Embryonal Rhabdomyosarcoma of Testis
Gunjan Bhatia1, Namita Goyal2
1 Senior Demonstrator, Department of Pathology, RNT Medical College, Udaipur, Rajasthan, India.
2 Associate Professor, Department of Pathology, RNT Medical College, Udaipur, Rajasthan, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Namita Goyal, 4, New Modern Complex, Bhuvana, Udaipur, Rajasthan, India.
E-mail: namitagoyal2007@rediffmail.com
Embroynal Rhabdomyosarcoma of the testis is a rare and aggressive tumour, mostly seen in children and young adults. It usually originates from the para testicular tissue. Intra testicular rhabdomyosarcoma of testis is a rare entity. The authors present a case of testicular rhabdomyosarcoma in a 28-year-old male patient. The patient presented to the surgical OPD with a painless scrotal mass of two months duration. A clinical diagnosis of testicular mass was made and patient was investigated and treated accordingly. Ultrasound (USG) revealed a right sided testicular mass measuring 16×6 cm. Patient underwent right sided inguinal orchidectomy. On microscopic examination tumour had varying degrees of cellularity, alternating densely packed hypercellular areas of oval to spindle shaped cells showing vesicular nucleus and pleomorphism along with loosely textured myxoid areas in between. IHC for keratin, Alpha-Fetoprotein (AFP), Inhibin and CD 117 were negative while Immunohistochemistry (IHC) for myogenin was positive. On basis of histopathology and IHC a final diagnosis of Embryonal Rhabdomyosarcoma was given. Intra testicular rhabdomyosarcoma of the testis is a rare tumour but should be kept in mind when dealing with a case of scrotal mass. Rarity of this entity makes it a strong learning point for our fellow clinicians and pathologists.
Aggressive tumour, Inguinal orchidectomy, Para testicular tissue
Case Report
A 28-year-old adult male patient presented to the Surgical OPD with a two months history of right sided testicular swelling which had rapidly increased in size since onset and was associated with a dragging sensation. On physical examination, there was a mass in the right scrotal region measuring 16×6 cm in size, firm to hard in consistency, regular in shape, non tender on palpation, mobile and not fixed to the scrotal skin. Right testis was not palpable separately. Other systemic examination was normal. There was no significant past history.
Patient was admitted with the clinical diagnosis of Testicular mass and a possibility of a malignant lesion was considered, all routine investigations were done. All investigations including tumour markers like Beta HCG and AFP were within normal limit. USG findings revealed a right testicular mass measuring 16×6.5 cm arising from the right testis. No evidence of any lymphnode or organomegaly was noted on USG. Chest X-ray was normal. MRI could not be done due to financial constraints.
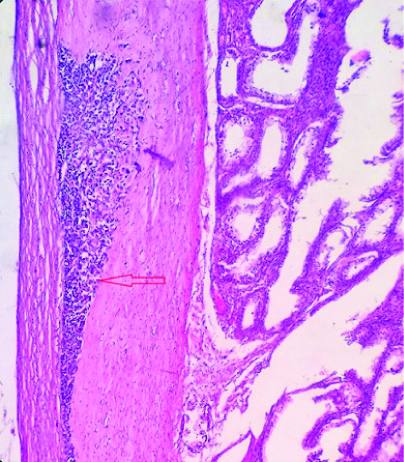
A right sided high inguinal orchidectomy was done and sample was sent for histopathology. On gross examination a grey white encapsulated soft tissue mass measuring 14.5×11.5×5 cm was noted [Table/Fig-1]. Cut section revealed homogenous grey white mass showing areas of myxoid degeneration replacing the normal testis and epididymis tissue completely. Attached cord measured 5.5 cm in length and normal spermatic cord was identified on cut section.
Gross specimen of the tumour: Grey white tumour mass with focal areas of myxoid degeneration. Normal testis and epididymis could not be identified separately.

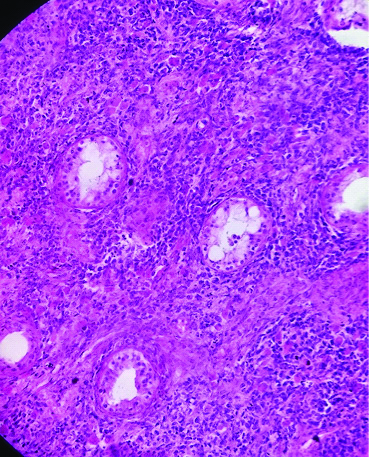
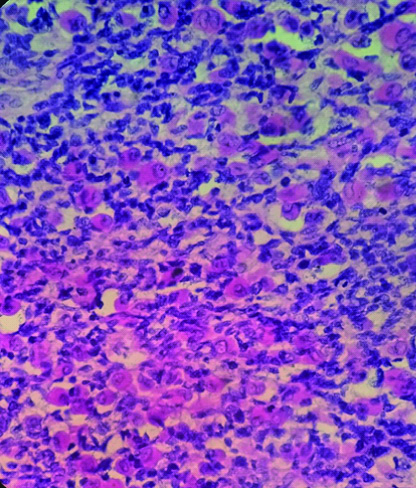
On microscopic examination, tumour had varying degrees of cellularity, alternating densely packed hypercellular areas of oval to spindle shaped cells showing vesicular nucleus and pleomorphism along with loosely textured myxoid areas in between [Table/Fig-2a]. Mitotic figures were frequently observed. At places sheets of rhabdomyoblasts having round hyperchromatic nucleus and brightly eosinophilic cytoplasm, several strap cells were also noted, few seminiferous tubules showing atrophic changes were also identified [Table/Fig-2b]. Tumour cells were infiltrating the tunica albugenia but not infiltrating tunica vaginalis and the cord cut margin was free from tumour [Table/Fig-2c]. Multiple sections from the spermatic cord at different levels did not show any evidence of tumour infiltration. Pathological staging of tumour was pT1NxMx.
Predominance of small primitive cells interspersed with more differentiated cells having rim of eosinophilic cytoplasm (rhabdomyoblast), (H&E,40X).
Few atrophic seminiferous tubules are noted with tumour cells in surrounding stroma (H&E, 200X).
Tumour infiltration in the tunica albuginea noted (H&E, 200X).
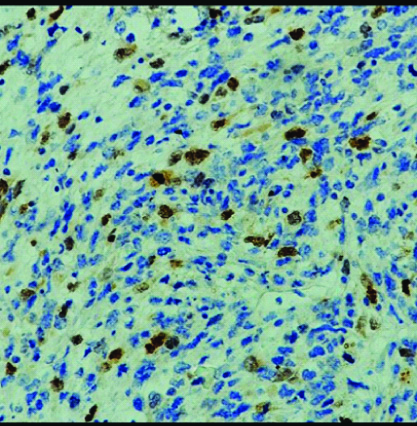
IHC for keratin, AFP, Inhibin and CD 117 were negative while IHC for myogenin was positive [Table/Fig-2d]. On basis of histopathology and IHC, a final diagnosis of well differentiated Embryonal Rhabdomyosarcoma was given. Patient was referred to oncology department and was given chemotherapy. At the time of submission the patient was doing well on chemotherapy.
IHC for Myogenin showing positive results (200X).
Discussion
Rhabdomyosracoma, is the most common soft tissue tumour occurring among children and adolescents with an annual incidence of 4-7 cases per million in children aged less than 15 years [1]. Embryonal Rhabdomyoscracoma of the testis is a rare and aggressive tumour of children and young adults [2]. It develops from the mesenchymal tissue of the spermatic cord, epididymis or the tunica vaginalis. Approximately 20% of all Rhabdomyosarcomas originate from the spermatic cord and paratesticular tissue. However Intra Testicular Rhabdomyosarcoma (ITRMS) of testis is a rare sarcoma of the testis. It develops rapidly and primarily presents as a painless scrotal mass of less than six months duration at the time of diagnosis. A radical orchidectomy followed by adjuvant chemotherapy is the currently recommended treatment for ITRMS. Though ITRMS presents as a painless scrotal mass more often, but it is not unusual to find evidence of distant metastasis at the time of initial diagnosis.
The majority of primary testicular tumours are of germ cell origin. Other rare origins of testicular tumours include lymphoma, gonadal stromal tumours and sarcomas. The incidence of rhabdomyosarcoma in testis and epididymis is 1 in 20 million males per year. Scrotal rhabdomyosarcomas primarily originate from paratesticular tissues and occur predominantly in children and adolescents. A 6% of all paratesticular tumours are embroynal rhabdomyosarcoma. Embryonal rhabdomyosarcoma is seen in all age groups but most commonly in children. An 80% of them occur before the age of 21 years. Testicular localisation of rhabdomyosarcoma is quite rare [3-10]. ITRMS is a rare tumour with an aggressive course. Embyronal rhabdomyosarcoma is the predominant histological subtype in 90% of testicular tumours and has a good prognosis if diagnosed early. Prognosis depends upon the age of patient, size of tumour, staging and rescetibility of tumour.
Myogenin is an important histochemical (IHC) marker which aids in confirmation of histological diagnosis. In our case IHC was positive for Myogenin. ITRMS is regarded as a highly malignant tumour with frequent recurrence. Spread of the tumour mostly occurs via lymphatics to the iliac and paraaortic lymphnodes [11]. Haematogenous metastases to lungs, liver and bone marrow are present in 20% of cases at time of presentation [12]. However, in our case there was no evidence of lymphadenopathy or organomegaly on USG at the time of diagnosis, also the margins were free of malignant cells. Unlike other germ cell tumours that develop in testis, tumour markers in ITRMS including Beta HCG, AFP and LDH were within normal range. USG remains the most important diagnostic modality for examining the testicular mass. Gross appearance and histopathology help in distinguishing ITRMS from paratesticular or spermatic cord rhabdomyosarcoma, while IHC confirms the diagnosis of rhabdomyosarcoma [13].
Though ITRMS is a rare tumour, clinicians and pathologists should be aware of this entity and it should be kept as one of the differential diagnosis in evaluating a scrotal mass. Multidisciplinary treatment is the key in dealing with cases of ITRMS. Our case underwent a right inguinal orchidectomy followed by chemotherapy and is doing well on follow-up.
Conclusion
Testicular rhabdomyosarcoma is a rare but aggressive tumour seen among young adults. Since this entity is quite rare in testis much is not known about the biological behaviour of this tumour. By picking up more of such cases we would be able to get a much better insight as to how this entity behaves which would help us in devising better treatment protocols.
Author Declaration:
Financial or Other Competing Interests: No
Was Ethics Committee Approval obtained for this study? NA
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 28, 2019
Manual Googling: Aug 02, 2019
iThenticate Software: Sep 30, 2019 (8%)
[1]. Dagher R, Helman L, Rhabdomyosarcoma: An overviewOncologist 1999 4:34-44. [Google Scholar]
[2]. Stewart LH, Lioe TF, Johnston SR, Thirty year review of intrascortal rhabdomyosarcomaBr J Urol 1991 68:418-20.10.1111/j.1464-410X.1991.tb15364.x1933165 [Google Scholar] [CrossRef] [PubMed]
[3]. Jun YI, Dong Zho U, Huo Ji, Yun Wang, Jin Ma, Primary intra testicular rhabdomyosarcoma. A case report and literature reviewOncol Lett 2016 11(2):1016-20.10.3892/ol.2015.398726893684 [Google Scholar] [CrossRef] [PubMed]
[4]. Liu ZW, Zhang XQ, Hou GL, Zhang ZL, Primary adult intratesticular rhabdo myosarcoma, results of treatment of six casesInt J Urol 2011 18:171-74.10.1111/j.1442-2042.2010.02685.x21272089 [Google Scholar] [CrossRef] [PubMed]
[5]. Kumar PV, Kazemi H, Khezri A, Testicular embryonal rhabdomyosarcoma diagnosed by fine needle aspiration cytologyHistopathology Acta Cytol 1994 38(4):573-76. [Google Scholar]
[6]. Banfield GK, Brookstein R, Rhabdomyosarcoma arising in teratoma of testisJ R Army Med Corps 1995 141:167-68.10.1136/jramc-141-03-078568751 [Google Scholar] [CrossRef] [PubMed]
[7]. Alexander F, Pure testicular rhabdomyosarcomaBr J Cancer 1968 22:498-501.10.1038/bjc.1968.585681010 [Google Scholar] [CrossRef] [PubMed]
[8]. Nasit JG, Parikh B, Trivedi P, Shah M, Primary intratesticular rhabdomyosarcoma in paediatricsIndian J Urol 2013 29:77-79.10.4103/0970-1591.10999523671375 [Google Scholar] [CrossRef] [PubMed]
[9]. Devi L P, Kumar P, Khonglah Y, Handique A, Advanced and recurrent testicular rhabdomyosarcoma in a young adult: A rare case reportClin Cancer Investig J 2015 4:428-30.10.4103/2278-0513.151943 [Google Scholar] [CrossRef]
[10]. Kelly B, Lundon D, Rowaiye B, Daly P, Embryonal rhabdomyosarcoma of the testisCan UrolAssoc J 2011 5:E7-E10.10.5489/cuaj.1004721470524 [Google Scholar] [CrossRef] [PubMed]
[11]. Shapiro E, Strother D, Pediatric genitourinary rhabdomyosarcomaJ Urol 1992 148:1761-68.10.1016/S0022-5347(17)37023-4 [Google Scholar] [CrossRef]
[12]. Demir A, Onol FF, Turkeri L, Paratesticular pleomorphic rhabdomyosarcoma in an adultInt Urol Nephrol 2004 36:577-78.10.1007/s11255-004-0853-x15787340 [Google Scholar] [CrossRef] [PubMed]
[13]. Shimamoto K, Tanji N, Ozaw A, Sasaki T, Intra scrotal rhabdomyosarcoma in an adult-A case reportNippon Hinyokika GakkaiZasshi 2009 100:545-49.10.5980/jpnjurol.100.54519514277 [Google Scholar] [CrossRef] [PubMed]