RA is a chronic multisystem autoimmune disease predominantly involving synovial joints, affecting 1-2% of general population [1]. Disease activity is measured by DAS 28 score in RA patients. DAS 28 is a composite disease score for defining severity of RA based upon total number of swollen and tender joint counts and patient’s perception of pain based upon Visual Analog Scale (VAS) (0-100 mm), calculated by using the formula: DAS28 = 0.56 × √(tender 28) + 0.28 × √(swollen 28) + 0.70 × ln(ESR) + 0.014 × VAS [2]. Extra articular disease, seen in about 40% RA patients, is the single most important cause of morbidity and mortality in RA [3]. Extra articular involvement is common in various stages of the disease [4]. However till date, there is no tool to access the severity of extra articular manifestations in RA. DAS, also known as Disease Activity Score, in RA combines the information from Swollen joints, Tender joints, acute phase response and patients’ global assessment as a single continuous measure for the disease activity in RA [5].
Physician’s Global Assessment, also called as Physician’s Global is a standardised data set which includes a 0-10 continuous VAS for recording. The values in 0-1 range indicates controlled or equivocal RA disease activity, and values in the 1.1-4, 4.1-8, and 8.1-10 ranges for mild, moderate, and high activity respectively [6].
Extra-Articular Manifestations (EAMs) are difficult to diagnose and treat since no clear consensus exists among the rheumatologists for their correct classification and also due to the fact that there are no guidelines available for their treatment. Therefore the aim of the current study was to make a composite score for EAM in RA.
Materials and Methods
This was a tertiary care teaching hospital based cross-sectional study conducted in Bhubaneswar, Odisha, India. After obtaining informed consent from all the patients who fulfilled 2010 ACR/EULAR classification criteria for RA [7] between the age group 18 to 60 years were included in the study. The patients with co-morbidities such as chronic airway diseases, liver diseases, renal diseases, diabetes mellitus, hypertension, hypothyroidism, current or past pulmonary tuberculosis, and connective tissue diseases other than RA, pregnant women were excluded from the study.
A total of 226 consecutive eligible patients with RA who attended the Outpatient Department (OPD) of rheumatology from 1st June 2018 to 30th December 2018 were included in this study. The study was approved by the Institutional Ethics Committee of the medical college (Kalinga Institute of Medical Sciences) (approval number KIMS/KIIT/69/2016 dated 22-09-2016).
Information on demographic and clinical characteristics such as sex, age, duration of disease, diagnosis, co-morbidities were collected. A complete physical, clinical examination and biochemical investigation (ESR, CRP, RF and Anti CCP) were done in each patient. Extra-articular disease parameters namely Skin Ulcer/Gangrene, Interstitial Lung Disease (ILD), Retinal Vasculitis, Scleromalacia, Coronary Artery Disease (CAD), Mononeuritis Multiplex, CNS Vasculitis, Nephritis, Amyloidosis, Felty/LGL Syndrome, Cord Compression, Lymphoma, Petechiae/Purpura, Pleurisy/Pleural Effusion, RA Lung Nodules, Scleritis/Episceritis, Valvular Heart disease, Myositis, Raynaud’s Phenomenon, RA Skin Nodules, Kerato Conjunctivitis Sicca (KCS), Pericarditis/Pericardial Effusion, Carpal Tunnel Syndrome, Anaemia, Thrombocytosis, Lymphadenopathy, Splenomegaly and Fever were assessed. Additionally, Physician’s Global Assessment Score and DAS 28 Score were also assessed and obtained for every patient; which are freely available for routine clinical use [6,8].
Weighting and Scoring
Based on the consensus of three well experienced rheumatologists, parameters for extra-articular disease, their weight and score were decided. A total of 28 extra-articular disease parameters were selected based on various common extra articular disease in RA, which were further grouped into 4 broader categories reflecting the importance of each parameter in the physicians’ ratings of disease activity and a weighting of 1, 2, 4 and 8 was assigned to each of the abnormal parameter which reflected their clinical importance [Table/Fig-1]. These weights were thought to be easier to remember for clinical use and a composite score based on these weights were compared with Physician’s Global Assessment score where the patients were reclassified into 3 groups; mild (VAS 1.1-4) with a score of 1, moderate (VAS 4.1-8) with a score of 2, and high disease activity (VAS 8.1-10) with a score of 3. This was considered as gold standard, as there is no such previous published literature on extra-articular RA assessment.
Disease activity index extra-articular manifestations in rheumatoid arthritis.
| Descriptor | Weight | Scores |
|---|
| Skin ulcer/Gangrene | 8 | 8 if present otherwise 0 |
| ILD | 8 | 8 if present otherwise 0 |
| Retinal vasculitis | 8 | 8 if present otherwise 0 |
| Scleromalacia | 8 | 8 if present otherwise 0 |
| CAD | 8 | 8 if present otherwise 0 |
| Mononeuritis multiplex | 8 | 8 if present otherwise 0 |
| CNS vasculitis | 8 | 8 if present otherwise 0 |
| Nephritis | 8 | 8 if present otherwise 0 |
| Amyloidosis | 8 | 8 if present otherwise 0 |
| Felty/LGL syndrome | 8 | 8 if present otherwise 0 |
| Cord compression | 8 | 8 if present otherwise 0 |
| Lymphoma | 8 | 8 if present otherwise 0 |
| Petechiae/Purpura | 4 | 4 if present otherwise 0 |
| Pleurisy/Pleural effusion | 4 | 4 if present otherwise 0 |
| RA lung nodules | 4 | 4 if present otherwise 0 |
| Sceleritis/Episceritis | 4 | 4 if present otherwise 0 |
| Valvular heart disease | 4 | 4 if present otherwise 0 |
| Myositis | 4 | 4 if present otherwise 0 |
| Raynaud’s phenomenon | 2 | 2 if present otherwise 0 |
| RA skin nodules | 2 | 2 if present otherwise 0 |
| KCS | 2 | 2 if present otherwise 0 |
| Pericarditis/Pericardial effusion | 2 | 2 if present otherwise 0 |
| Carpal tunnel syndrome | 2 | 2 if present otherwise 0 |
| Anaemia | 1 | 1 if present otherwise 0 |
| Thrombocytosis | 1 | 1 if present otherwise 0 |
| Lymphadenopathy | 1 | 1 if present otherwise 0 |
| Splenomegaly | 1 | 1 if present otherwise 0 |
| Fever | 1 | 1 if present otherwise 0 |
| Total maximum possible scores | 135 |
Hence, each individual was allocated a risk score. Patients were classified as no risk associated with score 0, low risk with a score range from 1 to 3, medium risk with a score range 4 to 8 and high risks associated with a score of more than 8 based on the consensus of rheumatologists (at least 10 years of expertise in the field).
Statistical Analysis
All the categorical parameters were reported as frequency and percentage whereas continuous parameters were presented in Mean±SD (Standard Deviation). Categorical parameters were compared among the various risk group using either Chi-square test or Fisher’s-exact test and continuous parameters were compared by One-Way Analysis of Variance (ANOVA) and Kruskal Wallis ANOVA followed by a multiple comparison test using Bonferroni adjustment. The Spearman’s Rank correlation Coefficient test was applied to find out the relationship between Physician’s Global Assessment score and DAS-EAM score. A quantification of Pearson’s correlation coefficient and scatter plot were shown between original DAS-28 and calculated composite scores. A Kappa statistics was performed to quantify the agreement between classified DAS-28 and classified composite score.
Data were analysed using standard statistical software Stata 15.1. A p-value of <0.05 was considered as statistical significant.
Results
Different socio-demographic and biochemical parameters for a total of 226 RA patients have been summarised in [Table/Fig-2].
Summary of socio-demographic and biochemical parameters for 226 Rheumatoid Arthritis patients.
| Parameters | Summary |
|---|
| Age (in years); Mean±SD | 49.4±11.8 |
| Disease duration (in months); |
| Mean±SD | 89.7±77.6 |
| RF; n (%) |
| Negative | 11 (10.6) |
| Positive | 92 (89.3) |
| Anti CCP; n (%) |
| Negative | 5 (6.7) |
| Positive | 70 (93.3) |
| Presence of either of RF or Anti-CCP; n (%) |
| Negative | 4 (3.4) |
| Positive | 114 (96.6) |
| Sex; n (%) |
| Male | 21 (9.3) |
| Female | 205 (90.7) |
[Table/Fig-3] shown that 50% of the patients were Anaemic followed by Kerato Conjunctivitis Sicca (12.8%), Lymphadenopathy (8.85%), Interstitial Lung Disease (8.41%), RA Skin Nodules (6.64%), Carpal Tunnel Syndrome (6.19%), fever (3.1%) and Thrombocytosis (1.78%). CAD, Mononeuritis Multiplex, Scleromalacia and Pleurisy/Pleural Effusion were found in less than 1% of patients. Other EAM parameters namely Skin Ulcer/Gangrene, Retinal Vasculitis, CNS Vasculitis, Nephritis, Amyloidosis, Felty/LGL Syndrome, Cord Compression, Lymphoma, Myositis Petechiae/Purpura, RA Lung Nodules, Sceleritis/Episceritis, Valvular Heart Disease, Raynaud’s Phenomenon, Pericarditis/Pericardial Effusion, and Splenomegaly were not present.
Presentation of various extra-articular manifestations in rheumatoid arthritis patients.
| EAM parameters | N (227) | % |
|---|
| Anaemia | 113 | 50 |
| KCS | 29 | 12.8 |
| Lymphadenopathy | 20 | 8.85 |
| ILD | 19 | 8.41 |
| RA skin nodules | 15 | 6.64 |
| Carpal tunnel syndrome | 14 | 6.19 |
| Fever | 7 | 3.1 |
| Thrombocytosis | 4 | 1.78 |
| CAD | 2 | 0.9 |
| Mononeuritis multiplex | 2 | 0.88 |
| Scleromalacia | 1 | 0.44 |
| Pleurisy/Pleural effusion | 1 | 0.44 |
[Table/Fig-4] shows the mean and standard deviation of DAS-28 (3.58±1.27) and DAS-EAM score (2.03±2.90) among rheumatoid arthritis patients. Additionally frequency distribution is reported with different cut-offs of DAS-28 and DAS-EAM score. According to physician global assessment scale, extra-articular manifestations among RA patients is also described in [Table/Fig-4].
Level of different Clinical Scores to predict extra-articular manifestations in rheumatoid arthritis patients.
| Scores to predict EAM | Mean±SD; n(%) |
|---|
| DAS-28 score; | 3.58±1.27 |
| ≤3.2 (Mild) | 99 (45.0) |
| 3.2-5.1 (Moderate) | 96 (43.6) |
| >5.1 (Severe) | 25 (11.4) |
| Physical global assessment score | n (%) |
| 0-Controlled RA | 50 (22.4) |
| 1-Mild | 95 (42.6) |
| 2-Moderate | 74 (33.2) |
| 3-Severe | 04 (1.79) |
| DAS-EAM score; Mean±SD | 2.03±2.90 |
| 0 | 82 (36.4) |
| 1-3 | 109 (48.5) |
| 4-8 | 20 (8.9) |
| >8 | 14 (6.2) |
[Table/Fig-5] shows that among RA patients, increasing age had significantly higher DAS-EAM score. The duration of disease was not statistically significant. Presence of RF and/or Anti-CCP did not influence DAS EAM score. There was no influence of gender on DAS-EAM score.
Association of different socio-demographic and biochemical parameters with DAS-EAM score.
| Parameters | DAS-EAM score classification | p-value |
|---|
| 0 | 1- 3 | 4-8 | >8 |
|---|
| Age (in years); Mean±SD | 49.4±12.3 | 47.1±10.9 | 55.5±12.2 | 57.2±9.0 | 0.001 |
| Disease duration (in months); |
| Mean±SD | 82.7±74.5 | 84.5±74.1 | 101.5±64.2 | 135.4±97.2 | 0.079 |
| RF; n (%) |
| Negative (11) | 3 (27.3) | 8 (72.7) | 0 (0.0) | 0 (0.0) | 0.526 |
| Positive (91) | 23 (25.0) | 48 (52.2) | 11 (12.0) | 10 (10.9) |
| Anti CPP; n (%) |
| Negative (5) | 3 (60.0) | 2 (40.0) | 0 (0.0) | 0 (0.0) | 0.551 |
| Positive (68) | 22 (31.4) | 36 (51.4) | 4 (5.7) | 8 (11.8) |
| Any positive of RF or Anti-CCP |
| Negative (4) | 2 (50.0) | 2 (50.0) | 0 (0.0) | 0 (0.0) | 0.841 |
| Positive (112) | 32 (28.1) | 59 (51.7) | 11 (9.7) | 12 (10.5) |
| Sex |
| Male | 9 (42.9) | 9 (42.9) | 2 (9.5) | 1 (4.8) | 0.900 |
| Female | 73 (35.8) | 100 (49.0) | 18 (8.8) | 13 (6.4) |
Tests applied-One-way ANOVA, Kruskal-Wallis ANOVA and Fisher’s-exact test
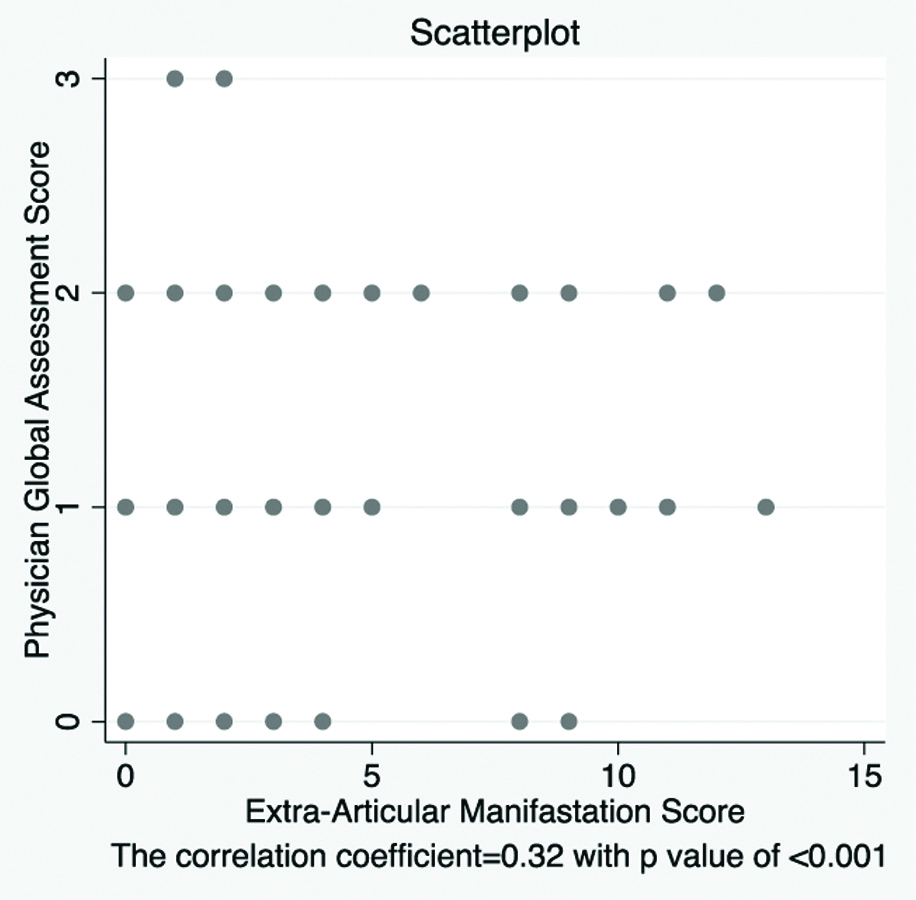
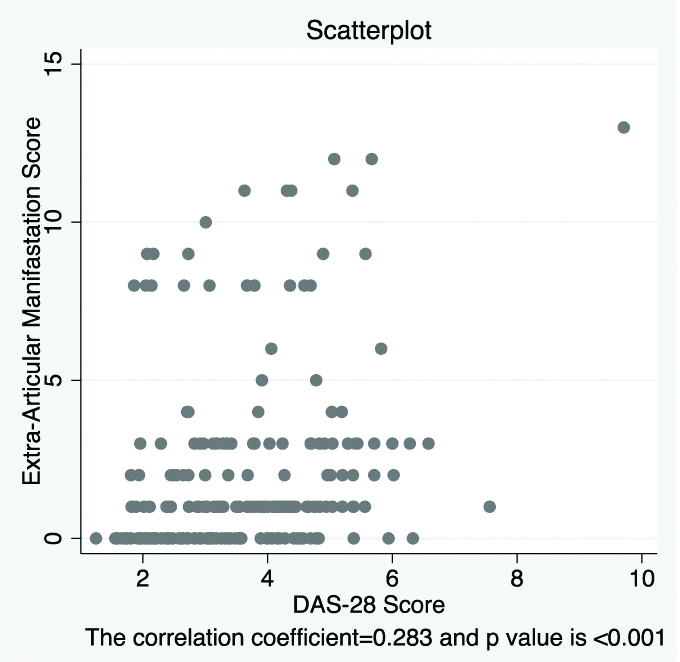
A correlation coefficient between Physician’s global assessment score and DAS-EAM score was observed as 0.32 with p-value of <0.001, as depicted in [Table/Fig-6] as scatter plot diagram. Additionally an agreement between Physician global assessment score and DAS-EAM score was observed as 41% (Kappa value =0.12) with p-value of 0.002 which was a significant moderate agreement. The agreement between DAS-28 and DAS-EAM score was observed as 21.5% (Kappa= -0.06) with p-value 0.983 which indicated no agreement between these two scores. The correlation coefficient between DAS 28 and DAS-EAM score was observed as 0.283 with p-value of <0.001. Also, scatter plot in [Table/Fig-7] clearly demonstrated that DAS-28 and DAS-EAM score were not linearly related.
Scatter plot between Physician’s Global Assessment score and DAS EAM Scores.
*Spearman’s Rank correlation
(The correlation coefficient r=0.32 with p-value of <0.001)
Scatter plot between DAS-EAM score and DAS 28 Scores.
*Pearson’s correlation coefficient
(The correlation coefficient r=0.283 and p-value is <0.001)
Discussion
In the study, though the correlation coefficient was found to be significant, there was no clinically meaningful correlation pattern between DAS-28 and DAS-EAM score depicted in the scatterplot. Also, the observed non-significant agreement between these two entities clearly indicates the present scoring system for disease activity in RA based on solely joints counts is not enough to predict the presence and severity of extra-articular disease. A DAS-EAM score in each RA patient should be a mandatory tool for composite disease assessment in addition to DAS-28.
It was found that the increasing age of the patients had a significant correlation with the DAS-EAM score. This is again related to the fact that in rheumatoid arthritis, the presence of extra-articular disease and co-morbidities in elderly could influence adverse outcome in these population. This finding is similar to study by Inbanathan J et al., where older age group patients had more extra-articular manifestations [9].
Serology, RF, and Anti-CCP antibodies did not influence the DAS-EAM score. This is contrary to previous literature which indicates DAS-EAM scoring is mandatory tool for assessment of extra-articular disease and its outcome and not the mere presence or absence of either RF or Anti-CCP [10]. Similarly gender did not influence our DAS-EAM score, though RA is more common in females.
Longer duration of disease is often associated with more extra-articular manifestations in RA and more cardiovascular events [11,12]. However in current study, this was again not found to be significant in comparison to DAS-EAM score which could be due to smaller sample size.
Physician’s Global Assessment score and DAS-EAM score had a significant positive correlation in this study. Hence the importance of inclusion of Physician’s Global Assessment score in DAS-EAM score could be a better tool for assessment of extra-articular disease in RA.
Limitation
The study has following limitations such as small sample size, single centre and cross-sectional study. In general, for assessment of disease activity in RA, a longitudinal study is warranted. However, this is the only and earliest attempt for extra-articular disease activity in RA. Hence, a multi-centric prospective study with validation model for the same is suggested.
Conclusion
DAS-EAM score can be a useful tool to monitor extra-articular disease severity in RA. Prospective validation for the same is warranted for future clinical use.
Tests applied-One-way ANOVA, Kruskal-Wallis ANOVA and Fisher’s-exact test