An Intriguing Case of Chronic Cough in a Child
Gautam Bir Singh1, Vishaka Bettadahalli2, Sonali Malhotra3, Arun Krishna4
1 Professor, Department of Otorhinolaryngology, Lady Hardinge Medical College and Associated Hospitals, New Delhi, India.
2 Senior Resident, Department of Otorhinolaryngology, Lady Hardinge Medical College and Associated Hospitals, New Delhi, India.
3 Junior Resident, Department of Otorhinolaryngology, Lady Hardinge Medical College and Associated Hospitals, New Delhi, India.
4 Senior Resident, Department of Otorhinolaryngology, Lady Hardinge Medical College and Associated Hospitals, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Gautam Bir Singh, House No; 1433/Sector 15, Faridabad-121007 [NCR], Haryana, India.
E-mail: gbsnit@yahoo.co.in
Foreign body, Unwitnessed, Whistle
An eight-year-old child presented with chronic cough for the past six months with occasional history of wheeze. He had been treated on the lines of reflex laryngo-pharyngitis, asthma and allergic cough. Patient was also initiated on anti-tubercular drugs, but his cough did not subside.
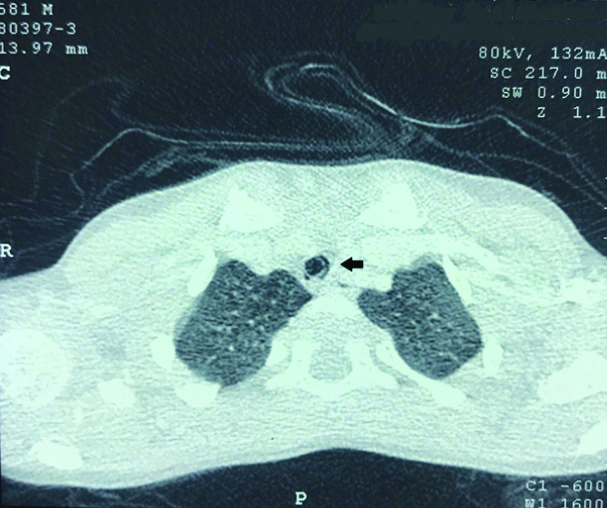
General physical examination was unremarkable. Chest was bilaterally clear with normal vesicular breathing and no added sounds. X-ray chest was clear [Table/Fig-1]. Finally, a CT scan was done which revealed a foreign body in the lower part of trachea just above the carina [Table/Fig-2].
Chest X-ray of the patent: normal.

CT Scan: Foreign body whistle in the trachea (dark arrow).
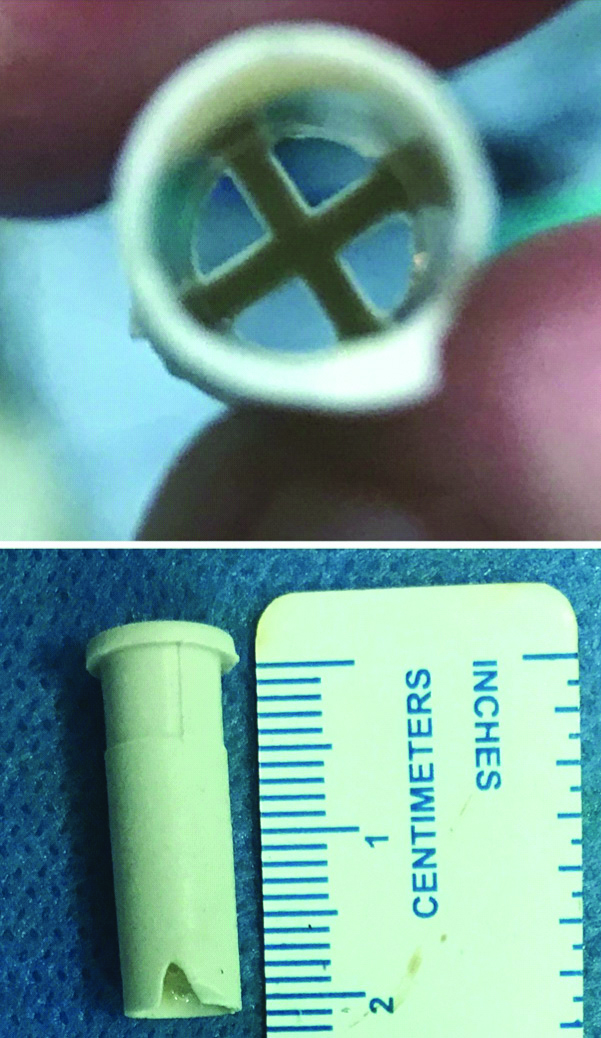
A detailed history was taken once again and now the child recalled that he had accidentally aspirated the whistle while blowing a “peepni” (Indian toy) with his friends about six months back. At that time patient had a severe bout of cough, which soon settled. Out of fear, the child did not discuss the incident with his parents. Subsequently, he developed cough, which at time did settle to medications, but soon cropped up again and again and was occasionally associated with wheeze. It was the fear of TB that prompted the parents to seek repeated medical advice for his cough ailment. Finally, the foreign body was removed by bronchoscopy under general anaesthesia with no untoward incident to report [Table/Fig-3]. The post-operative period was uneventful.
Whistle: hollow and fenestrated not causing respiratory obstruction.
This case has many interesting facets which warrant discussion. Firstly, this case report underlines the importance of CT in long standing inhalation of foreign body in children. Chest X-ray is an inconsistent investigation for diagnosis of foreign body in the aero-digestive tract [1]. Whereas, the literature reports a sensitivity and specificity of more than 94% and 97% respectively for CT scans [2,3]. However, the role of CT scan is not delineated in aspiration of foreign bodies- especially children with normal radiographs (like in this case) and the subject is open to debate. Nevertheless, the authors would like to emphasise that if a role for CT scan can be defined in cases of chronic cough, such rare and asymptomatic cases can be diagnosed early. Of note, cough is the most common symptom for long standing inhalation foreign bodies [4], but at present there are no specific clinical guidelines for CT scan in chronic cough. Chronic cough is defined as persistent cough for more than eight weeks [5]. Furthermore, in children, any cough extended beyond four weeks requires to be investigated [6,7].
In view of this clinical record, we believe that children with dry chronic cough and no clinical diagnosis should be investigated with CT scan immediately after four weeks, so that skepticism regarding inhalational and aspirated foreign bodies is duly resolved. In this context, it would be prudent to note that natural clinical course of missed foreign body is not benign. It can cause stricture, lung abscess, bronchiectasis, bronchopneumonia, infiltration and effusion [8].
Whistle is used for playing by all the kids. In India, it is a very common toy in rural area known as “Peepni”. However, it would be pertinent to note that it has a potential to become an asymptomatic foreign body, albeit rarely. Interestingly, in this case the child had no symptoms. As the whistle was hollow (i.e., fenestrated) & stuck in the lower part of trachea above the carina, proper ventilation was being maintained to both the lungs [Table/Fig-3]. No signs of emphysema or collapse of lungs were seen. We also did not record a wheeze, although the patient gave a history of occasional wheeze with a bout of cough.
There is not much in the literature on the subject of cough and whistle aspiration. Wang L et al., reported removal of whistle impacted in the bronchus for 14 years in an adult [9]. In a massive internet search at Medline/PubMed database using MeSH terms “whistle inhalation” and “children”, we could find only two paediatric cases with whistle inhalation reported since 1950 [6,7]. Both the cases were symptomatic and in only one case CT scan was required as X-ray chest were normal. In this case, tracheostomy was done to retrieve the foreign body. The age of the child was eight years. In contrast, the index case was totally asymptomatic (except for the cough) and was diagnosed accidentally on CT scan. Furthermore, we retrieved the foreign body by routine bronchoscopy with no complications whatsoever. This unique clinical presentation finds no mention in paediatric medical literature on the cited subject.
In summary, the rarity of the type of foreign body and its unusual clinical presentation make this case report unique and thus prompted us to share our professional experience with other members of our medical fraternity.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes (from guardian)
For any images presented appropriate consent has been obtained from the subjects. Yes (from guardian)
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Sep 11, 2019
Manual Googling: Sep 27, 2019
iThenticate Software: Oct 03, 2019 (7%)
[1]. Hitter A, Hullo E, Durand C, Righini CA, Diagnostic value of various investigations in children with suspected foreign body aspirationEur Ann Otorhinolaryngol Head Neck Dis 2011 128:248-52.10.1016/j.anorl.2010.12.01122018977 [Google Scholar] [CrossRef] [PubMed]
[2]. Liu YC, Zhou SH, Ling L, Value of helical computed tomography in the early diagnosis of esophageal foreign bodies in adultsAm J Emerg Med 2013 31:1328-32.10.1016/j.ajem.2013.05.04923896013 [Google Scholar] [CrossRef] [PubMed]
[3]. Manach Y, Pierrot S, Couloigner V, Ayari-Khalfallah S, Nicollas R, Venail F, Diagnostic performance of multidetector computed tomography for foreign body aspiration in childrenInt J Pediatr Otorhinolaryngol 2013 77:808-12.10.1016/j.ijporl.2013.02.01623489882 [Google Scholar] [CrossRef] [PubMed]
[4]. Martin A, van der Meer G, Blair D, Mahadevan M, Neeff M, Barber C, Long-standing inhaled foreign bodies in children: Characteristics and outcomeInt J Pediatr Otorhinolaryngol 2016 90:49-53.10.1016/j.ijporl.2016.08.01827729151 [Google Scholar] [CrossRef] [PubMed]
[5]. Irwin RS, Madison JM, The diagnosis and treatment of coughN Engl J Med 2000 343:1715-21.10.1056/NEJM20001207343230811106722 [Google Scholar] [CrossRef] [PubMed]
[6]. Kugelman A, Shaoul R, Goldsher M, Srugo I, Persistent cough and failure to thrive: a presentation of foreign body aspiration in a child with asthmaPediatrics 2006 117:e1057-60.10.1542/peds.2005-219616651284 [Google Scholar] [CrossRef] [PubMed]
[7]. de Jongste JC, Shields MD, Cough.2: Chronic cough in childrenThorax 2003 58:998-1003.10.1136/thorax.58.11.99814586058 [Google Scholar] [CrossRef] [PubMed]
[8]. Tang CL, Lee SC, Mohamad Lal A, Thomas RA, Ngui LX, Lim LY, Tracheotomy: an alternative for tracheobronchial foreign body removalMed J Malaysia 2014 69:241-43. [Google Scholar]
[9]. Wang L, Pudasaini B, Wang X-F, Diagnose of occult bronchial foreign body: A rare case report of undetected Chinese medicine aspiration for 10 long yearsMedicine (Baltimore) 2016 95:e407610.1097/MD.000000000000407627495017 [Google Scholar] [CrossRef] [PubMed]