 2013 7(10):713-19.10.3855/jidc.285124129623 [Google Scholar] [CrossRef] [PubMed]
[7]. Choi SH, Lee JE, Park SJ, Choi SH, Lee SO, Jeong JY, Emergence of antibiotic resistance during therapy for infections caused by Enterobacteriaceae producing AmpC beta-lactamase: Implications for antibiotic useAntimicrob Agents Chemother 2008 52(3):995-1000.10.1128/AAC.01083-0718086837 [Google Scholar] [CrossRef] [PubMed]
[8]. Cornejo-Juárez P, Vilar-Compte D, Pérez-Jiménez C, Ñamendys-Silva SA, Sandoval-Hernández S, Volkow-Fernández P, The impact of hospital-acquired infections with multidrug-resistant bacteria in an oncology intensive care unitInt J Infect Dis 2015 31:31-34.10.1016/j.ijid.2014.12.02225528484 [Google Scholar] [CrossRef] [PubMed]
[9]. Olaitan AO, Morand S, Rolain JM, Mechanisms of polymyxin resistance: Acquired and intrinsic resistance in bacteriaFront Microbiol 2014 5:64310.3389/fmicb.2014.0064325505462 [Google Scholar] [CrossRef] [PubMed]
[10]. M100-S27: Performance Standards for Antimicrobial Susceptiility Testing. 2016, Clinical and Laboratory Standards Institute [Google Scholar]
[11]. Laxminarayan R, Chaudhury RR, Antibiotic resistance in India: Drivers and opportunities for ActionPLoS Med 2016 13(3):e100197410.1371/journal.pmed.100197426934098 [Google Scholar] [CrossRef] [PubMed]
[12]. Barker AK, Brown K, Ahsan M, Sengupta S, Safdar N, What drives inappropriate antibiotic dispensing? A mixed-methods study of pharmacy employee perspectives in Haryana, IndiaBMJ Open 2017 7(3):e01319010.1136/bmjopen-2016-01319028255093 [Google Scholar] [CrossRef] [PubMed]