Giant Periosteal Chondroma: Report of a Rare Case
Amritha Kesavan1, Divya Surendran2, Joy Augustine3, Dominic K Puthoor4, Dijoe Davis5
1 Junior Resident, Department of Pathology, Amala Institute of Medical Sciences, Thrissur, Kerala, India.
2 Associate Professor, Department of Pathology, Amala Institute of Medical Sciences, Thrissur, Kerala, India.
3 Professor and Head, Department of Pathology, Amala Institute of Medical Sciences, Thrissur, Kerala, India.
4 Professor, Department of Orthopaedics, Amala Institute of Medical Sciences, Thrissur, Kerala, India.
5 Associate Professor, Department of Orthopaedics, Amala Institute of Medical Sciences, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Amritha Kesavan, 9E, Cheloor Platinum Heights, Pipeline Road, Mylipadam, P.O. Chembukkavu, Thrissur-680020, Kerala, India.
E-mail: amritha90k@gmail.com
Periosteal chondromas are uncommon benign cartilaginous neoplasms which account for <2% of all bone tumours. They are rarely >5 cm in greatest diameter with an average size of 3 cm, with proximal humerus being a characteristic location. Large periosteal chondromas are very rare. Clinically, they present as palpable often painful masses. Radiographically, they appear as radiolucent bone surface tumours that form sharply marginated erosions (“saucerisation”) of the cortex and are well demarcated from the underlying medullary cavity by a thin rim of sclerosis. Histologically, these tumours are well circumscribed, and are characterised by lobules of cartilage with benign clusters of chondrocytes that do not have a permeative growth pattern. Occasionally, these tumours can be more cellular showing nuclear pleomorphism and binucleation, which can be misdiagnosed as chondrosarcoma. Periosteal chondromas are treated with en-bloc excisions. This case report describes a case of giant periosteal chondroma of proximal humerus.
Bone neoplasm, Chondroma, Humerus
Case Report
A 15-year-old boy presented to the Department of Orthopaedics with chief complaint of swelling of the left shoulder of 6 months duration. The swelling was gradually increasing in size. There was dull aching pain on deep pressure. On examination, the swelling was 8 cm × 6 cm in size, firm, well defined and there was tenderness on deep palpation. The X-ray showed an eccentric expansile cortical lytic lesion involving the lateral aspect of the proximal humerus with “ring and arc” matrix calcification [Table/Fig-1]. The lesion showed a narrow zone of transition with the surrounding bone and a well-defined margin with the adjacent soft tissue. Contrast enhanced MRI showed a heterogeneously enhancing lesion with predominant soft tissue component arising from the periosteum of the meta-diaphysial region of the proximal third of the left humerus. The provisional diagnoses considered based on the clinical and radiological findings were conventional osteosarcoma, periosteal osteosarcoma, periosteal chondroma and osteochondroma.
X-ray showing eccentric expansile cortical lytic lesion with “ring and arc” like internal calcifications.

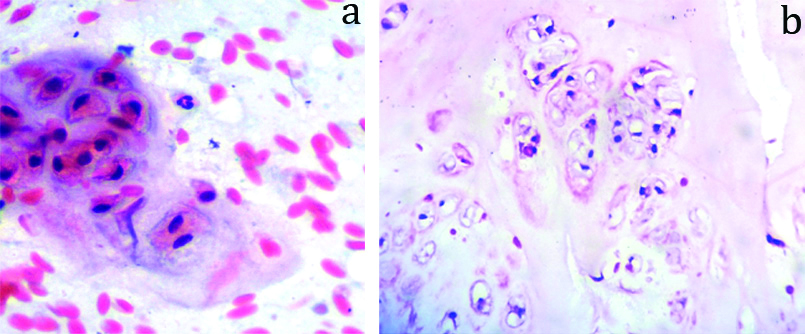
CT guided trucut biopsy was done from the lesion and imprints were taken from the biopsy sample. The imprint cytology showed benign chondrocytes suggestive of a benign chondroid neoplasm [Table/Fig-2a]. Trucut biopsy showed lobules of chondrocytes with uniform nuclei. No permeation into the bony trabeculae was noted [Table/Fig-2b]. Based on trucut biopsy findings, a diagnosis of chondroid neoplasm was made.
a) Imprint cytology showing chondrocytes with moderate amount of cytoplasm and uniform nuclei. (H&E, 40x). b) Trucut biopsy section showing chondrocytes with uniform nuclei. (H&E, 40x).
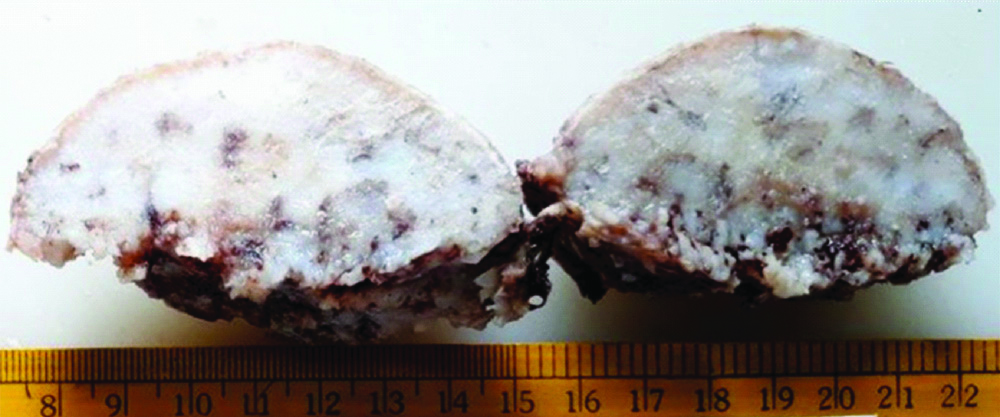
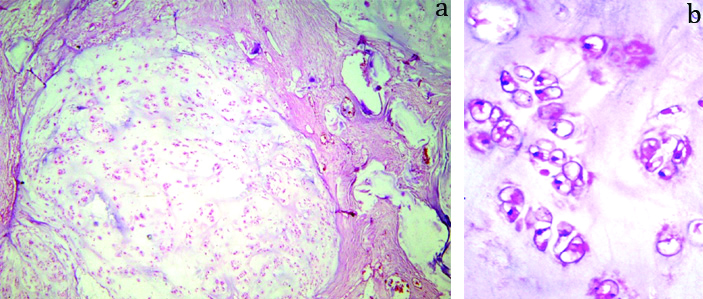
Excisional biopsy specimen showed a smooth, circumscribed, partially encapsulated neoplasm measuring 8 cm×6 cm×4 cm, the cut section of which was predominantly cartilaginous [Table/Fig-3]. Microscopy showed a circumscribed chondroid neoplasm arranged in lobules separated by fibrous septae. Lobules showed moderate cellularity with chondrocytes within the lacunae [Table/Fig-4a,b]. Nuclear pleomorphism, increased cellularity, mitotic activity and necrosis were absent. Endochondral ossification was noted. Considering the radiological and histopathological features, a final diagnosis of periosteal chondroma was made. Local excision with curettage was done. Postoperative period was uneventful. An X-ray, taken 6 months post surgery, showed no evidence of residual neoplasm. Patient is on regular follow-up and is doing well without any recurrence radiologically.
Partially encapsulated neoplasm with predominant grey white glistening cartilaginous areas.
Excisional biopsy section showing Circumscribed chondroid neoplasm arranged in lobules with moderate cellularity. (a- H&E, 10x) (b- H&E, 40x).
Discussion
Periosteal chondroma is an uncommon (<2%) benign hyaline cartilaginous neoplasm of the bone surface that arises from the periosteum. It was first described by Keiller VH [1]. He observed a benign cartilage tumour of the toe in a 20-year-old man and named it as subperiosteal epiphyseal chondroma. Following this, six cases of periosteal chondroma were reported by Lichtenstein L and Hall JE, [2]. The second series of tumour consisting of nine cases were described by Jaffe HL [3].
Periosteal chondroma is a slow growing tumour. Most cases occur in the second and third decades of life with the highest frequency between 10 and 20 years. It occurs in children and young adults with a predilection for males [4-6]. It accounts for <2% of bone tumours. This case is being presented owing to the large size of the tumour and since the authors believe that this is one of the largest periosteal chondromas reported in the literature to date.
Periosteal chondromas commonly occur in the long bones with proximal humerus being a characteristic location. Small tubular bones are the other sites. In the present case, the tumour was located in the proximal humerus. They usually arise from the metaphysis or metadiaphysis [7]. These tumours are rarely greater than 5 cm in greatest diameter with an average size of 3 cm [8]. A few case reports have cited a larger tumour size. Imura Y et al., reported a giant periosteal chondroma (9 cm) of the femur [9]. The tumour in the present case was 8 cm in maximum dimension. The cells of the periosteum, rather than the physis, appear to be the source for periosteal chondroma [10].
Clinically they present as palpable often painful masses. Radiologically, they are radiolucent bone surface tumours forming sharply marginated erosion of the cortex. Scalloping or remodelling of the adjacent bony cortex, cartilaginous matrix with ringlets of calcification, and a possible soft tissue mass component form the main radiographic features of this lesion [11-13].
Grossly, they present as hyaline cartilaginous masses with variable calcification. Microscopy shows lobules of hyaline cartilage within well-formed lacunae which is covered by a fibrous periosteal capsule [4,14].
In this case, the imaging features were suggestive of periosteal chondroma with an unlikely differential diagnosis of periosteal osteogenic sarcoma. Periosteal chondrosarcoma is another important tumour to be distinguished from periosteal chondroma. They also present as slow growing malignancies. Radiologically, they may show sclerosis and scalloping similar to periosteal chondromas. However, periosteal chondrosarcomas are generally larger in size and does not occur in the younger age group.
Radiologically, the margins of periosteal chondrosarcomas are indistinct. They tend to permeate the underlying bone with formation of bony spicules extending out from the cortex [15,16]. The mean tumour size in periosteal chondrosarcomas is usually more than 5 cm in size. Mankapure PK et al., mentions that chondroma has regular lobulation pattern with an almost inactive fibrous capsule which has less vascularity as compared to chondrosarcoma which has an irregular, asymmetrical lobulation pattern with increased blood vessels in the fibrous capsule [4]. Other differential diagnoses include periosteal osteosarcoma, aneurysmal bone cyst, sub-periosteal haemangioma, sub-periosteal ganglion and chondromyxoid fibroma [17,18].
Periosteal osteosarcomas arise beneath the periosteum as slow growing masses. They occur as radiolucent lesions on the surface of bone with perpendicular striae and peripheral Codman’s triangle. Histological appearance is characterised by chondroid areas with anaplastic features, and may show lace like malignant osteoid [19]. Osteochondroma was considered as a differential diagnosis in this case based on the clinical and radiological features. Most of the osteochondromas occur in the long bones of adolescents, particularly distal femur and proximal tibia and present as an irregular bony masses with a cartilaginous cap. Microscopically, they resemble a normal growth plate with vertical rows of chondrocytes as they show endochondral ossification on the basal surface of hyaline cartilage [19,20]. Chondromyxoid fibroma, which is the least common benign cartilaginous tumour of bone, can also occur as surface lesion, long bones being a common site. Classic chondromyxoid fibroma is characterised by lobules of stellate or spindle shaped cells in a chondromyxoid background. Periphery of the lobules shows increased neoplastic cells. Fibrous bands containing blood vessels and occasionally multinucleated giant cells separate the lobules [21].
Histopathological examination helps to confirm the diagnosis. Histologically periosteal chondromas are well demarcated from the underlying cortex. Sometimes erosion and scalloping of cortex can occur, but they do not penetrate into the cancellous bone. Cellularity and cytological features are similar to other chondromas. Occasionally, they show greater nuclear pleomorphism and more binucleation. Nojima T et al., reported a series of 46 patients with periosteal chondroma in which increased cellularity, hyperchromasia, nucleomegaly, binucleation or myxoid change of the matrix was present in 33 cases [8]. Immunohistochemically S-100 will show positivity. Clonal karyotypic abnormalities have been described in very few cases.
Periosteal chondromas are treated with intralesional, marginal and en-bloc excisions. Recurrence rate is low in marginal and en-bloc excisions compared to intralesional curettings [7,22].
Conclusion
A benign nature of chondroid tumours is difficult to establish. It requires a combination of clinical data, radiological imaging and histopathological examination of the lesion. Authors believe that this case is one of the largest periosteal chondromas reported in the literature to date. Further, the case report highlights the importance of histopathology and radiology in arriving at the correct diagnosis.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Not Required
For any images presented appropriate consent has been obtained from the subjects. Not Required
PLAGIARISM CHECKING METHODS: [Jain H et al.]
Plagiarism X-checker: Jun 29, 2019
Manual Googling: Sep 06, 2019
iThenticate Software: Sep 28, 2019 (12%)
[1]. Keiller VH, Cartilaginous tumours of boneSurg Gynecol Obstet 1925 40:510 [Google Scholar]
[2]. Lichtenstein L, Hall JE, Periosteal chondroma; a distinctive benign cartilage tumourJ Bone Joint Surg Am 1952 24-A-3:691-97.10.2106/00004623-195234030-00026 [Google Scholar] [CrossRef]
[3]. Jaffe HL, Juxtacortical chondromaBull. Hosp. Joint Dis 1956 17:20-29. [Google Scholar]
[4]. Mankapure PK, Barpande SR, Bhavthankar JD, Periosteal chondroma of mandible: report of a case and differential diagnosisOral Maxillofac Pathol J 2014 5(2):498-502. [Google Scholar]
[5]. Boriani S, Bacchini P, Bertoni F, Campanacci M, Periosteal chondroma. A review of twenty casesJ Bone Joint Surg Am 1983 65(2):205-12.10.2106/00004623-198365020-000096822582 [Google Scholar] [CrossRef] [PubMed]
[6]. Zhang Y, Yu MY, Li DY, Zhao DW, Periosteal chondroma of the scapula penetrating into both the anterior and posterior cortices: a case reportInt J Clin Exp Med 2018 11(8):8704-07. [Google Scholar]
[7]. Ricca RL, Kuklo TR, Shawen SB, Vick DJ, Schaefer RA, Periosteal chondroma of the cuboid presenting in a 7-year-old boyFoot & Ankle International 2000 21(2):145-49.10.1177/107110070002100209 [Google Scholar] [CrossRef]
[8]. Nojima T, Unni KK, Mcleod RA, Pritchard DJ, Periosteal chondroma and periosteal chondrosarcomaAm J Surg Pathol 1985 9(9):666-77.10.1097/00000478-198509000-000064051099 [Google Scholar] [CrossRef] [PubMed]
[9]. Imura Y, Shigi A, Outani H, Hamada K, Tamura H, Morii E, A giant periosteal chondroma of the distal femur successfully reconstructed with synthetic bone grafts and a bioresorbable plate: a case reportWorld J Surg Oncol 2014 12:35410.1186/1477-7819-12-35425416085 [Google Scholar] [CrossRef] [PubMed]
[10]. Brien EW, Mirra JM, Luck JV Jr, Benign and malignant cartilage tumours of bone and joint: their anatomic and theoretical basis with an emphasis on radiology, pathology and clinical biology. II. Juxtacortical cartilage tumoursSkeletal Radiol 1999 28(1):01-20.10.1007/s00256005046610068070 [Google Scholar] [CrossRef] [PubMed]
[11]. Robinson P, White LM, Sundaram M, Kandel R, Wunder J, McDonald DJ, Periosteal chondroid tumours: radiologic evaluation with pathologic correlationAJR Am J Roentgenol 2001 177(5):1183-88.10.2214/ajr.177.5.177118311641198 [Google Scholar] [CrossRef] [PubMed]
[12]. DeSantos LA, Spjut HJ, Periosteal chondroma: a radiographic spectrumSkeletal Radiol 1981 6(1):15-20.10.1007/BF003473416936836 [Google Scholar] [CrossRef] [PubMed]
[13]. Woertler K, Blasius S, Brinkschmidt C, Hillmann A, Link TM, Heindel W, Periosteal chondroma: MR characteristicsJ Comput Assist Tomogr 2001 25(3):425-30.10.1097/00004728-200105000-0001611351194 [Google Scholar] [CrossRef] [PubMed]
[14]. Liu Z, Yan W, Zhang L, Li Q, Periosteal chondroma of the proximal tibia: report of three casesInt J Clin Exp Med 2016 9(6):9908-16. [Google Scholar]
[15]. Nguyen TP, Burk DL Jr, Musculoskeletal case of the day. Giant cell tumour of the sacrumAJR Am J Roentgenol 1995 165(1):201-02.10.2214/ajr.165.1.77855967785596 [Google Scholar] [CrossRef] [PubMed]
[16]. Singh AP, Singh AP, Mahajan S, Periosteal chondroma of the sacrumCan J Surg 2008 51(5):E105-06. [Google Scholar]
[17]. Kenan S, Abdelwahab IF, Klein MJ, Lewis MM, Case report 837: Juxtacortical (periosteal) chondromyxoid fibroma of the proximal tibiaSkeletal Radiol 1994 23(3):237-39.10.1007/BF001974718016680 [Google Scholar] [CrossRef] [PubMed]
[18]. Durr HR, Lienemann A, Nerlich A, Stumpenhausen B, Refior HJ, Chondromyxoid fibroma of boneArch Orthop Trauma Surg 2000 120(1-2):42-47.10.1007/PL0002121410653103 [Google Scholar] [CrossRef] [PubMed]
[19]. Zheng K, Yu X, Xu S, Xu M, Periosteal chondroma of the femur: A case report and review of the literatureOncology Letters 2015 9(4):1637-40.10.3892/ol.2015.288925789014 [Google Scholar] [CrossRef] [PubMed]
[20]. Agrawal A, Dwivedi SP, Joshi R, Gangane N, Osteochondroma of the sacrum with a correlative radiographic and histological evaluationPediatr Neurosurg 2005 41:46-48.10.1159/00008486515886513 [Google Scholar] [CrossRef] [PubMed]
[21]. Sam HS, Shooshtarizadeh T, Zekavat H, Bahrabadi M, Juxtacortical chondromyxoid fibroma of tibiaBiomed J Sci & Tech Res 2017 1(5):1394-96.10.26717/BJSTR.2017.01.000445 [Google Scholar] [CrossRef]
[22]. Mora R, Guerreschi F, Fedeli A, Alfarano M, Angi V, Two cases of periosteal chondromaActa Orthop Scand 1988 59(6):723-27.10.3109/174536788091494353213465 [Google Scholar] [CrossRef] [PubMed]