Ranula is an oral floor cyst, originating from the extravasation of salivary mucus from the sublingual gland due to obstruction of the gland ducts. This report presents the case of an extensive congenital plunging ranula in a 19-day-old male newborn. The infant presented easy fatigue, with delay in the time of the feedings during breastfeeding due to volumetric enlargement in mouth floor and ventral tongue regions since birth. The therapeutic proposal was marsupialization of the lesion. However, during surgery, due to the ranula’s location and the possibility of relapse, the enucleation of the lesion was performed. Infant was kept intubated in the neonatal ICU for three days and was under nasogastric fed for seven days. Excision of the ranula and maintenance of intubation was done until the reduction of post-operative oedema prevented intercurrences in the post-operative period and allowed a good clinical evolution of the child who recovered his respiratory and digestive function.
Case Report
A 19-day-old male newborn was attended at the craniofacial malformations outpatient clinic. His mother reported a normal delivery birth in a public hospital in the city of Cuiabá.
The mother stated that the child was born with a “tumour in the mouth” and that she had difficulty in breastfeeding and breathing, therefore she was referred to the neonatal intensive care unit of the hospital. CT scan was performed at the hospital and showed an extensive hypodense image, with a cystic appearance, on floor of mouth and ventral tongue [Table/Fig-1]. The child had a satisfactory clinical evolution without respiratory decompensation being discharged from the hospital and referred for outpatient evaluation in the service of craniofacial malformations.
Computed tomography (axial section) showing extensive hypodense image, with cystic aspect, on topography of floor of mouth and ventral surface of tongue.

The buccomaxillofacial surgery team found an extensive volume increase in the floor of the mouth of newborn, which caused posterior projection of the tongue. At rest, there was no change in the child’s respiratory pattern. During breastfeeding, the child presented easy fatigue, with delay in the time of the feedings. In addition, the newborn had detachable whitish plaques distributed throughout the oral mucosa, compatible with moniliasis [Table/Fig-2], for which oral nystatin was prescribed.
Infant’s oral cavity showing increased volume floor of mouth with posterior projection of the tongue and whitish plaques on the mucosal surface.

After one week, the moniliasis resolved and it was verified that the extensive volume increase in floor of mouth and ventral surface of tongue was a submucosal lesion without disruption of oral epithelial integrity. The clinical presentation added to the tomographic image led to the diagnostic hypothesis of salivary retention cyst (ranula) and the therapeutic proposal was the marsupialization of the lesion.
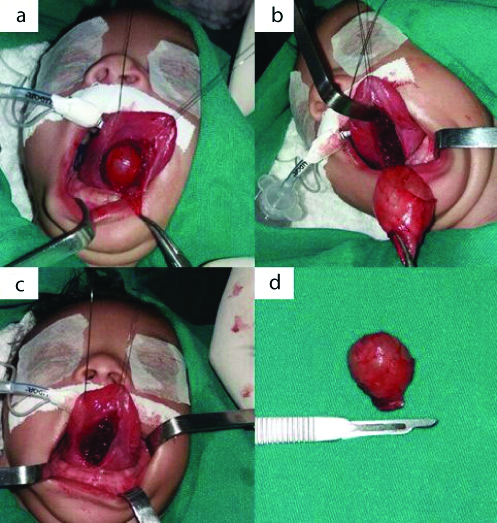
General anaesthesia was administrated to the child with orotracheal intubation. At that time, the inspection showed that the surface of the mucosa was not very close to the limit of the lesion. An incision was made in the floor of mouth and tissue dissection confirmed that the lesion was deeper than it appeared on physical examination. The progression of dissection demonstrated that the lesion was extensive, projected posteriorly towards the body of the tongue, and it was possible to remove it completely [Table/Fig-3]. After removal, suture was performed by planes with 4-0 monocryl wire in the deep plane and monocryl 5-0 in the surface plane. After excision, the lesion was sent for histopathological investigation.
a) Surgical access on floor of mouth and ventral surface of tongue, demonstrating extensive lesion, projecting posteriorly on the body of the tongue; b) Extensive lesion well delimited; c) Ventral surface of tongue after lesion enucleation; d) Cystic lesion.
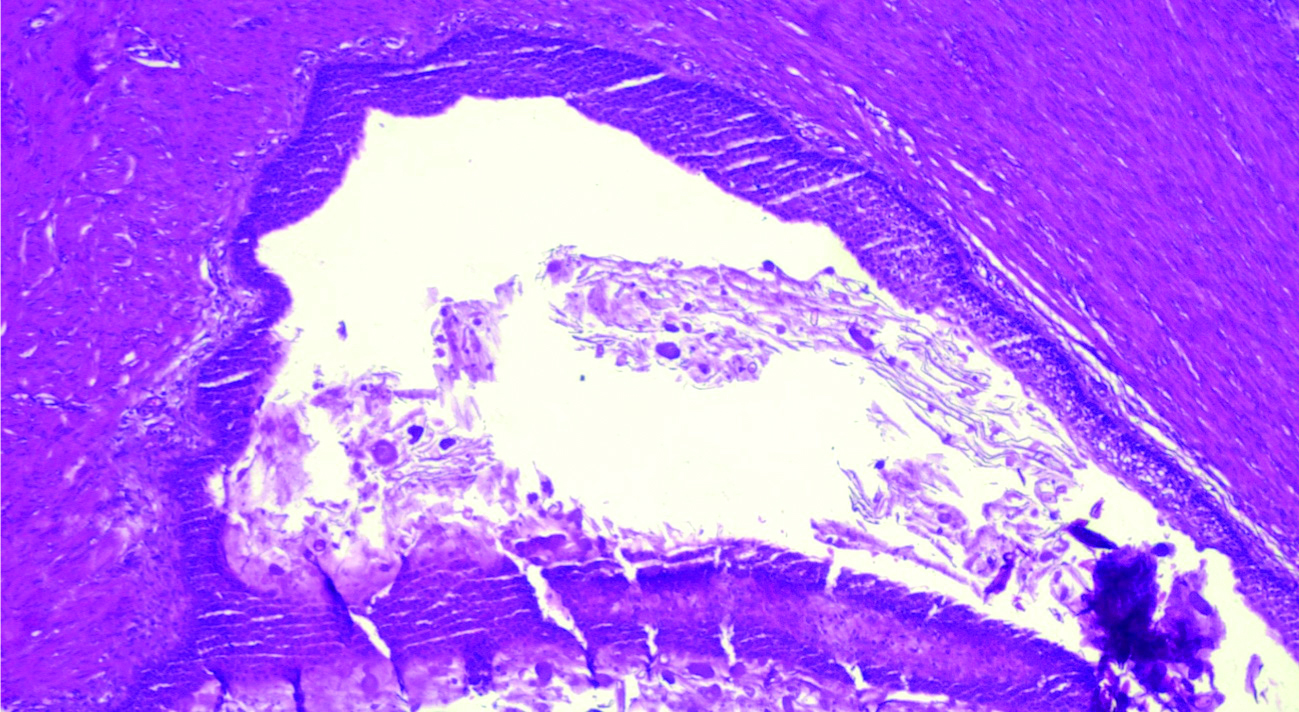
The histopathological analysis showed a fragment of muscular and fibroadipose connective tissue with a lesion of cystic lining at the center, internally coated by mucoproductive glandular epithelium and cylindrical, ciliated pseudostratified, without atypia, with areas of squamous metaplasia. The lumen was filled by mucus and a moderate amount of histiocytes were also seen. The histopathological picture confirmed the diagnostic of ranula [Table/Fig-4].
Fragment of muscular and fibroadipose connective tissue showing, at the center, lesion of cystic lining, internally coated by mucoproductive glandular epithelium and cylindrical, ciliated pseudostratified, without atypia, with areas of squamous metaplasia; the lumen is filled by mucus and a moderate amount of histiocytes were seen; a histopathological picture compatible with the clinical hypothesis of a ranula (H&E stain 100x).
As the dissection was ample, the possibility of important post-operative oedema and consequent compromising of the respiratory pattern was taken into account, and it was decided to keep the child intubated in the neonatal ICU, to be re-evaluated in 24 hours. For post-operative medication, Cefoxitin was used for 10 days, and Dexamethasone for 8 days with gradual reduction.
The first post-operative day, there was a significant oedema of the tongue, which was partially insinuated outside the oral cavity, which confirmed the temerity of risk of immediate extubation. Child extubation occurred on the third post-operative day, when oedema reduction was compatible with maintaining the child’s breathing with ambient air.
Child was maintained on diet by nasogastric tube for 7 days. After this period a liquid oral diet was started, assisted by phonoaudiology, with maneuvers to improve the suctioning efficiency during breastfeeding. Patient was discharged on the 13th post-operative day.
Patient was monitored by the paediatric team for 20 months without signs of relapse or any associated complications.
Discussion
In the present case, the neonatology team noticed an important congenital volume increase in the floor of mouth soon after delivery. Later on, it was diagnosed as a plunging ranula. Most plunging ranula cases were reported in patients younger than 30-year-old, but the occurrence in paediatric patients are rare [1]. The aetiology of such retention cysts is described as arising from trauma or surgery on the floor of the mouth [1]. The cause of the neonatal ranula is still unknown [2].
In the present case, the infant had difficulty in breastfeeding, probably due to the posterior projection of the tongue, which also caused respiratory difficulty (perceived during feeding). If left untreated, ranula may increase in size and cause difficulties in breathing and swallowing [3,4].
CT scan showed an extensive cystic-like lesion on the floor of the mouth, displacing the tongue of the newborn posteriorly and upwards.
Many surgical techniques for treating ranulas are described, including excision of the lesion (with or without excision of the ipsilateral sublingual gland), cryosurgery, laser excision and marsupialization [2]. A search of the Medline database was performed through the Pubmed platform in April 2019 using the terms “ranula” and “neonate”, resulting in 44 articles. After reviewing the titles and abstracts of the articles, 14 were excluded because they were not the cases of congenital ranula. Eight articles that did not provide the abstract could not be found. The 22 included articles and the present neonatal ranula case with the corresponding treatments are shown on [Table/Fig-5] [2,5-25].
Review of the reported neonatal ranula cases and their treatments [2,5-25].
| Authors (publication year) | Age of infant | Treatment | Prognosis |
|---|
| Redpath TH (1969) [5] | 7-day | Marsupialization. | No recurrence |
| Constantinides CG et al., (1982) [6] | 15-day | 14 patients presented as neonates. Ranulas excised. | No recurrence |
| Bailey BM (1982) [7] | 3-month | Excision. | No recurrence |
| Steelman R (1998) [8] | 1-day | Spontaneous regression. | No recurrence |
| Fernandez Moya JM et al., (1998) [9] | Newborn | Aspiration puncture and excision after 30 days. | No recurrence |
| Amin MA and Bailey BM, (2001) [10] | Patient 1: 3-monthPatient 2: 2-day | 2 patients. Decompression. | No recurrence |
| Saheeb BD (2001) [11] | Newborn | Marsupialization. Excision after recurrence. | No recurrence |
| Onderoglu L et al., (2003) [12] | Newborn | Aspiration puncture and excision after 27 days. | No recurrence |
| Kolker MT et al., (2004) [13] | Newborn | Aspiration puncture. | No recurrence |
| Haberal I et al., (2004) [14] | 17-day | Excision. | No recurrence |
| Akyol MU and Orhan D, (2004) [15] | Newborn | Aspiration when newborn and excision after 6 weeks, | No recurrence |
| Drost B and Tytgat GA, (2005) [16] | Newborn | Spontaneous regression. | No recurrence |
| Chan DF et al., (2006) [17] | Newborn | Aspiration puncture and excision after 19 days. | No recurrence |
| Gul A et al., (2008) [18] | 2-day | Excision. | No recurrence |
| Zhi K et al., [2] | Patient 1: 3-dayPatient 2: 3-dayPatient 3: 1-monthPatient 4: 2-monthPatient 5: 7-dayPatient 6: 1-monthPatient 7: 2-monthPatient 8: 3-monthPatient 9: 4-monthPatient 10: 3-dayPatient 11: 7-day | 11 patients: Excision in 7, marsupialization in 2 and aspiration in 2. | No recurrence |
| Rosow DE et al., (2009) [19] | Patient 1: 5-monthPatient 2: 1-month | 2 patients: Simple sialodochostomy (excision of the imperforate sublingual caruncle) with cyst decompression. | No recurrence |
| Marques MI et al., (2010) [20] | 3-day | Drainage and marsupialization. | No recurrence |
| Licéaga R et al., (2010) [21] | Patient 1: 2-monthPatient 2: 2-monthPatient 3: 1-month | 3 patients: Marsupialization in 2 and excision in 1. | No recurrence |
| Singh GB et al., (2013) [22] | Newborn | Excision. | No recurrence |
| Soni A et al., (2013) [23] | 1-day | Aspiration puncture. | No recurrence |
| George MM et al., (2015) [24] | 37 weeks of gestation | Prenatal aspiration puncture via ultrasonography. Post-natal marsupialization and excision of the contralateral pseudocyst. | No recurrence |
| Mneimneh S et al., (2016) [25] | 4-month | Excision. | No recurrence |
| Paz et al., (2019) (present study) | 19-day | Excision. | No recurrence |
Initial therapeutic proposal in the present case was the marsupialization of the lesion. However, in the trans-operative period, initial inspection and manipulation of the lesion demonstrated that the distance from the surface of the floor of mouth mucosa to the lesion surface, would make it difficult to perform the marsupialization. Surgical team changed the initial therapeutic orientation, performing the peripheral dissection of the ranula, as it was possible to remove the lesion as a whole. The lesion was dissected laterally and posteriorly to the base of the tongue. There were no haemorrhagic intercurrences.
Another reason for the alteration of the initial therapeutic plan was the high rate of recurrence of ranula when submitted to marsupialization [26-28]. Surgical manipulation in the newborn’s oral cavity is not an easy task, considering the difficulty in accessing the airway (orotracheal intubation) and risk of extubation during surgery [27]. Thus, to perform a surgical procedure with lower chances of recurrence, seems to be an appropriate decision for this case.
Considering the area of dissection and knowing that hematoma and oedema in the post-operative period could compromise the airway permeability of the child, it was decided to maintain the newborn under orotracheal intubation in the neonatal intensive care. This conduct also proved to be adequate, as the child developed an important tongue oedema in the post-operative period. If the child had been extubated in the immediate post-operative period, he could have suffered significant respiratory problems. In addition, it is known that the difficulty of intubating a patient, especially a newborn, during emergency conditions with respiratory insufficiency and with large lingual volume [27].
The child was extubated on the third post-operative day, with the significant reduction in oedema and the possibility of maintenance of breathing with ambient air without orotracheal tube. In subsequent consultations it was verified that the child had a good clinical evolution, recovering the respiratory and digestive function.
Conclusion
Decision-making and surgical manipulations in lesions involving the floor of the mouth of newborns are not frequent and should be very well planned considering the risks of recurrence, risks of compromising airway permeability in the trans and post-operative periods, and therefore should be performed by teams experienced in approaching such lesions in paediatric patients. Excision of the ranula and maintenance of intubation until the reduction of post-operative oedema prevented intercurrences in the post-operative period and allowed a good clinical evolution of the child who recovered his respiratory and digestive function.
[1]. Mahadevan M, Vasan N, Management of pediatric plunging ranulaInt J PediatrOtorhinolaryngol 2006 70(6):1049-54.10.1016/j.ijporl.2005.10.02216356556 [Google Scholar] [CrossRef] [PubMed]
[2]. Zhi K, Wen Y, Ren W, Zhang Y, Management of infant ranulaInt J PediatrOtorhinolaryngol 2008 72(6):823-26.10.1016/j.ijporl.2008.02.01218387677 [Google Scholar] [CrossRef] [PubMed]
[3]. Baurmash HD, Marsupialization for treatment of oral ranula: a second look at the procedureJ Oral Maxillofac Surg 1992 50(12):1274-79.10.1016/0278-2391(92)90226-P [Google Scholar] [CrossRef]
[4]. Chai RL, Ozolek JA, Branstetter BF, Mehta DK, Simons JP, Congenital choristomas of the oral cavity in childrenLaryngoscope 2011 121(10):2100-06.10.1002/lary.2175821826675 [Google Scholar] [CrossRef] [PubMed]
[5]. Redpath TH, Congenital ranulaOral Surg Oral Med Oral Pathol 1969 28(4):542-44.10.1016/0030-4220(69)90262-X [Google Scholar] [CrossRef]
[6]. Constantinides CG, Davies MR, Cywes S, Intralingual cysts of foregut originS Afr J Surg 1982 20(3):227-32. [Google Scholar]
[7]. Bailey BM, A detached bronchogenic cyst occurring in the tongue of a neonateBr J Oral Surg 1982 20(4):288-93.10.1016/S0007-117X(82)80025-5 [Google Scholar] [CrossRef]
[8]. Steelman R, Weisse M, Ramadan H, Congenital ranulaClin Pediatr (Phila) 1998 37(3):205-06.10.1177/0009922898037003099545611 [Google Scholar] [CrossRef] [PubMed]
[9]. Fernandez Moya JM, Cifuentes Sulzberger S, Díaz Recaséns J, Ramos C, Sanz R, Perez Tejerizo G, Antenatal diagnosis and management of a ranulaUltrasound Obstet Gynecol 1998 11(2):147-48.10.1046/j.1469-0705.1998.11020147.x9549845 [Google Scholar] [CrossRef] [PubMed]
[10]. Amin MA, Bailey BM, Congenital atresia of the orifice of the submandibular duct: a report of 2 cases and reviewBr J Oral Maxillofac Surg 2001 39(6):480-82.10.1054/bjom.2001.067211735147 [Google Scholar] [CrossRef] [PubMed]
[11]. Saheeb BD, Recurrent congenital bilateral ranula: a case reportSADJ 2001 56(8):366-68. [Google Scholar]
[12]. Onderoglu L, Saygan-Karamürsel B, Deren O, Bozdag G, Tekşam O, Tekinalp G, Prenatal diagnosis of ranula at 21 weeks of gestationUltrasound Obstet Gynecol 2003 22(4):399-401.10.1002/uog.20714528477 [Google Scholar] [CrossRef] [PubMed]
[13]. Kolker MT, Batti JS, Schoem SR, The ex utero intrapartum treatment procedure for congenital ranula in a Jehovah’s WitnessOtolaryngol Head Neck Surg 2004 130(4):508-10.10.1016/j.otohns.2003.09.01015100657 [Google Scholar] [CrossRef] [PubMed]
[14]. Haberal I, Göçmen H, Samim E, Surgical management of pediatric ranulaInt J Pediatr Otorhinolaryngol 2004 68(2):161-63.10.1016/j.ijporl.2003.09.01714725982 [Google Scholar] [CrossRef] [PubMed]
[15]. Akyol MU, Orhan D, Lingual tumors in infants: a case report and review of the literatureInt J Pediatr Otorhinolaryngol 2004 68(1):111-15.10.1016/j.ijporl.2003.08.05214687694 [Google Scholar] [CrossRef] [PubMed]
[16]. Drost B, Tytgat GA, [Diagnostic image (229). A neonate with a sublingual swelling]Ned Tijdschr Geneeskd 2005 149(9):462 [Google Scholar]
[17]. Chan DF, Lee CH, Fung TY, Chan DL, Abdullah V, Ng PC, Ex utero intrapartum treatment (EXIT) for congenital giant ranulaActa Paediatr 2006 95(10):1303-05.10.1080/0803525060058054516982507 [Google Scholar] [CrossRef] [PubMed]
[18]. Gul A, Gungorduk K, Yildirim G, Gedikbasi A, Ceylan Y, Prenatal diagnosis and management of a ranulaJ Obstet Gynaecol Res 2008 34(2):262-65.10.1111/j.1447-0756.2008.00767.x18412794 [Google Scholar] [CrossRef] [PubMed]
[19]. Rosow DE, Ward RF, April MM, Sialodochostomy as treatment for imperforate submandibular duct: a systematic literature review and report of two casesInt J Pediatr Otorhinolaryngol 2009 73(12):1613-15.10.1016/j.ijporl.2009.03.00719380165 [Google Scholar] [CrossRef] [PubMed]
[20]. Marques MI, Morais S, Coutinho S, de Castro O, Rei AI, [Congenital ranula]Acta Med Port 2010 23(5):937-40.Epub 2010 Oct 22 [Google Scholar]
[21]. Licéaga R, González C, Licéaga C, Vargas G, Congenital ranulaJ Clin Pediatr Dent 2010 34(3):263-66.10.17796/jcpd.34.3.n3t6x8148g1756vl [Google Scholar] [CrossRef]
[22]. Singh GB, Rai AK, Arora R, Garg S, Abbey P, Shukla S, A rare case of congenital simple cystic ranula in a neonateCase Rep Otolaryngol 2013 2013:84193010.1155/2013/84193024083044 [Google Scholar] [CrossRef] [PubMed]
[23]. Soni A, Suyal P, Suyal A, Congenital ranula in a newborn: a rare presentationIndian J Otolaryngol Head Neck Surg 2012 64(3):295-97.10.1007/s12070-011-0371-y23998039 [Google Scholar] [CrossRef] [PubMed]
[24]. George MM, Mirza O, Solanki K, Goswamy J, Rothera MP, Serious neonatal airway obstruction with massive congenital sublingual ranula and contralateral occurrenceAnn Med Surg (Lond) 2015 4(2):136-39.10.1016/j.amsu.2015.04.00625984300 [Google Scholar] [CrossRef] [PubMed]
[25]. Mneimneh S, Barazi R, Rajab M, A rare case of congenital ranula in an infantCase Rep Otolaryngol 2016 2016:587459510.1155/2016/587459527313929 [Google Scholar] [CrossRef] [PubMed]
[26]. Lee DH, Yoon TM, Lee JK, Lim SC, Treatment outcomes of the intraoral approach for a simple ranulaOral Surg Oral Med Oral Pathol Oral Radiol 2015 119(4):e223-25.10.1016/j.oooo.2015.01.00725758846 [Google Scholar] [CrossRef] [PubMed]
[27]. McAllister JD, Gnauck KA, Rapid sequence intubation of the pediatric patientFundamentals of practice. Pediatr Clin North Am 1999 46(6):1249-84.10.1016/S0031-3955(05)70185-1 [Google Scholar] [CrossRef]
[28]. King RC, Smith BR, Burk JL, Dermoid cyst in the floor of the mouth. Review of the literature and case reportsOral Surg Oral Med Oral Pathol 1994 78(5):567-76.10.1016/0030-4220(94)90166-X [Google Scholar] [CrossRef]