The most preferred anaesthetic technique for elective as well as unplanned caesarean sections is spinal anaesthesia and the most important adverse effects of it is bradycardia and hypotension, which is determined by the block height.
The commonly practiced position while performing spinal anaesthesia is either left lateral decubitus or sitting position. After the procedure, when the parturient is placed in supine position, the aorto-caval compression by gravid uterus reduces the maternal cardiac output which may exacerbate to cause hypotension with the sympathetic blockade [1]. Many studies found that a modified head elevation position can prevent a higher spread of block height and maintaining haemodynamic stability. The position in which parturients are made to lie down in left lateral position with three pillows under the head and two pillows under the shoulder is called as Oxford position. Oxford position was described by Carrie to prevent problems of aortocaval compression and unpredictable spread of spinal block. It is called as Oxford position because it was more commonly used at Oxford University [2]. Oxford position further reduces the cephalic spread of a local anaesthetic and the aorto-caval compression at the time when compensatory mechanisms are developing [3].
Even though there are many studies, the scope of Oxford position needs to be evaluated as this position is less in practice and in similar studies combined spinal-epidural was given for LSCS. In the present study, we evaluated under only subarachnoid block in order to know the failure rate in oxford position.
Materials and Methods
The randomised controlled study was conducted on parturients who underwent caesarean section under spinal anaesthesia, from study period January 2017 to August 2018. The Ethical committee approved the research protocol (INSTEC/EC/157/2016-17). Parturients were randomly allocated into two groups of 50 each, group L and O by closed envelope method. In group L, parturients were placed in lateral position with one pillow supporting the head. In group O, parturients were placed in lateral position with three pillows supporting the head and two pillows under the shoulder (Each firm pillow height of 10 cm).
Inclusion criteria: All parturients belonging to the American Society of Anaesthesiologists Physical Status (ASA PS) II, aged from 18-45 yrs, undergoing a caesarean section were included in the study.
Exclusion criteria: Parturients who had any contraindications to regional anaesthesia, spine abnormality, body weight <45 kg and >100 kg, body mass index >30, intrauterine growth retardation, pregnancy-induced hypertension, gestational diabetes, multiple gestations, fetal distress were excluded from the study.
After institutional ethics committee clearance, parturients were evaluated and written informed consent was taken. Parturients were kept nil per oral as per standard protocol.Inj.metoclopromide10 mg and Inj.ranitidine 50 mg was given prior to surgery in both elective and emergency caesarean section.
After shifting the patient to the Operation Theatre (OT), Electrocardiography (ECG), pulse-oximeter (Spo2) and Non-invasive Blood Pressure (NIBP) monitor were connected. Baseline values {(Systolic Blood Pressure (SBP), Diastolic blood pressure (DBP), Mean Arterial Pressure (MAP) and Heart Rate (HR)} were noted.
After positioning, SBP, DBP, MAP and HR were recorded. Oxygen supplementation was given at the rate of 5L/min via face mask.
Lumbar puncture was performed via midline approach at L3-L4/ L4-L5 interspinous space. When free flow of Cerebrospinal Fluid (CSF) was confirmed, 12.5 mg of 0.5% hyperbaric bupivacaine was injected into the subarachnoid space over 30s using 25 QB needle (standardised) [4].
After injecting the drug in group L, parturients were repositioned to supine and in group O, parturients were repositioned to supine with three pillows continuing to support under the head and two pillows under the shoulder, until the end of surgery. Surgeons were requested to wait at least for 10 minutes before incision (the mean time to achieve T6 analgesia with 12.5 mg hyperbaric 0.5% bupivacaine injected in the lateral position is from 3.3/4-8 minutes [4].
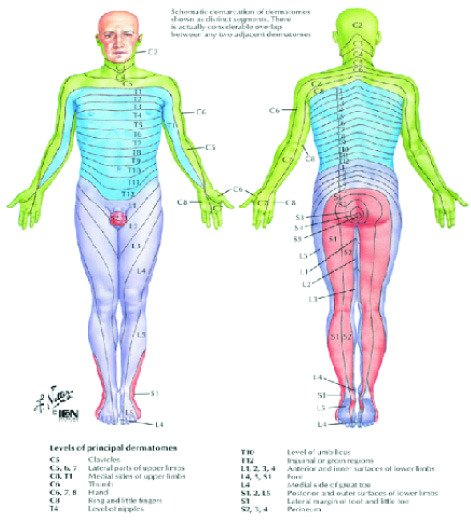
Blood pressure (SBP, DBP, MAP) and heart rate was recorded throughout the procedure and the required ephedrine dose was also to be recorded. Sedation was standardised for all the parturients whoever had discomfort with inj fentanyl 1 mcg/kg and inj midazolam 0.02 mg/kg. The measurement of sensory level based on below picture and motor blocked was based on bromage scale [Table/Fig-1]. Patient distribution is shown in [Table/Fig-2].
Sensory dermatomes.
Image source: Science Direct.Com; Sensory dermatomes were numbered accordingly
L5-1, L4-2, L3-3, L2-4, L5-5, T12-6, T11-7, T10-8, T9-9, T8-10, T7-11, T6-12, T5-13, T4-14, T3-15, T2-16, T1-17
Flowchart of patients enrolled and analysed in two groups.
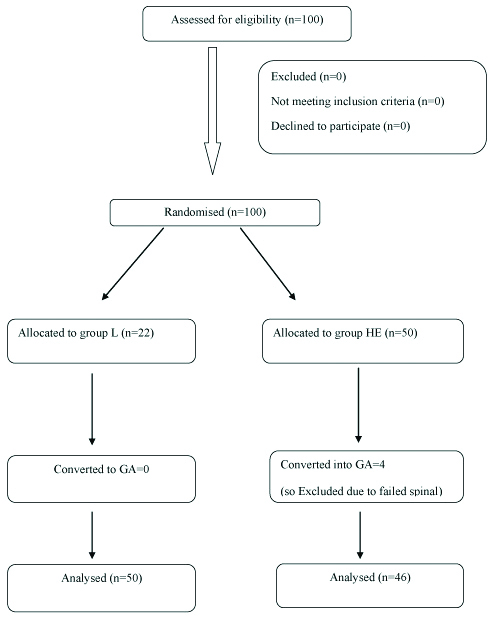
In either group, when adequate block was not achieved (i.e., to reach the T6 segment block within 20 minutes of interthecal injection), general anesthesia was induced and surgery was started. Parturient were shifted to Post Anaesthesia Care Unit (PACU) after the completion of procedure where further care of the patients was taken.
Sample size: To compute sample size, the study which was done in Korea by Lee MH et al., was taken as a reference and the technique of estimating the difference between two means using a formula [5]:
n= Z2-α/2{2(Sp)2}\d2
Sp2=S12+S22/2=(21)2+(27)2/2=585
n=(1.96)2{2×585}/15×15=19.97≈20whereas:
S1=SD in first group
S2=SD in second group
α=Level of significance (5%)
Sp=Pooled standard deviation (which is summation of SD of first group and SD of second group i.e., S12+S22/2)
d=Precision (15%)
According to formula, estimated total sample size was total=40 parturients. However, as per institutional ethics committee recommendations, sample size was increased to total of 100. It was done by using design effect i.e., 20×5=100, which was divided into 50 in each group.
The collected data was entered in Microsoft Excel. Data analysis was done using SPSS software version 16. The univariate analysis was done for anthropometric measurements and vitals which were shown using frequency, percentages, mean and standard deviation. Independent t-test used to find the difference in between mean. The p-value <0.05 was taken significant.
Results
Four parturients were excluded from the study as spinal anaesthesia failed to act in group O (Oxford position) due to difficulty in practicing different position rather than conventional lateral. Demographic data are presented in [Table/Fig-3] and did not differ significantly between the two groups. The characteristics of the sensory blocks are presented in group O and group L [Table/Fig-4]. The length of time from spinal injection to T6 sensory block and achievement of Maximum Sensory Block Level (MSBL) were shorter in group L than in group O. Longer interval was required to reach T6 sensory block in group O, leading to increased length of time for spinal injection to surgical incision, delivery and surgery completion in this group. MSBL was also higher in group L than in group O {12 (T4) versus 10 (T6), p=0.0015}. However, the length of time to TSR of the sensory level was significantly differing between the two groups. Incidences of hypotension and the amount of ephedrine administered before and after achieving sensory block to T6 were significantly higher in group L. The number of dermatomes blocked were greater in group L than in group O during the 30 minutes following spinal injection.
| Group O | Group L | p-value |
|---|
| Age (years) | 28.67±-3.621 | 28.82±4.074 | 0.854 |
| Weight (kg) | 63.89±8.306 | 62.53±8.591 | 0.431 |
| Height (cm) | 156.59±4.745 | 155.56±5.257 | 0.319 |
| Body mass index (BMI) | 25.559±4.5014 | 25.751±3.1143 | 0.808 |
Characteristics of sensory block in group O and group L.
| Group O | Group L | p-value |
|---|
| Time to achieve T6 (min) | 9.52±1.560 | 5.57±0.821 | <0.0001 |
| Time to incision (min) | 13.15±2.022 | 10.60±1.457 | <0.0001 |
| Time to achieve MSBL (min) | 12.15±2.366 | 8.98±1.801 | <0.0001 |
| Time to TSR sensory (min) | 111.30±11.077 | 124.10±7.934 | <0.0001 |
| Time to completion of surgery (min) | 84.17±6.668 | 75.06±10.375 | <0.0001 |
| Total ephedrine requirement (mg) | 10.92±8.458 | 3.57±11.26 | <0.0001 |
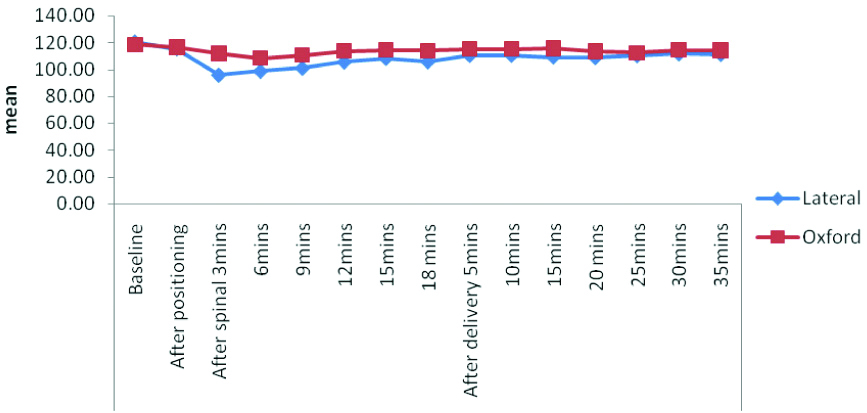
[Table/Fig-5,6] shows changes in MAP and HR after spinal injection. In group L, MAP decreased more than 20% compared to baseline at 3,6 and 9 mins till 20 mins after spinal injection. HR did not significantly differ between the groups. In this study, most of the parturients in the Oxford group had pain during exteriorization of uterus hence requirement of sedation was present. 4 out of 50 parturients (8%) in Oxford Group, due to failed spinal anaesthesia, got converted into general anaesthesia.
Comparison between the two groups in terms of heart rate.
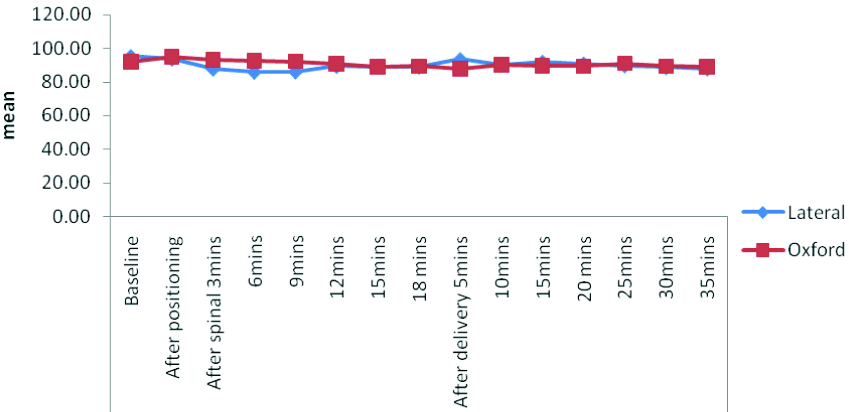
Comparison between the two groups in terms of mean blood pressure.
For reference, [Table/Fig-7] enumerates the parameters that were studied in the parturients.
Parameters measured between the two groups.
| Time to achieve T6: it is the time measured from the time of spinal given to time of T6 block achieved |
| Time to incision: time of spinal given to time of surgical incision |
| Time to achieve MSBL (Maximum sensory block eve): time of spinal given to time when maximum block achieved i.e., above T6 |
| Time to TSR (Two segment resessive) sensory: from the time of spinal to time of decrease in two segment sensory level |
| Time to completion of surgery: from the time of spinal given to time of completion of surgery |
Discussion
The conventional lateral position is most commonly used in lower segment cesarean section and level of the block in this is not predictable which lead to higher risk of severe hypotension and bradycardia [5]. In the Oxford position, due to prevention of the cephalic spread of a local anaesthesia above mid-thoracic region T3-4 and also by minimising aorto-caval compression leads lesser risk of hypotension and bradycardia [5].
Hence, this study was conducted to determine whether Oxford position during spinal anaesthesia produces adequate sensory and motor block height while maintaining haemodynamic stability for caesarean section.
The present study, found that sensory and motor blockade achieved was faster in lateral position compared to Oxford position as there was slower onset of blockade with a limited spread in Oxford position. Hence, haemodynamic stability was well maintained in Oxford position compared to lateral position.
In this study, it was found that there were significant changes in the haemodynamic parameters i.e., SBP, DBP, MAP and HR (p<0.0001) intraoperatively. There was a significant decrease in the time required to reach peak sensory blockade in the lateral group compared to Oxford group (p<0.0001) as a result, the incidence of hypotension was more in case of the lateral group. The onset of motor blockade was significantly faster in lateral as compared to the Oxford group. Even the requirement of ephedrine was more in case of lateral group compared to Oxford group (p<0.0001). Due to the slower onset of block level, Oxford position had an advantage of less haemodynamic instability. The duration of analgesia was significantly prolonged in the lateral group compared to Oxford group which was determined by TSR; found to be more in lateral position (p<0.0001).
It was found that in caesarean section, maintaining the head elevated position, is better compared to the lateral to supine position, as it is associated with appropriate sensory block height, with a gradual onset and improved haemodynamic stability [5,6].
It was so found that the Oxford position slowed the onset of the sensory block due to an elevation of the upper thoracic vertebra and time to achieve T5 sensory block and maximum sensory block level was fastest in lateral as compared to the Oxford position which was also similar to present study results. Due to which incidence of hypotension was also more in the lateral, compared to Oxford position [7-9].
Elfil H et al., studied the effects of the Oxford Head Elevating Laryngoscopy Pillow (O/HELP) on subarachnoid local anaesthetic spread in elective Caesarean section. Parturients were assessed for adequacy of sensory block (T6 or higher) at 10 minutes and requirement of epidural top-up or conversion to general anaesthesia. They found that the discomfort were higher in the intervention group hence requirements for epidural top-up or conversion to general anaesthesia was more in O/HELP parturients due to increased incidence of subarachnoid block failure, which was similar to present study whereas 4 out of 50 parturients had an inadequate block, it was converted into general anaesthesia [10].
Limitation
The limitation of this study was inability to achieve adequate block upto T4 which leads to discomfort during exteriorization of the uterus in the parturients, but it was adequately managed with mild sedation. In other studies in case if maximum sensory block level of T6 was not achieved, epidural supplement were given as they choose the combined spinal-epidural technique [5-8]. In this study, the maximum sensory block heights of T6 were not achieved in 4 cases and these were converted to general anaesthesia.
Conclusion
Results of this study showed that the adequacy of sensory, motor block achieved and haemodynamic changes with Oxford position in spinal anaesthesia for caesarean section was better compared to lateral position, due to an elevation of mid-thoracic vertebrae, higher level blockade was prevented, as a result severe hypotension and bradycardia were prevented.