LipStaT- Know Where, When and How?
Priyanka Chopra1, Shalini Kapoor2, Preeti Karhana3
1 Head of the Department, Department of Periodontology, SGT Dental College, Gurugram, Haryana, India.
2 Associate Professor, Department of Periodontology, SGT Dental College, Gurugram, Haryana, India.
3 Postgraduate Student, Department of Periodontology, SGT Dental College, Gurugram, Haryana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Priyanka Chopra, SGT University, Gurugram, Haryana, India.
E-mail: drpriyankachopra79@gmail.com
Excessive Gingival Display (EGD) is an aesthetic concern affecting a considerable section of the population. Labial hyperactivity, gingival overgrowth, delayed passive eruption, vertical maxillary excess or a combination of them may result in excessive gingival appearance. LipStaT was similar technique to first introduced by Rubinstein and Kostianovsky’s in 1973 for treatment of high smile lines. Here, a case of 22-year-old female patient who reported with the chief complaint of gummy smile has been discussed. On extra-oral examination, the face was found to be bilaterally symmetrical with competent lips. Intraorally, gingival display was 6 mm during dynamic smile which extended from premolar to premolar. The treatment planned was to surgically minimise the gingival display in her smile using LipStaT Technique. The present paper also discuss in detail about the indications of LipStaT, clinical case selection, treatment and possible complications.
Excessive gingival display, Hyperactivity of lip, Vertical maxillary excess
Case Report
A 22-year-old female patient reported to the OPD of the Department of Periodontology and Oral Implantology with the chief complaint of excessive display of gums during talking and smiling. Medical, dental and drug history was negative. On extraoral examination, the face was found to be bilaterally symmetrical with competent lips. Intraoral examination revealed Gingival display of 4-6 mm while talking. The gingival display increased upto 6 mm on dynamic smile. The colour, contour, consistency and texture of gingiva was found to be normal. Complete clinical evaluation based on the classification of Excessive gingival display was done [1]. Detailed intraoral examination of the patient revealed that there was no discrepancy in crown measurements [Table/Fig-1]. So, EGD (A) was ruled out. EGD (C) was also ruled out as no gingival enlargement was present in the case. There was no hypermobility of maxillary lip and the maxillary lip length was found to be adequate, thus ruling out EGD (D) and EGD (E) [Table/Fig-2]. On dividing the face into three equal halves i.e., from trichion to glabella (upper 1/3rd), from glabella to subnasale (middle 1/3rd) and subnasale to menton (lower 1/3rd), it was found to be a case of vertical maxillary excess by 6 mm. Bony maxillary excess was present with the discrepancy of 0.5-0.7 mm which comes under degree 2 an indication towards lipStaT. Hence, the final diagnosis was EGD (B) Degree 2 [Table/Fig-3]. Considering all the above points; LipStaT procedure was treatment of choice in the present case. The patient was referred for blood investigations prior to surgery. The counts were found to be within normal limits.
Normal crown measurements.

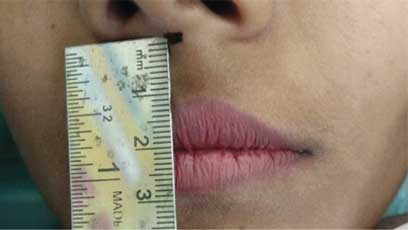
Excessive gingiva on dynamic smile.

Surgical Procedure
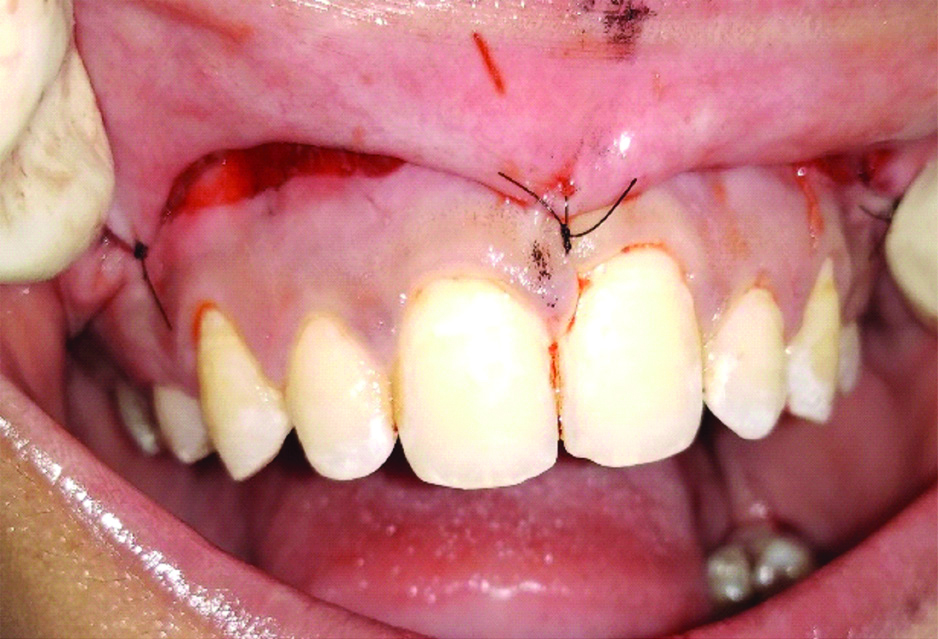
Complete treatment plan was explained to the patient. After getting the informed consent, standard skin preparation was carried out by 10% povidone-iodine solution and temporary draping was done. Adequate local anaesthesia was administered. It was decided to excise 8-10 mm of tissue as the rule follows to remove the double of the gingival display. The Borders of surgical incision area were marked using a surgical marker [Table/Fig-4]. Midline was also marked. The inferior border was located at the mucogingival junction and extended laterally based on the horizontal extent of the dynamic smile. The superior border was extended into the vestibule depending on the subclass of Excessive Gingival Display (B). Partial thickness incisions were made along superior and inferior borders and joined with vertical incisions at posterior aspect using 15 no. BP blade, junction extending from right first premolar to left first premolar [Table/Fig-5]. By partial thickness dissection, outlined mucosa was removed which exposed the underlying connective tissue [Table/Fig-6]. Suturing was first initiated at midline by placing interrupted sutures using 5-0 non-resorbable material (Trulon®). The first suture was placed midway between midline and most distal aspect of dissection [Table/Fig-7]. Additional sutures were then placed approximately 3 mm apart to approximate wound edges [Table/Fig-8].
Superior & inferior borders marked.

Raising partial thickness flap.

Removal of excess mucosa.

First suture placed at midline.

Post-operative Instructions
Prescription for analgesics (ibuprofen, 600-800 mg every 6-8 hours for pain) and chlorhexidine gluconate 0.12% (twice daily for 2 weeks) were given. Instructions were given to apply cold compression in form of an ice pack at 20-minute intervals after 24 hours. Patient was advised to avoid any manipulation or mechanical trauma to surgical area, by reducing lip movements while talking or smiling during first 10 to 14 days. Follow-up done at fifth day [Table/Fig-9]. Suture removal was done at second week post-operatively [Table/Fig-10] and only 1-2 mm of gingival display was observed during dynamic smile [Table/Fig-11]. Well appreciated change in the smile and excessive gingival display pre-operative and post-operative is shown in [Table/Fig-12]. Gingival display at rest was 6 mm pre-operatively and 2 mm post-operatively.

Follow-up at second week to show satisfactory mucosal healing.

Post-opertaive display of gingiva.

Pre-operative and Post-operative photograph.

No complications were reported, except the patient felt some tension at the suture area during first week. The healing was found satisfactory at the follow-up visits at second and third week. Follow-up and observations was done by the operator at 5 months and no complication was reported.
Discussion
Smile is the important part of our personality. Any discrepancies in it make the patient conscious. EGD is the excessive gingival exposure during smile and is an aesthetic concern for most of the patient. An imbalance in the gingival-tooth ratio results in dominance of gingival appearance often referred to as “gummy smile. The harmony of smile is determined not only by the shape, position and colour of the teeth but also by the gingival tissues. The normal gingival display between the gingival margin of the central incisors and the inferior border of the upper lip during a normal smile is 1-2 mm. Whereas, an excessive gingiva-to-lip distance of 4 mm or more is classified as unattractive [1]. When Kokich VO Jr et al., studied the gingiva-to-lip distance, they reported it as noticeably unattractive at 4 mm by layperson and at 2 mm by orthodontists, whereas others placed the threshold at 1 mm [1]. It can affect a large percentage of the population, with prevalence ranging from 10.5% to 29% [2]. It is considered that women are more concerned about aesthetics as compared to men [3].
As aetiology is multifactorial, simply it is classified into-Excessive gingival display (A)-Altered Passive eruption; Excessive gingival display (B)-Bony Maxillary Excess; Excessive gingival display (C)-Conditions Causing gingival Enlargement; Excessive gingival display (D)-Deficient Maxillary Lip Length; Excessive gingival display (E)-Excessive Mobility of the maxillary lip; which further divided by subclasses. Excessive gingival display (B)- degree 1 and 2, Excessive gingival display (E)-subclass- 1,2 and 3 are indications for LipStaT [4]. A classification for altered passive eruption was suggested by Coslet JG et al., [Table/Fig-13]. Vertical maxillary excess is a condition that involves an overgrowth of the maxilla in the vertical dimension and many times it appears as a long face syndrome [Table/Fig-14] [5,6].
Classification of altered passive eruption of altered passive eruption Classification of altered passive eruption.
| Type | Description | Treatment |
|---|
| 1A | Osseous crest apical to cementoenamel junctionAdequate amount of attached gingivaGingival margin incisal to CEJ | Gingivectomy |
| 1B | Osseous crest at CEJAdequate amount of attached gingivaGingival margin incisal to CEJ | Gingivectomy and osseous surgery |
| 2A | Osseous crest at CEJInadequate amount of attached gingivaGingival margin incisal to CEJ | Apically positioned flap |
| 2B | Osseous crest at CEJInadequate amount of attached gingivaGingival margin incisal to CEJ | Apically positioned flap and osseous surgery |
Vertical maxillary excess classification classification.
| Type | Description | Treatment |
|---|
| I | 2 to 4 mm | Orthodontic intrusion only Orthodontics and periodontics Periodontics and restorative therapy |
| II | 4 to 8 mm | Periodontics and restorative therapy Orthognathic surgery |
| III | 8+ mm | Orthognathic surgery with or without adjunctive periodontal therapy and restorative therapy |
Rubinstein AM and Kostianovsky AS, (1973) described a procedure where an elliptical portion of gingiva and buccal mucosa was excised and borders were approximated and sutured together [7]. This described technique was similar to the LipStaT. Proper sequencing of treatment is needed to obtain the ideal outcome. All orthognathic, orthodontic, restorative, and initial periodontal therapy must be completed before beginning with LipStaT. Borders are marked using surgical marker Posterior extension is based on horizontal extent of dynamic smile Vertical extension is based on subclass of Excessive gingival display (E). Removal of the outlined mucosa by partial thickness dissection, exposes the underlying connective tissue.
LipStaT is a versatile technique to decrease the amount of Excessive gingival display. The LipStaT is a predictable technique for management of Excessive gingival display (B) degree 1 and 2 and Excessive gingival display (E) subclass 1, 2, and 3, along with combination cases of Excessive gingival display (A) to Excessive gingival display (E). There is minimal post-operative morbidity and low incidence of complications. Faster recovery is observed as compared to orthognathic surgery and myotomy [4].
In patients with inadequate attached gingiva and patients with severe skeletal deformities and severe vertical maxillary excess that has to be treated with orthognathic surgeries, this surgical technique cannot be used [8]. There are chances of recurrence also. The improvement in quality of life and confidence level as the procedure met the esthetic demands of the patient [9].
Conclusion
LipStaT is sensitive surgical procedure which requires skill and meticulous case selection for its long term success. This technique gives immediate results with the patient satisfaction and there is minimum postoperative swelling or pain.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
PLAGIARISM CHECKING METHODS: [Jain H et al.]
Plagiarism X-checker: Jun 10, 2019
Manual Googling: Sep 12, 2019
iThenticate Software: Sep 26, 2019 (18%)
[1]. Kokich VO Jr, Kiyak HA, Shapiro PA, Comparing the perception of dentists and lay people to altered dental estheticsJ Esthet Dent 1999 11(6):311-24.10.1111/j.1708-8240.1999.tb00414.x [Google Scholar] [CrossRef]
[2]. Dong JK, Jin TH, Cho HW, Oh SC, The esthetics of the smile: a review of some recent studiesInt J Prosthodont 1999 12:09-19. [Google Scholar]
[3]. Ackerman MB, Ackerman JL, Smile analysis and design in the digital eraJ Clin Orthod 2002 36:221-36. [Google Scholar]
[4]. Bhola M, Fairbairn JMP, LipStaT: The lip stabilization technique-indications and guidelines for case selection and classification of excessive gingival displayInt J Periodontics Restorative Dent 2015 35:549-59.10.11607/prd.205926133145 [Google Scholar] [CrossRef] [PubMed]
[5]. Coslet JG, Vanarsdall R, Weisgold A, Diagnosis and classification of delayed passive eruption of the dentogingival junction in the adultThe Alpha Omegan 1977 70(3):24-28. [Google Scholar]
[6]. Silberberg N, Goldstein M, Smidt A, Excessive gingival display in a smile- Etiology, diagnosis, treatment modalitiesQuintessence Int 2009 40:809-18. [Google Scholar]
[7]. Rubinstein AM, Kostianovsky AS, Surgery of the malformation of the smilePren Med Argent 1973 60:952[Translated from Spanish] [Google Scholar]
[8]. Ezquerra F, Berrazueta MJ, Ruiz-Capillas A, Arregui JS, New approach to the gummy smilePlast Reconstr Surg 1999 104:1143-50.10.1097/00006534-199909020-0004210654758 [Google Scholar] [CrossRef] [PubMed]
[9]. Rao AG, Koganti VP, Prabhakar AK, Soni S, Modified lip repositioning: A surgical approach to treat the gummy smileJ Indian Soc Periodontol 2015 19:356-59.10.4103/0972-124X.15240026229285 [Google Scholar] [CrossRef] [PubMed]