Plaster Ingestion and Concurrent Fuel Oil Poisoning: An Unusual Method of Suicide
Asad Imani1, Hamid Heidarzadeh2, Hadis Nazari3, Sara Mohammadnejad4, Saleheh Tajalli5
1 Department of Nursing, Faculty of Nursing and Midwifery, Ilam University of Medical Sciences, Ilam, Iran.
2 Department of Nursing, Faculty of Nursing and Midwifery, Ilam University of Medical Sciences, Ilam, Iran.
3 Department of Nursing, Faculty of Nursing and Midwifery, Ilam University of Medical Sciences, Ilam, Iran.
4 Department of Nursing, Faculty of Nursing and Midwifery, Ilam University of Medical Sciences, Ilam, Iran.
5 Student Research Committee, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Hamid Heidarzadeh, Faculty of Nursing and Midwifery, Ilam University of Medical Sciences, PO Box: 69391-77143, Ilam, Iran.
E-mail: heidarzadehh@medilam.ac.ir
Suicide is one of the leading causes of death in the world and all type of suicides are remarkable for health workers. However, concurrent use of plaster diluted in water and fuel oil (gasoline) is unreported. A 68-year-old man with history of suicide attempts was brought to the emergency department. He attempted suicide by consuming 50 gm of plaster powder diluted in water and gasoline (30 gm) concurrently. In the present case, surgical intervention was not done and the treatment approach was mainly conservative in nature.
Attempted suicide, Diluted plaster, Gasolines
Case Report
A 68-year-old male with history of suicide attempts was brought to the emergency department. He neither smoked nor was an alcoholic or drug addict. One of the relatives told that the patient had intentionally ingested approximately 50 gm of plaster 30 minutes ago, because of recent family conflict and financial problems. He diluted plaster in water and drank it. Also, after 2 minutes, he drank approximately 30 gm of gasoline.
The patient was admitted with vague pain in epigastrium, coughing, frequent nausea with once vomiting, agitation and without chest pain. At the time of admission, cardiac monitoring and Electrocardiogram (ECG) showed normal sinusal rhythm. He was oriented to time, place, and person.
On physical examination, the abdomen was soft without any palpable mass and the whitish spots were seen around the mouth. Vital signs of patient were recorded as follows: Blood Pressure=110/70 mm/Hg, Pulse=76 pulse/minute, Temperature=36.8°C and RR=17 bpm. Arterial blood gases indicated normal respiratory conditions {arterial oxygen tension (paO2): 85 mmHg; arterial carbon dioxide tension (paCO2): 37 mmHg; arterial oxygen saturation (SaO2): 94% and arterial pH: 7.4}.
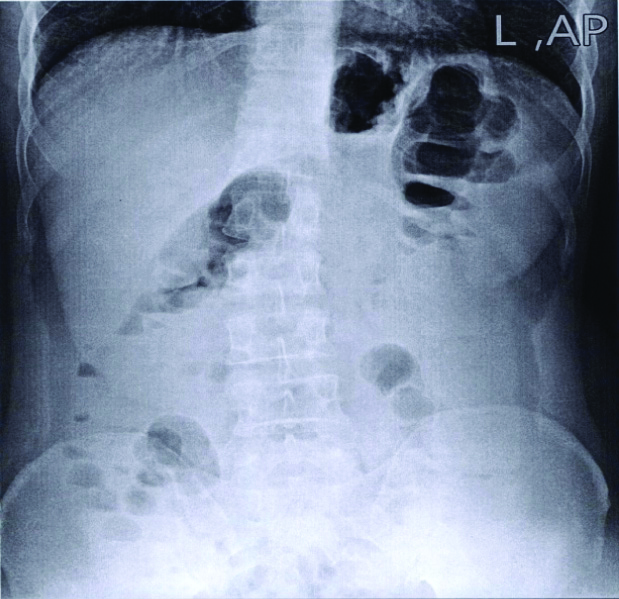
Upon admission, all of the patient’s clothes were removed, and the area around the mouth was thoroughly washed with water and soap, and oxygen was immediately given through nasal cannula. In the present case, due to less plaster ingestion (50 gm), the subsequent radiographs showed that there was no white opaque sign in abdominal X-ray, bezoar formation or pathologic findings [Table/Fig-1]. A consultation with general surgery specialist and medical toxicologist was made and the patient was transferred to the general ward. Some of the supportive treatments were done in ward, such as oxygen therapy with nasal cannula with 4-5 lit/minute, controlling nausea and vomiting with 4 mg IV/bolus of Amp ondansetron, and then controlled with 0.15 mg/kg/q 12 hourly. Treatment was done based on conservative and antibiotic approach to prevent the side effects of probable aspiration, due to vomiting. After 24 hours of conservative treatment, gastric lavage showed that there were no remnants of white plaster. After 48 hours of treatment there were no whitish spots seen and defecation was also normalised.
After the third day, the patient was discharged with a good general status, no cough or respiratory distress and without any gastroenteritis symptoms or haemodynamic problems. At the time of discharge, the patient was councelled, to prevent the recurrent suicide attempts. After two weeks, patient was in good general condition and had no physiological problems. He also had two consultations with a psychologist during this time.
Discussion
Suicide is one of the leading causes of death in the world and is considered to be a major health problem for most countries. Individuals commit suicide for multiple complex and intangible reasons, but society is often not willing to talk openly about this issue [1]. Suicidal behaviour is often the result of a complex matrix of clinical, familial, economic, political and even geographical variables [2].
In the past two decades in Iran, family conflicts was the most prevalent cause of suicide attempts [3]. In the present case also, family conflict and financial problems were mentioned as causes of suicide attempts. It has been estimated that by 2020, about 1530000 people will attempt suicide [4]. According to Iran’s Forensic Medicine organisation reports, nationwide rates of suicide in Iran were 5.7 per 100000 for males and 3.1 for females [5]. Suicide methods vary across different countries, perhaps reflecting different lifestyles, culture and religious beliefs [6].
Literatures indicates, that the dominant methods used for suicide in Asia are hanging and solid or liquid poisoning [7]. Different studies show that the most common methods for suicide in Iran are hanging, self-immolation, drug poisoning, and suicide with a firearm, respectively [8]. Some of these methods, such as hanging or shooting have a high fatality rate. Other methods such as drugs, on the contrary, have a low fatality rate [9]. Plaster ingestion has been reported as a suicide method only in Iran [10], and Germany [11]. However, in this case report, the authors described a suicide attempt with plaster ingestion concurrent with drinking gasoline, as an unusual method. In plaster ingestion, treatment depends on the time interval between ingestion and arrival to the emergency department. If this period is short, the patient can be treated by gastric irrigation [12]. In cases with bezoar formation in gastric or accompanying problems such as perforation or obstruction, surgery is recommended. A study done in Iran showed that gastric irrigation in all of the patients leads to prevention of surgical intervention. Only in one case, surgical intervention was done [13]. This patient was lavaged with less than normal 2-litre saline. In another study, surgical intervention was done following consuming 450 gm plaster [10]. However, in the present case, due to the low plaster ingestion (50 gm), and the lack of pathologic evidence in patient’s abdominal X-ray, surgical intervention was not done. Also, due to the concurrent use of gasoline, the insertion of nasogastric tube was not done and then conservative management was applied; followed-up by frequently abdominal examinations over 24 hour. In these examinations, no evidence was found in favour of palpable mass in the abdomen or epigastrium.
Gasoline, a substance with low viscosity and high volatility, is associated with high aspiration risk. Also, it can lead to cardiac arrhythmias, by sensitising the myocardium to catecholamines or act as a simple asphyxiant, if its vapours displace sufficient oxygen from the breathing atmosphere [14]. Managing the airway is always the first approach in treating patients with gasoline poisoning. In present case, patient did not have any breathing complication, except coughing.
Conclusion
In concurrent poisoning with plaster and gasoline, the conservative treatment should be the first line of treatment. Invasive procedure should be used if there are life threatening factors and serious complications.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
PLAGIARISM CHECKING METHODS: [Jain H et al.]
Plagiarism X-checker: Jul 08, 2019
Manual Googling: Sep 09, 2019
iThenticate Software: Sep 26, 2019 (16%)
[1]. McConnell D, Hahn L, Savage A, Dubé C, Park E, Suicidal ideation among adults with disability in Western Canada: a brief reportCommunity Ment Health J 2016 52(5):519-26.10.1007/s10597-015-9911-326202547 [Google Scholar] [CrossRef] [PubMed]
[2]. May AM, Klonsky ED, What Distinguishes suicide attempters from suicide ideators? a meta-analysis of potential factorsClinical Psychology: Science and Practice 2016 23(1):05-20.10.1111/cpsp.12136 [Google Scholar] [CrossRef]
[3]. Nazarzadeh M, Bidel Z, Ayubi E, Soori H, Sayehmiri K, Factors related to suicide attempt in Iran: A systematic review and meta-analysisHakim Research Journal 2013 15(4):352-63. [Google Scholar]
[4]. Wang YC, Hsieh LY, Wang MY, Chou CH, Huang MW, Ko HC, Coping card usage can further reduce suicide reattempt in suicide attempter case management within 3-month interventionSuicide Life Threat Behav 2016 46(1):106-20.10.1111/sltb.1217726201436 [Google Scholar] [CrossRef] [PubMed]
[5]. Malakouti SK, Nojomi M, Bolhari J, Hakimshooshtari M, Poshtmashhadi M, De Leo D, Prevalence of suicide thoughts, plans and attempts in a community sample from Karaj, IranCommunity Ment Health J 2009 45(1):37-41.10.1007/s10597-008-9173-419051014 [Google Scholar] [CrossRef] [PubMed]
[6]. Ajdacic-Gross V, Weiss MG, Ring M, Hepp U, Bopp M, Gutzwiller F, Methods of suicide: international suicide patterns derived from the WHO mortality databaseBull World Health Organ 2008 86:726-32.10.2471/BLT.07.04348918797649 [Google Scholar] [CrossRef] [PubMed]
[7]. Wu KC, Chen YY, Yip PS, Suicide methods in Asia: implications in suicide preventionInternational Journal of Environmental Research and Public Health 2012 9(4):1135-58.10.3390/ijerph904113522690187 [Google Scholar] [CrossRef] [PubMed]
[8]. Shojaei A, Moradi S, Alaeddini F, Khodadoost M, Ghadirzadeh MR, Khademi A, The Association between Completed Suicides and Season of the Year in an Iranian PopulationIran J Public Health 2013 42(3):293-97. [Google Scholar]
[9]. Santander J, Brokering W, Ramos P, Arenas A, Suicide in hospitalized patients and medical liabilityRev Med Chil 2015 143(4):506-11.10.4067/S0034-9887201500040001326204543 [Google Scholar] [CrossRef] [PubMed]
[10]. Yegane R-A, Bashashati M, Bashtar R, Ahmadi M, Gastrointestinal obstruction due to plaster ingestion: a case-reportBMC Surg 2006 6:410.1186/1471-2482-6-416483375 [Google Scholar] [CrossRef] [PubMed]
[11]. Germerott T, Jaenisch S, Hatch G, Albrecht U-V, Guenther D, Planned complex suicide: Self-strangulation and plaster ingestionForensic Sci Int 2010 202(1-3):e35-37.10.1016/j.forsciint.2010.04.05320554136 [Google Scholar] [CrossRef] [PubMed]
[12]. Taheri MS, Kharrazi SM, Haghighatkhah HR, Moharamzad Y, Unusual acute formed gastric bezoars due to plaster ingestion successfully treated by gastric irrigation: report of two casesEmergency Radiology 2008 15(5):357-59.10.1007/s10140-007-0684-z18046589 [Google Scholar] [CrossRef] [PubMed]
[13]. Yeganeh R, Rafiei N, Kazemi AH, Ahmadi M, Dortag F, Study of cases of suicide with plaster as a new and strange way of suicide in Lorestan ProvinceYafteh 2004 5(4):23-28. [Google Scholar]
[14]. Srinivasa Murthy A, Das S, Bheemanathi Hanuman S, Fatal diesel poisoning: a case report and brief review of literatureAm J Forensic Med Pathol 2018 39(2):169-72.10.1097/PAF.000000000000038529465462 [Google Scholar] [CrossRef] [PubMed]