Avascular Necrosis of Femoral Head: A Retrospective Study of MRI Scans
Prateek Singh Gehlot1, Kajal Agrawal2, Ritema Mangal3, Varsha Sodani4
1 Associate Professor, Department of Radiology, R.D. Gardi Medical College, Ujjain, Madhya Pradesh, India.
2 Senior Resident, Department of Radiology, R.D. Gardi Medical College, Ujjain, Madhya Pradesh, India.
3 Assistant Professor, Department of Radiology, R.D. Gardi Medical College, Ujjain, Madhya Pradesh, India.
4 Postgraduate Student, Department of Radiodiagnosis, R.D. Gardi Medical College, Ujjain, Madhya Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Prateek Singh Gehlot, B-5/18, R.D. Gardi Medical College Campus, Surasa, Ujjain, Madhya Pradesh, India.
E-mail: prateekgehlot@yahoo.com
Introduction
Avascular necrosis of the femoral head is commonly encountered now-a-days with increasing use of steroids and alcohol. MRI is considered the most effective diagnostic investigation for avascular necrosis and is helpful for screening and detecting at early stage.
Aim
The aim of the study was to determine the prevalence pattern and stages of presentation of Avascular Necrosis (AVN) of the femoral head.
Materials and Methods
This was a retrospective study carried out at the Department of Radio-diagnosis in which MRI of the hip joint was performed during our study period, only those patients which showed positive signs for avascular necrosis of femoral head were included and were analysed over a period of seven years. The age, sex, laterally distribution, causative factors, staging according to Ficat and Arlet classification was done.
Results
It was found that most commonly males of productive age group (21 to 40 years) were affected. Most of them had bilateral involvement however the involvement of left and right hip joint was nearly the same. Mostly, patient presented with stage-III disease accounting for 81 patients.
Conclusion
Considering that the young males were commonly affected and presented with advanced stage disease it was recommended that screening MRI should be done in all patients presenting with hip complaints especially males of productive age group.
Ficat and arlet staging, Osteonecrosis
Introduction
AVN of the femoral head is a common hip pathology, causing severe musculoskeletal disability. It is also a common cause for the hip replacements, these days. Hence, the efforts are increasingly being made for its early detection and, various imaging techniques were assessed time to time. Although, assessment of hip joint begins with clinical evaluation including careful physical examination, imaging is fundamental for accurate diagnosis and staging of AVN. The young adults mainly the men are affected in their third and fifth decade of life [1].
Avascular necrosis occurs in femoral head as it has single terminal blood supply from epiphyseal arteries that traverse from the femoral neck to supply the head. These arteries can be interrupted from trauma, can get blocked from thrombi/embolism or may be externally compressed. The potential causes that predisposes to osteonecrosis are long term steroids use, alcoholism, immunosuppression, trauma causing femoral head and neck fractures, hip dislocation, inflammatory diseases like pancreatitis, connective tissue disease, rheumatoid arthritis, radiation therapy and haematological disorders like sickle cell anaemia, haemophilia, polycythemiarubravera and metabolic and endocrine disorders like pregnancy, diabetes, Cushing’s syndrome, Gaucher’s disease, etc., [1].
Radiograph of hip is usually the first investigation done in a case of suspected AVN, but unfortunately, plain radiographs are unremarkable in early stages of AVN. MRI is the most sensitive means of diagnosing AVN. This imaging modality provides the criterion standard of non-invasive diagnostic evaluation and is more sensitive than CT scanning or bone scans [2]. MRI is the investigation of choice for the accurate staging of AVN, because images clearly depict the size of the lesion, and gross estimates of the stage of disease can be made. CT is basically done to evaluate extent of disease and to confirm subchondral or cancellous fractures or collapse. SPECT scanning has a role in assessing the radioactivity of the organ and it is useful in early cases to detect the avascular focus that can be missed with routine MRI sequences without contrast. Bone scanning can be performed in cases where MRI is contra-indicated or equivocal, and it helps to quantify the physiologic data i.e., uptake in static and perfusion states. Bone biopsy is accurate, and can establish early diagnosis, however, generally avoided as it is invasive. The aim of the study was to determine the prevalence pattern and stages of presentation of Avascular Necrosis (AVN) of the femoral head.
Materials and Methods
The study was carried out at the Department of Radio-diagnosis, R.D. Gardi Medical College and C.R. Gardi Hospital, Ujjain M.P. mainly serving the rural population of Malwa region during a period of seven years “from January 2011 to December 2017. MRI examination of one hundred and eighty-six patients of avascular necrosis of femoral head were analysed retrospectively”. The study was conducted after the approval of the institutional ethical committee with IEC reference number-IEC-RDGMC55A/2019.
All the patients showing signs of avascular necrosis of femur on MRI, from all age groups and both sexes were included in the study. All the patients with post-operative implants, other associated hip joint pathologies and trauma were excluded from the study. The MRI scans were performed on a 1.5 TGE HDE Scanner using T1 Weighted spin echo (T1W) sequence in the axial and the coronal plane, the T2 weighted fast spine echo (T2W) sequence in the axial plane, the Short Tau Inversion Recovery (STIR) sequence in the coronal and the axial planes and Gradient echo sequence (GRE) in the sagittal plane. The various well-known manifestations of AVN like bone marrow oedema, joint effusion, flattening of femoral head, narrowing of joint space, marginal irregularity, collapse of head, subchondral fracture and double line sign were seen on various MRI sequences, especially in coronal plane. These appearances of the lesion over the various sequences of MRI were used as the criteria for diagnosing and staging of AVN [Table/Fig-1,2,3 and 4]. The Ficat and Arlet classification of avascular necrosis was used to stage the patients. Ficat and Arlet have developed a staging system using radiographic findings, consisting of four stages. Hungerford and Lennox modified this staging system when MRI became available, adding stage 0 to the classification and now the system currently uses a combination of plain radiographs, MRI and clinical features to stage avascular necrosis of the femoral head [3-4].
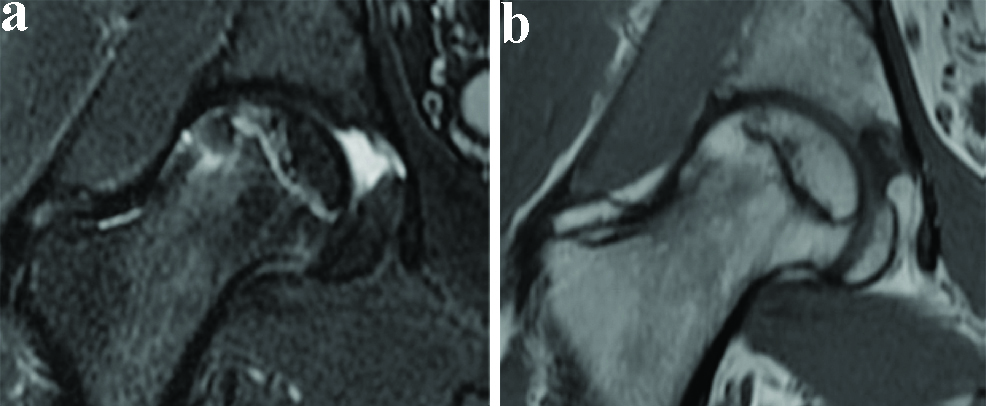
AVN Stage-I Coronal STIR (a) and T1W (b) sequence of right hip joint shows a band of hypointensity on T1W sequence in head with preserved fat signal in subchondral portion of head of femur and minimal marrow oedema. Normal appearing acetabulum.
a: Coronal stir sequence. b: Coronal T1W sequence
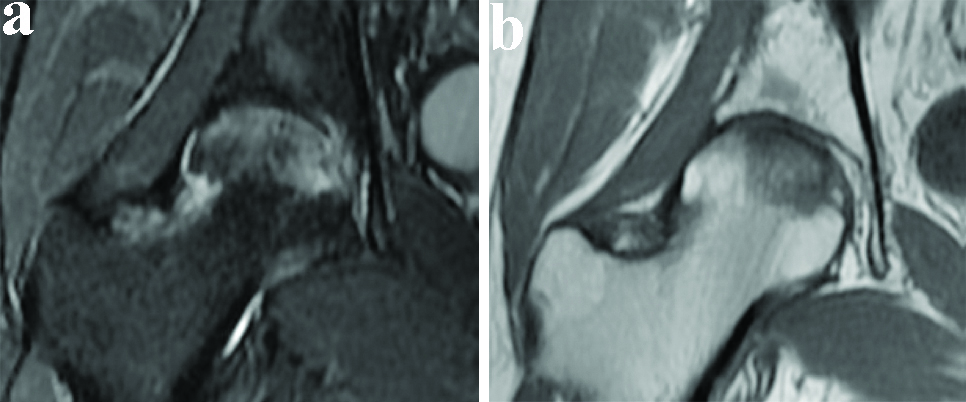
AVN Stage-II Coronal STIR (a) and T1W (b) sequence of right hip joint shows awedge-shaped area of hypointensity on T1W sequence in head with patchily lost fat signal of head of femur and marrow oedema. Normal appearing acetabulum.
a: Coronal stir sequence. b: Coronal T1W sequence
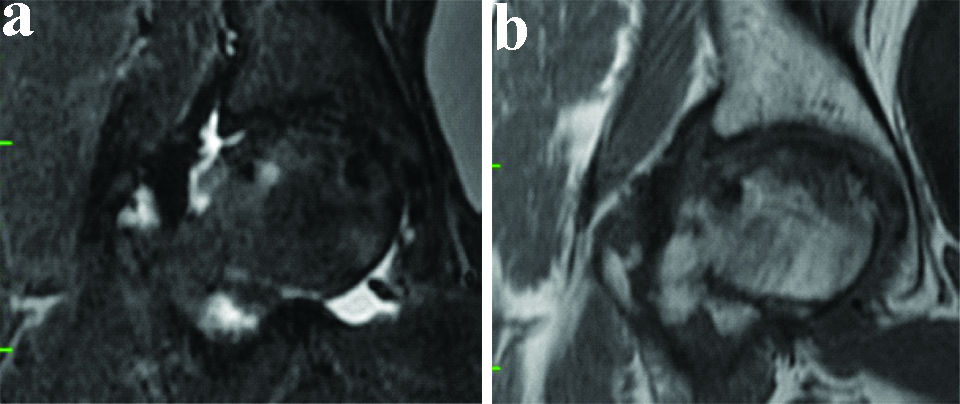
AVN Stage-III Coronal STIR (a) and T1W (b) sequence of right hip joint shows altered shape of head of femur with subchondral collapse, small fragmentation and flattening, irregularity of articular surface of head sclerosis, loss of fat signal and reduced joint space. Normal appearing acetabulum.
a: Coronal stir sequence. b: Coronal T1W sequence
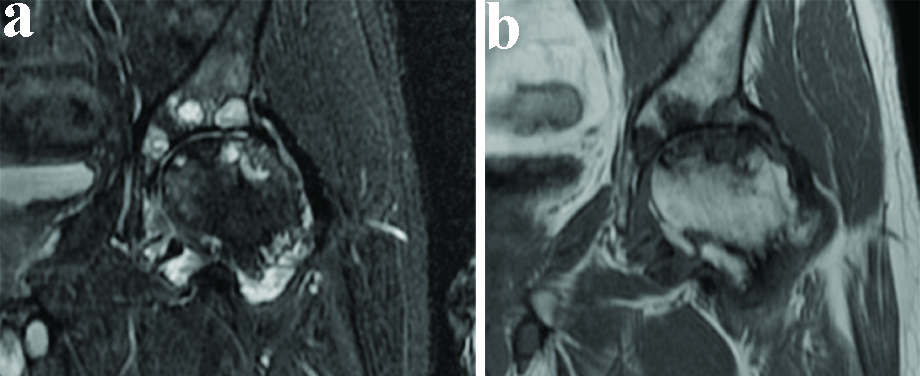
AVN Stage-IV Coronal STIR (a) and T1W (b) sequence of left hip joint shows significantly altered shape of head of femur with subchondral collapse, fragmentation and flattening, irregularity of articular surface of head, sclerosis, loss of fat signal and lost joint space with absent cartilage. Irregularity of articular surface of acetabulum with focal subchondraloedema and cyst formation.
a: Coronal stir sequence. b: Coronal T1W sequence
According to this classification there are five stages of AVN of femoral head, however, in stage zero the MRI findings were normal, hence, the cases were staged from stage I to stage IV considering the MRI findings. The Ficat classification system in its last two stages (III and IV) describe the changes that occur after the femoral head collapse [5-7].
Results
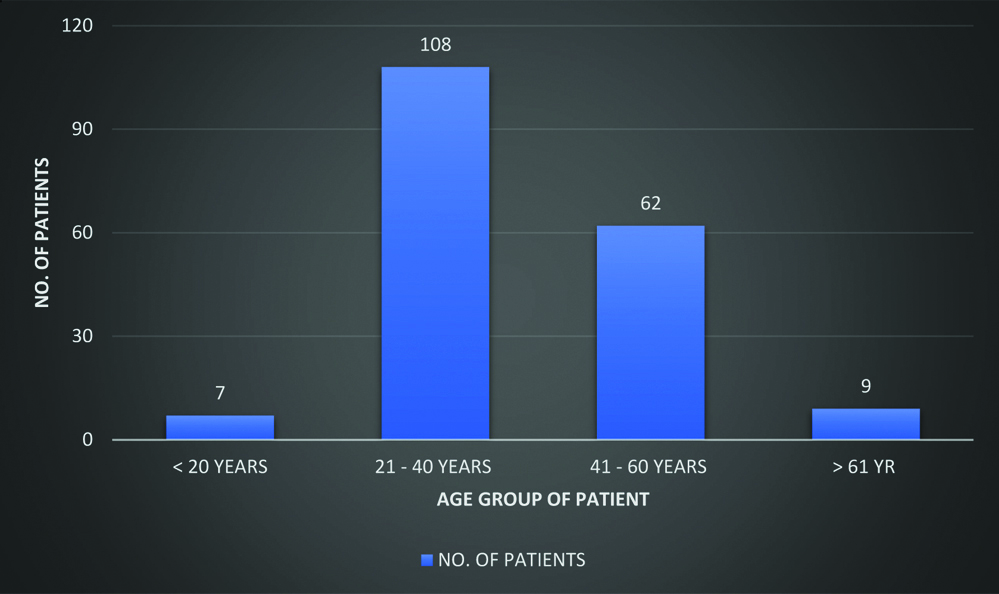
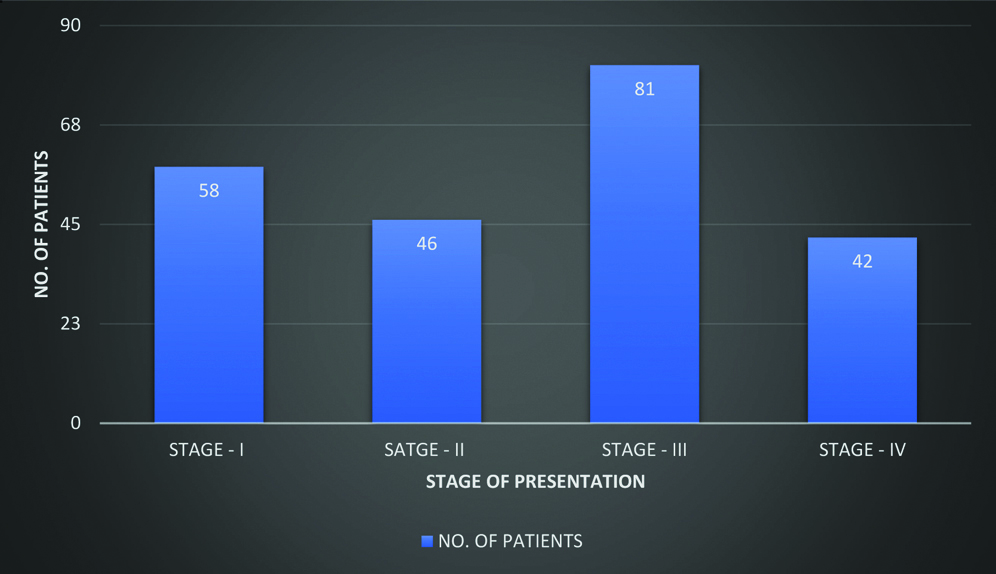
Total 186 patients were included in this study, out of which, the highest number of patients were seen in the economically productive age group of 21 to 40 years [Table/Fig-5]. A clear-cut male predominance was noted, as out of the 186 patients, one sixty (86%) patients were males and twenty-six (14%) were females. Also, a predominant bilateral involvement of hip joint was seen in one thirty-eight (74%) and forty-eight (26%) had unilateral hip involvement. As far as laterality is considered in unilateral cases, mild difference is seen as twenty-six (54%) had right sided involvement and twenty-two (46%) had left sided involvement. Most of the patients came for MRI after an advanced stage, in which out of the 186 total patients, 81 had stage-III disease at the time of diagnosis [Table/Fig-6]. On comparing male and female involvement in various age-groups with stage of presentation [Table/Fig-7], it has been observed that males are predominantly affected in all age-groups with stage-I commonest in 20 and less than 20 years of age, stage-III commonest in age group 21 to 40 years and 41 to 60 years of age and stage-III and IV being equally involved in age group of 61 and above years.
Age distribution of cases of avascular necrosis of femoral head.
Stage of presentation, according to Ficat and Arlet classification system.
Comparison of sex distribution with stage of presentation and age group of the patients.
| Age group | Stages | Males | Females |
|---|
| Less than 20 years | STAGE-I | 3 | 1 |
| STAGE-II | NIL | NIL |
| STAGE-III | 2 | 2 |
| STAGE-IV | NIL | 2 |
| 21-40 years | STAGE-I | 26 | 4 |
| STAGE-II | 25 | 1 |
| STAGE-III | 39 | 8 |
| STAGE-IV | 30 | 10 |
| 41-60 years | STAGE-I | 20 | 1 |
| STAGE-II | 15 | 2 |
| STAGE-III | 26 | nil |
| STAGE-IV | 22 | nil |
| 61 and above years | STAGE-I | 1 | 2 |
| STAGE-II | 1 | NIL |
| STAGE-III | 2 | NIL |
| STAGE-IV | 2 | 4 |
*During this comparison both left and right-sided hip joint of each patient are considered separately, as they may show different stages at a given time.
During the study, two patients had early AVN changes, however the lesions were not qualifying correctly for the Stage-I description of the Ficat and Arlet Classification, and hence these 2 cases were excluded from the study, and finally 186 patients were included in the study.
Also, three patients had follow-up scans after hip replacement, and only their follow-up scans were excluded from the study. Patients having history of trauma to hip joints resulting in fractures were also excluded from the study.
Discussion
The major cause for AVN of hip still remains unknown but now-a-days we observed a significant increase in the prevalence of the well-known causative factors for AVN like increased alcohol consumption in males and increased contraceptive use in females. Its occurrence in relatively younger age which leads to significant stress on health system and decrease in financial and social productivity of the individual. It causes irreversible damage to the joint which requires a replacement of joint in future depending on the stage of disease and degenerative consequences. An early detection of disease carries lot of significance since corrective measures and removal of causative factors can limit the size of lesion and severity of disease, thus delaying the joint replacement and improving the quality of life.
In our study, we found that AVN pre-dominantly affected the younger adults with highest number of patients (108) seen in the age-group of 21 to 40 years, followed by 62 patients in 41-60 years. These findings were consistent with the study conducted by Khaladkar MS et al., in which the age group varied from 11 to 70 years. Maximum belonged to age group 31-40 (30.5%), followed by 21-30 (25%) and 41-50 (22.2%). However, as far as the sex prevalence is considered our results opposes the result of the study by Khaladkar MS et al., in which out of 36 cases of AVN, 32 (88.88%) were males and 4 (11.11%) were females but we found a clear-cut male predominance as out of the 186 patients, one sixty (86%) patients were males and twenty-six (14%) were females. Similar results were also found on comparing the bilateral and hip involvement which was 22 patients (61.1%) in the study conducted by Khaladkar MS et al., and one thirty-eight (74%). They also found that out of 58 hips, left hip was involved in 33 cases (56.8%) and right hip was involved in 25 (43.1%), however in our study we observed twenty-six (54%) had right sided involvement and twenty-two (46%) had left sided involvement [8].
We also observed that people usually opt for MRI at the advanced stage of disease even when the symptoms were present for years as stage-III was the commonest stage found. Also, the treatment options available at higher stages of disease like hip replacement surgeries are costly and lead to financial constraints. MRI being multi-planner was able to show the extent of involvement of weight-bearing area and total involvement of head of femur which is helpful in predicting the prognosis of AVN. The T1W and STIR sequences in coronal plane were found to be extremely helpful for quick and clear review of both the hip joints and should be incorporated in short screening protocols for the suspected patients of AVN, which will reduce the cost and time of the investigation without compromising patient care.
Since joint preserving measures have much better prognosis when diagnosis of AVN is made in early course of disease and since result of joint replacement therapy are poorer in young age groups, diagnosis of AVN as early as possible is critical to prevent or delay progression of disease. MRI is excellent for picking up early AVN changes that are far beyond to be seen on plain radiographs. Also, all the well-known manifestations of AVN can be well appreciated on MRI.
Limitation
The only limitation we found in our study was that while analysing the scans we could have quantified the extent of the femoral head involvement through which we can predict the prognosis of the patient.
Conclusion
MRI can detect early AVN changes in asymptomatic patients which is necessary because early diagnosis is critical to prevent or delay progression of disease hence, it should be the investigation of choice for screening the patients who are at great risk for development of AVN. Awareness and education regarding early diagnosis and possible prevention and delay in progression of disease by MRI evaluation should be promoted as it has long term advantages in terms of health of the individual and on health care system.
*During this comparison both left and right-sided hip joint of each patient are considered separately, as they may show different stages at a given time.
Author Declaration:
Financial or Other Competing Interests: No
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? No
For any images presented appropriate consent has been obtained from the subjects. No
PLAGIARISM CHECKING METHODS: [Jain H et al.]
Plagiarism X-checker: Jan 14, 2019
Manual Googling: Jul 12, 2019
iThenticate Software: Sep 28, 2019 (13%)
[1]. Kamal D, Trăistaru R, Alexandru DO, Grecu DC, Mogoanta L, Epidemiologic study of avascular necrosis of the femoral headCurrent Health Sciences Journal 2013 39(3):169-74. [Google Scholar]
[2]. Aiello MR, Imaging in avascular necrosis of the femoral head guidelinesMedscape 2017 [Google Scholar]
[3]. Orban HB, Cristescu V, Dragusanu M, Avascular necrosis of the femoral headMAEDICA- A Journal of Clinical Medicine 2009 4(1):26-34. [Google Scholar]
[4]. Aldridge JM 3rd, Urbaniak JR, Avascular necrosis of the femoral head: etiology, pathophysiology, classification, and current treatment guidelinesAm J Orthop 2004 33(7):327-32. [Google Scholar]
[5]. Kamal DI, Alexandru DO, Kamal CK, Streba CT, Grecu D, Mogoantă L, Macroscopic and microscopic findings in avascular necrosis of the femoral headRom J Morphol Embryol 2012 53(3):557-61. [Google Scholar]
[6]. Mont MA, Marulanda GA, Jones LC, Saleh KJ, Gordon N, Hungerford DS, Systematic analysis of classification systems for osteonecrosis of the femoral headJ Bone Joint Surg Am 2006 88(Suppl 3):16-26.10.2106/00004623-200611001-00004 [Google Scholar] [CrossRef]
[7]. Stark DD, Bradley WG, Magnetic Resonance Imaging3rd edMosby; Chapter 44, Ischemic necrosis:1044-45. [Google Scholar]
[8]. Khaladkar MS, Randhawa S, Singh G, Aditi G, Rajesh K, Rajeshwar S, Rapid magnetic resonance imaging protocol for detecting femoral head avascular necrosis: A case series-it’s utility in the general population in developing countriesMedical Journal of Dr. DY Patil University 2015 8(2):18910.4103/0975-2870.153156 [Google Scholar] [CrossRef]