A pulpotomy is performed on primary teeth that have extensive decay, or when caries removal would result in further carious or mechanical pulp exposure. The success rate of pulpotomy treatments depends on the correct diagnosis through a good dental history, a thorough clinical and radiographic examination, the sealing ability of the final restoration after treatment and the appropriate use of a pulpal medicament [1,2].
The ideal pulpotomy medicament would be bactericidal with biocompatibility, and does not interfere with the physiologic root resorption process [3]. The international standard for pulpotomy medicament that has been used for long time with a high success rate is Buckley’s formocresol, but its cytotoxicity, mutagenicity, genotoxicity and immunotoxic properties have recently raised concerns [4-6]. A wide range of materials have been studied as a pulpotomy medicament, including formocresol, glutaraldehyde, ferric sulphate, calcium hydroxide and Mineral Trioxide Aggregate (MTA). Several studies have reported that the clinical success rate of formocresol pulpotomy treatment gradually decreases with time due to chronic inflammation and necrotic pulp tissue [1,5]. Therefore, other materials have been proposed to replace formocresol.
In recent years, Calcium silicate based cements, such as MTA have been developed. It is a biocompatible and bioinductive which defined as a material that has the effect on or eliciting a response from living tissue, organisms or cell such as inducing the hydroxyapatite or in pulp therapy, induce dentine bridge formation in pulp treatment [7]. The ideal properties of bioactive material are; it should be bactericidal and bacteriostatic, sterile, stimulate reparative dentine formation and maintain pulp vitality [7]. MTA has been used in many dental applications such as endodontic treatment, endodontic repair, and as a pulp capping material. According to several authors, MTA offers excellent clinical and radiographic outcome as compared to formocresol [8,9]. A recent meta-analysis of 30 clinical articles from 7 databases reported the success rate of MTA and FC to be 95% ad 87% respectively [10]. Portland cement is a new calcium silicate-based cement which is packaged as power and liquid. Its distinguished biological properties have led to the development of Biodentine (Septodont, St. Maurdes-Fosses, France). The composition of powder includes tricalcium silicate, calcium bicarbonate and zirconium oxide. The liquid component is comprised of water, calcium chloride (to speed up setting) and modified polycarboxylate (superplactisizer). Liquid and powder are mixed in single measure dispensed in capsule with mixing device for 30s [11]. The biological properties of biodentine include- high biocompatibility, bioactivity of calcium silicates, enhanced rapid setting times conferred by calcium chloride and high strength by low water-cement ratio [12].
Biodentine was introduced in dentistry after becoming commercially available in 2009 (Septodont Ltd.,). It is a calcium-silicate that is formulated using the MTA-based cement technology, but the physical and chemical properties of these types of cements were improved, adding higher viscosity, greater ease of handling, shorter setting time [13]. It has been proved that biodentine has antibacterial properties due to its high pH, and it can stimulate dentine bridge formation [11,14].
There are few in vitro studies that have evaluated the use of biodentine in pulpotomy treatment in animal teeth. Their result showed hard tissue formation in primary pig teeth after 90 days in all samples [15]. Another in vitro investigation was done in human molars using tomographic evaluation revealed promising results of biodentine as a pulpotomy medication in primary teeth but in Thailand, this type of study are still limited [16].
The present study was aimed to evaluate the clinical and radiographic success rate in primary molars using biodentine and formocresol. Result demonstrated that biodentine showed the greatest thickness of dentine bridge formation in comparison with MTA and other material [16]. These properties make biodentine a possible choice for use as a pulp dressing agent for pulpotomy in primary molars. Even though, there are some clinical studies in many countries molars between biodentine and formocresol through 12 months follow-up in Thai children. The proposed hypothesis was that the clinical and radiographic success rates after 6 and 12 months between biodentine and formocresol pulpotomy are not different.
Materials and Methods
This parallel design single blinded randomised control trial was conducted and performed in the department of paediatric dentistry, Mahidol University and Phatthalung province, Thailand between September, 2016-November, 2018. A statistician consultation was carried out before a sample size calculation based on previous studies (Nowicka A et al., and Sonmez D et al., [16,17]) with two sided type I error 5% and 90% power of test. Sample size was calculated based on McNemar test by the Query Advisor program (Statistical Solution). A minimum of 21 children were required to detect a significant difference. The total number of subjects required was calculated as 25 in each group in order to make up for lost cases (20%) while the study was being conducted.
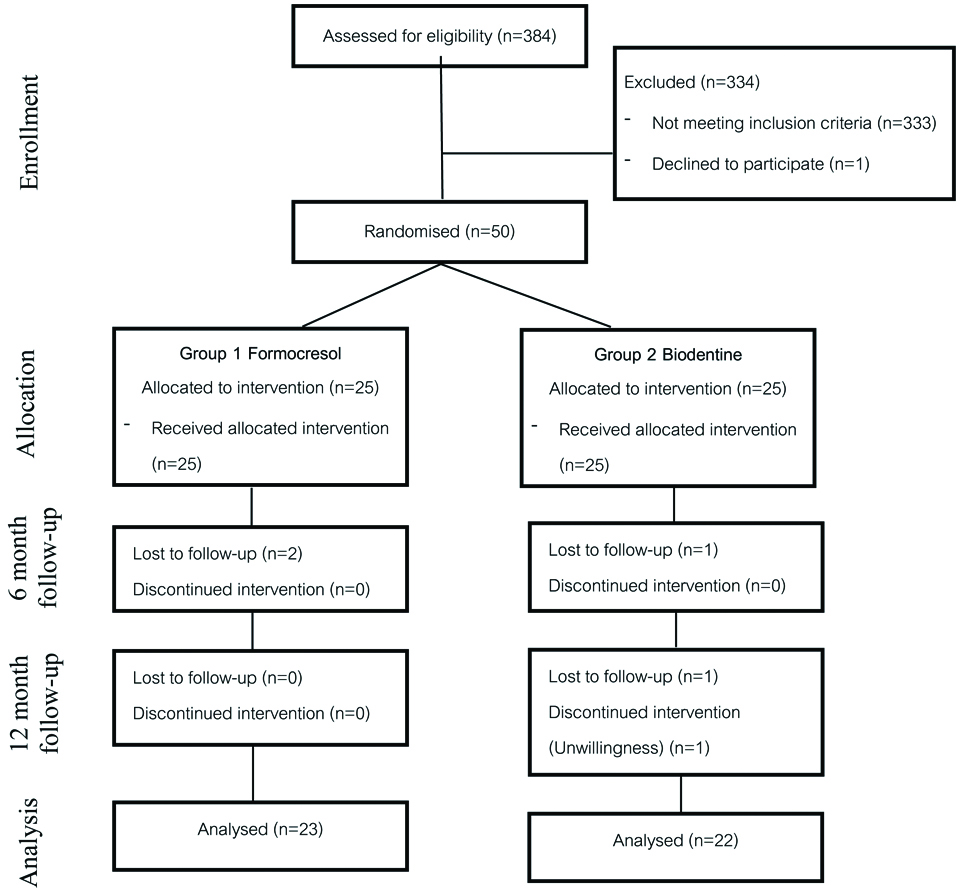
Faculty of Dentistry and Faculty of Pharmacy, Mahidol University’s Ethical Institutional Review Board (MU-DT/PY-IRB 2016/044.1509), approved this study; CTRN: TCTR20181115015 (Clinical Trial Registration Number). A total of 50 teeth in 38 children (aged 3-8 years) were selected after screened by clinical and radiographic examination and met the inclusion criteria. Written informed consents were obtained from parents/legal guardians. All subjects were allowed to voluntarily quit from the study at any point of time without affecting their dental treatment [Table/Fig-1].
Flow diagram of the participants in the study.
Subject Selection
Subjects were conveniently selected based on their need for restorative dental treatments from patients who came to the paediatric dental clinics using a random sampling by giving each individual with a number and then used a table of random number. The study was performed on the primary molars of Thai children aged three to eight-year-old. A total of fifty teeth from 38 children were selected for inclusion.
Inclusion Criteria
The patients who: 1) were in good general health; 2) had a deep carious primary molar with no history of pain, or only intermittent pain due to a stimulus such as when chewing food or through having food stuck in the decayed tooth; 3) had no clinical evidence of irreversible pulpitis or pulp necrosis, such as pulp exposure, the swelling of soft tissue or fistula and sinus track, or abnormal tooth mobility; and 4) there was no radiographic evidence of irreversible pulpitis or pulp necrosis, such as internal resorption, inter-radicular bone destruction, pathology in the periapical area, and the roots remained more than 2/3 of the normal root length.
Exclusion Criteria
The tooth has: 1) an unrestorable crown; 2) no exposed pulp after the removal of carious was complete; and 3) inflammation had extended into the radicular pulp, or the pulp had necrosis, and after removal, the coronal pulp had no haemostasis that could be obtained using moistened cotton pellets within 5 minutes.
Calibration of Examiners
The calibration was performed for radiographic examinations. The inter-examiner calibration was done by randomly interpreting 20 radiographs by two separate experts. Two readers determined the root length, lamina dura, Periodontal Ligament (PDL) space, radiolucency, pathologic root resorption, internal root resorption and pulp obliteration. Measured inter-examiner reliability gave a result that showed the mean Kappa statistic between two readers is 0.863, which is an excellent agreement.
Intervention
Teeth were assigned to one of the two treatment groups using the simple random sampling method (random table) with 25 in each group. If the child had two teeth from the contralateral site which met the inclusion criteria, one site was randomly assigned and the remaining site was automatically assigned to the other group. The procedure was done in step-by-step manner after giving local anaesthesia and rubber dam isolation. The cavity outline form was established and caries was excavated. Pulpotomy was carried out if removal of soft caries revealed pulp exposure or if on close inspection the pulp exposure was found. A #330 high-speed bur was used to remove the roof of the pulp chamber whereas a low speed carbide bur was used to remove the coronal pulp to a depth of 5-7 mm. Normal saline was used for irrigation of the pulp chamber, haemostasis was achieved through sterile cotton pellet by applying pressure to the amputated pulp stumps.
In the formocresol group (Group 1), Buckley’s formula, (a one-fifth dilution formulated at Mahidol University, Thailand) was used through applied cotton pellet moistened with formocresol for 5 minutes. The pulp was then covered with reinforced Zinc-oxide eugenol (IRM, DentsplyR, USA), and restored with a stainless steel crown. In the biodentine group (Group 2), the material was prepared following the manufacturer’s instructions by squeezing out the liquid, using 5 drops of a single dose container into a powder-containing capsule, which was mixed for 30 seconds and was further placed in to a mixing device at a speed of 4000-4200 rotations/minutes. The mixture was then placed into the pulp chamber to fill the cavity, and was left for 12 minutes, for the material to set before the tooth was restored with a stainless steel crown.
In Biodentine group (Group 2), the material was prepared following the manufacturer’s instructions by squeezing out the liquid, using 5 drops of a single dose container into a powder-containing capsule, which was then placed in a mixing device at a speed of 4000-4200 rotations/minutes, and was mixed for 30 seconds. The mixture was then placed into the pulp chamber to fill the cavity, and was left for 12 minutes for the material to set before the tooth was restored with a stainless steel crown.
Follow-up
The children were recalled for follow-up visit at 6 and 12 months after the treatment. Each follow-up visit included a clinical examination, which was performed by one expert (not the operator) who did not know the treatment group they belonged to. Periapical radiographs were taken for the radiographic evaluation at 6 and 12 months, which was performed by two expert readers (neither the operator nor the clinical examiner) who were blinded to the treatment group and clinical data. Preoperative radiograph and previous follow-up radiograph were provided to compare. The criteria for clinical failure were: 1) a history of pain after treatment; 2) gingival swelling or having a sinus tract; 3) tenderness to percussion or palpation; and 4) pathologic tooth mobility. The criteria for radiographic failure were: 1) furcation or periapical radiolucency; 2) pathologic external root resorption; and 3) internal root resorption.
Statistical Analysis
The inter-examiner reliability was calculated using Cohen’s kappa coefficient and analysed using the SPSS version 20. The differences between the clinical and radiographic success rates were analysed by the Chi-square test or the Fisher-exact test using SPSS version 20. The level of significance was set at p<0.05.
Results
A total of 50 primary molars were included in this study. Age, sex and type of primary molars treated in 2 groups showed no statistically significant differences [Table/Fig-2].
The baseline characteristics of subjects in both groups.
| Characteristics | Group 1 (Formocresol) | Group 2 (Biodentine) | p-value |
|---|
| Age (years) |
| Mean±Std. deviation | 5.33±1.13 | 5.24±1.17 | 0.192 |
| Male:Female | 10:13 | 13:11 | 0.556 |
| Maxillary teeth | 0.410 |
| First molar | 3 | 1 |
| Second molar | 1 | 2 |
| Mandibular teeth |
| First molar | 11 | 10 |
| Second molar | 10 | 12 |
At 6 months, 47 teeth were available to follow-up (formocresol=23, biodentine=24); At 12 months, an additional 2 teeth from biodentine group were lost due to patient relocation
Clinical and Radiographic Evaluation
The clinical success rate of both groups were equally 100% at the 6 and 12 months follow-up, and there was no statistical difference between these two groups (p=1.000). The radiographic success rate at 6 months of formocresol and biodentine groups were 65% and 79%, respectively. Other teeth were classified as either questionable or failure [Table/Fig-3]. At 6 months follow-up (p=0.237) there were no statistically significant difference with the radiographic success rate between the two groups. The percentage of radiographic evaluations in both groups is shown in [Table/Fig-3].
The Radiographic success rate in both groups at 6 and 12 months follow-up.
| Radiographic | | Groups | |
|---|
| Evaluation | | Formocresol | Biodentine | p-value |
|---|
| 6 months | Success | 15 (65.2%) | 19 (79.2%) | 0.237 |
| Questionable | 3 (13.1%) | 4 (16.7%) |
| Failure | 5 (21.7 .0%) | 1 (4.2%) |
| Total | 23 (100%) | 24 (100%) | |
| 12 months | Success | 17 (73.9%) | 21 (95.5%) | 0.022* |
| Questionable | - | 1 (4.5%) |
| Failure | 6 (26.0%) | - |
| Total | 23 (100%) | 22 (100%) | |
| p-value | | 0.286 | 0.261 | |
*Statistically significant at the p<0.05
The radiographic evaluation of questionable teeth in both groups at 12 months follow-up showed one tooth from formocresol group was changed to radiographic failure, while 3 out of 4 radiographs in biodentine group were changed to success [Table/Fig-4], except for one tooth that was still questionable and required further follow-up.
The radiographic finding of biodentine and formocresol groups.
| Groups | |
|---|
| Radiographic finding | Formocresol (n=23) | Biodentine (n=22) | p-value |
|---|
| Pathologic root resorption* with periapical radiolucency | 3 (13.04%) | - | 0.233 |
| Periapical radiolucency | 1 (4.35%) | 1 (4.55%) | 1.000 |
| External root resorption | 1 (4.35%) | - | 1.000 |
| Pulp obliteration | 3 (13.04%) | 10 (45.45%) | 0.016† |
*Pathologic root resorption means external with or without internal root resorption, †: Statistically significant
There was a statistically significant difference in the radiographic success rate between 2 groups at 12 months (p=0.022). The radiographic findings in both groups are presented in [Table/Fig-4]. The most common radiographic finding in the formocresol group was external and internal root resorption with periapical radiolucency. Pulp obliteration in formocresol and biodentine groups were 13% and 45%, respectively which was statistically significant difference (p=0.016). Pulp canal obliteration was the most common radiographic finding in biodentine group, and this was not classified as a radiographic failure.
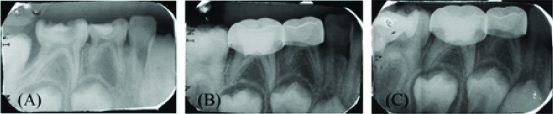
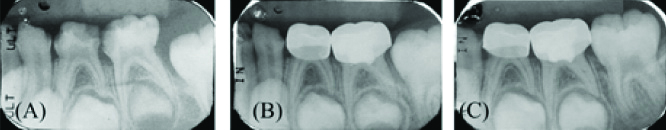
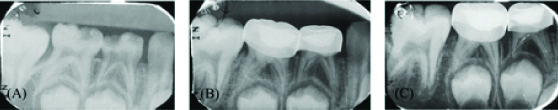
[Table/Fig-5,6 and 7] showing the Periapical radiographs which shows successful pulpotomy treatment at 6 months and 12 months follow-up.
Periapical radiographs showing a successful formocresol pulpotomy treatment of tooth 85: (a) Preoperative radiographs; (b) 6 months postoperative follow-up; (c) 12-month postoperative follow-up.
Periapical radiographs showing a successful biodentine pulpotomy treatment of tooth 75: (a) Preoperative Radiographs; (b) 6 months postoperative follow-up; (c) 12-month postoperative follow-up. The postoperative radiographs at 6-and 12-months follow-up showed signs of pulp obliteration.
Periapical radiographs showing a successful biodentine pulpotomy: (a) Preoperative radiograph; (b) At 6 months follow-up, tooth 85 was classified as questionable because of some area showed discontinuous lamina dura; (c) At 12-months postoperative follow-up was changed to radiographic success.
Discussion
Biodentine has proven to be a successful material in dentine replacement, and used for a wide range in endodontic treatment. The advantages of this material include less leakage, antimicrobial, biocompatibility, and can stimulate dentine bridge formation [14].
In this study, all pulpotomies were performed by one operator, who could not be blinded to the treatment group because the medicaments had to be carried to the pulp chamber. Instead, samples were randomly assigned. The clinical examinations during the follow-up periods were performed by another operator who did not know the group of the treatment. The radiographic interpretation was performed by two experts who blinded to the treatment groups, and they showed an excellent agreement Kappa index. Stainless steel crowns are considered to be the restoration method of choice after pulp treatment due to their durability and sealing ability [5,18]. After the pulpotomies treatment, the final restoration was performed using a stainless steel crown immediately to prevent any possible failure from any microleakage of the restoration, which could happen if the final restoration was delayed until a later visit. There are studies regarding the success rate of the formocresol pulpotomy, and they showed that immediate stainless steel crown after pulp treatment significantly affected the success rate of pulpotomy when compared with using the IRM as a temporary restoration and restoring the stainless steel crown in a later visit [5].
The clinical success rate of formocresol and biodentine in this study were 100% at 12 months for both groups, which is similar to previous studies which were all 100% [2,6,19-22]. None of the teeth had any symptoms or showed any sign of gingival inflammation, pus or other clinical signs of failure after one year.
The radiographic success rate at 6 months with both groups were 65% and 79%, respectively. This result was lower than other studies done at 6 months [2,17,21,23]. In a study, by Godhi B et al., 100% success with both the groups were seen clinically at 1, 3, 6 and 12 months. The radiographic success rates of formocresol and MTA were 92% and 96%, respectively at 3 months, and the radiographic success rates of formocresol and MTA were 88% and 96%, respectively at 6 and 12 months [2]. Previous study by Guven Y et al., showed the success rate of formocresol at 6 months follow-up was 76% [22]. Some radiographs were classified as questionable because it could not be deemed to be either a success or a failure, and these were then followed-up for later 6 months, which was different from other studies. The questionable groups showed some area of discontinuous lamina dura or a slightly widening of the periodontal ligament space, but there was an absence of other concurrent pathology which were 13% in the formocresol group, and 16% in the biodentine group. The radiographic success rates of formocresol and biodentine at 12 months were 74% and 95%, respectively. When compared with previous studies by Juneja P and Kulkarni S, who used the same evaluation criteria, the success rates were similar [21]. Even though there are other studies that showed higher success rates of formocresol pulpotomy than this study (82-84%) [2,6], the evaluation criteria were different. From the study done by Aeinehchi M et al., they did not define the internal root resorption as a radiographic failure [6], and the study by Godhi B et al., did not classify the pathologic root resorption as a radiographic failure [2]. These would affect a higher radiographic success rate than in this study.
In this study, there was no statistically significant difference in the clinical and radiographic success rates between two groups at 6 months follow-up, which is consistent with the study from Juneja P and Kulkarni S, [21]. However, in this study at 12 months follow-up showed statistically significant differences different from the study done by Juneja P and Kulkarni S, which showed no statistically significant difference in the radiographic success rate at this period [21].
The most common radiographic failure found in the formocresol group was pathologic root resorption with periapical radiolucency, which was not found in the biodentine group. Pulp canal obliteration was the most common radiographic finding in the biodentine group. Inflammatory root resorption is composed of both external and internal root resorption. Formocresol pulpotomized teeth were likely to have internal root resorption more than the calcium silicate based-cement [24,25]. Pathologic root resorption might be as a result of undiagnosed chronic inflammation existing in the radicular pulp prior to the pulpotomy treatment [26], or because of a technical failure while performing the treatment [25]. Internal root resorption resulted from odontoclastic activity, indicating that the teeth had vitality. Some studies found that internal root resorption was caused by an undiagnosed chronic inflammation existing in the radicular pulp prior to the pulpotomy treatment. Other causes of internal root resorption might occur because of the reversible fixative effect of formocresol [26], or the overstimulation of primary pulp tissue by the high pH of calcium hydroxide, leading to the formation of an odontoclast [27]. However, the internal root resorption is self-limiting, and this response is not considered a failure at the micro level [2]. Holan G et al., categorised failure only when the resorption reached the outer surface of the root, or presented clinical signs and symptoms [28]. In this study, the internal root resorption that coincided with external root resorption or periapical radiolucency was as a radiographic failure, which was found in 3 teeth (13%), which only in the formocresol group. Calcium silicate-based materials have a lower prevalence of internal root resorption than formocresol but this did not produce significant differences, which is consistent with the results of other studies [17,22].
Pulp canal obliteration is a result of odontoblastic activity and shows that with some degree of vitality, which was not considered as a failure [22,29,30]. The pulp obliteration in formocresol and biodentine groups were 13% and 45%, respectively. In other studies, pulp obliteration in formocresol pulpotomy ranged from 0 to 13% [17,30-32]. In biodentine, pulp obliteration ranged from 14 to 36% [22,23]. The results from this study found that the use of biodentine showed higher pulp canal obliteration, especially at the 12 months follow-up. Pulp canal obliteration is associated with the occurrence of dentine bridge formation; although no dentine bridges were observed in this study. This may be because all the teeth in the study were restored with preformed metal crowns, and any coronal pulp or the presence of a dentine bridge would be masked by the metal.
The histology of formocresol pulpotomy was different from that of biodentine even though both treatments were successful, they demonstrated atypical tissue reactions [33,34]. The area of chronic inflammation was usually observed in the pulp. The severity varied but was more severe in the pulp tissue that was in contact with formocresol, and some became partially or totally necrotic [34]. Histological analysis of the formocresol pulpotomized teeth showed zones of atrophy, inflammation and fibrosis [35]. In biodentine pulpotomy, a dentine bridge formed under the materials induced by the calcium silicate-based cement, with odontoblast and odontoblast-like cells can be found in the adjacent area [11,36,37]. There was no evidence of inflammation or necrotic areas below the dentine bridge, and there was no statistically significant difference between the biodentine and MTA. The formation of the dentine bridge was interpreted as a positive reaction, a sign of healing to protect the underlying pulp tissue [38].
The clinical advantages of the using biodentine are high biocompatibility, high compressive strength, its sealing ability, ease of handling, faster setting [9] and less step required for the pulpotomy procedure, because biodentine can be placed in contact with the pulp and used as temporary coronal restoration for up to 6 months. The setting time was 9 to 12 minutes after mixing. Formocresol required 5 minutes to fix the pulp tissue before temporary filled with reinforced zinc-oxide eugenol. It can be concluded that formocresol pulpotomy had more steps to do than using biodentine but the duration of the procedure may be approximately the same. From this study, there was no statistical difference between the 2 groups in the clinical (p=1.00) but there was statistically significant difference in radiographic success rates (p=0.022) at 12 months follow-up. Biodentine showed statistically significant difference, higher pulp canal obliteration when compared with formocresol pulpotomies (p=0.016). Most radiographic failure of the formocresol pulpotomy was pathologic root resorption with periapical radiolucency, which was not found when using biodentine. This study found that biodentine is an alternative and effective material for pulpotomy treatment in deep carious primary molars. Although biodentine is cheaper than MTA, a limiting factor with biodentine usage is still the high cost of the material.
Limitation
Further studies are required to evaluate the long-term success rates of the biodentine pulpotomy, as there were limitations with this study because of the short-term follow-up and the small sample size. Long-term clinical and radiographic studies are required with a larger sample size to test the efficacy of biodentine as a pulpotomy medicament.
Conclusion
Biodentine showed similar clinical and radiographic success rates as formocresol at 6 months follow-up and it was effective in clinical and radiographic with favorable outcome at 12 months follow-up. Biodentine can be used as an alternative medicament for pulpotomy treatment in deep carious primary molars.
At 6 months, 47 teeth were available to follow-up (formocresol=23, biodentine=24); At 12 months, an additional 2 teeth from biodentine group were lost due to patient relocation