Diathermy Versus Conventional Scalpel in Making an Abdominal Incision: A Prospective Study
Shruti Pandey1, Rajendra Prasad Choubey2, Indra Tiwari Narain3
1 Senior Resident, Department of Surgery, Hindu Rao Hospital, Delhi, India.
2 Director, Department of Surgery, ANIIMS, Port Blair, Andaman and Nicobar Islands, India.
3 Senior Consultant Surgery and Plastic, Department of Surgery, Kalra Hospital and Research Institute, Kirti Nagar, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Rajendra Prasad Choubey, ANIIMS, Port Blair, Andaman and Nicobar Islands, India.
E-mail: shrutipandey_29@yahoo.co.in
Introduction
Scalpel incisions produce nominal harm to neighboring and adjacent tissues. Diathermy is considered to be an efficient mode of incision and its use is widespread, but due to scarring potential, advanced wound contamination rate and poor wound healing, the extensive use of surgical diathermy for incisions.
Aim
To compare the use of electrosurgery and conventional scalpel in making an abdominal incision with respect to blood loss, operating time, wound infection rate and post-operative pain.
Materials and Methods
This was a prospective study in which patients above 16 years of age were included and all patients undergoing abdominal surgery were randomly allocated to two arms of the study. In Group A, incision by conventional scalpel and in group B, incision by diathermy were made. Incisions were of three types i.e., Kocher’s incision were 4, Midline were 22 and Pfannestiel were 44. Data was collected and entered in the Microsoft excel sheet and analysed for blood loss, operating time, wound infection rate and post-operative pain.
Results
Total number of patients included in this study was 70. Age of the participants were in range of second to seventh decade, youngest being 19 years and the oldest being 73 Years of age. Male and female ratio was 1:6. Time taken for incision and blood loss in group B is less than group A respectively. (p=0.009, p=0.001) in all types of incision. Rate of complications following electrocautery incision were also low and no haematoma or seroma were noted in those wounds.
Conclusion
Diathermy technique is compatible with conventional scalpel being safe, effective and simple. Less blood loss was noted with clearer field of dissection, as compared to one created by conventional steel scalpel. Because of the faster haemostasis, the mean time of making an incision was also less in case of diathermy.
Electrosection, Incision, Scalpel incision, Wound infection
Introduction
Conventionally skin incisions have regularly been performed with scalpels. In present days there is a change in trend from this method to electrosurgical skin incisions [1]. Cautery is considered to be an efficient mode of dissection device being haemostatic & convenient. Reduced blood loss, dry and rapid separation of the tissue, and a possible decreased risk of unintentional damage caused by the scalpel to working personnel are the possible advantages of electrosurgery [2,3]. Despite its several advantages, the idea of Diathermy as a cutting instrument instead of a conventional scalpel for making a surgical incision has met with skepticism by majority of the surgeons, because of its unnecessary scarring, elevated wound infection rate and reduced wound healing have condensed the extensive use of surgical diathermy for skin incisions [4,5]. Hence, the present study was conducted with an aim to compare the use of electrosurgery and conventional scalpel in making an abdominal incision with respect to blood loss, operating time, wound infection rate and post-operative pain.
Materials and Methods
The prospective study was conducted in the department of Surgery, Kalra Hospital from May 2011 to June 2012. All the patients undergoing elective abdominal surgery during the above period were included in the study. All patients of both sex above 16 years of age, requiring elective abdominal surgery, who agreed to regular follow-up visit and consented to be part of the study, were included. Patients with history of receiving antibiotics in preceding seven days, patient with previous surgical scar, those who receiving immuno-supportive therapy or undergone radiation therapy were excluded. Patient diagnosed with chronic pain syndrome or undergone treatment for pain management and pregnant women were also excluded. Institutional ethical clearance was obtained prior to conduction of study (NBE/Thesis/2048/2012/14169) and written informed consent was obtained. The candidates were divided into two groups- Group A, in which abdominal incision was made with a scalpel and Group B, in which abdominal incision was made with diathermy (setting of 70 watt with monopolar current was used). The incisions were of three types i.e., Kocher’s incision were 4, Midline were 22 and Pfannestiel were 44. A detailed history and clinical examination followed by investigations leading to confirmation of diagnosis and routine pre-anaesthetic investigations for fitness of the patient was undertaken. All patients received one dose of Inj. Ceftriaxone 1 gm I/V and Inj. Amikacin 500 mg I/V, as pre-operative and three doses as post-operative prophylaxis. The abdominal skin was prepared with povidone iodine. Incision time was calculated from the time of making incision to the time of opening peritoneum with complete homeostasis, with a stop watch and blood loss during incision was calculated using dry surgical mops which were weighed pre-operatively as well as post-operatively in a sterile manner, using weighing scale with 2 gram resolution. Pain assessment was done with Visual Analogue Score (VAS). Pain was represented on a 10 cm straight line, extremes of which corresponded to no pain at one end and the worst pain imaginable on the other end. All patients received eight hourly intramuscular diclofenac sodium injections for pain relief. VAS score was measured at 8, 14 and 24 hours respectively. All the patients were followed up in 2nd and 4th week after discharge to record any wound infections.
Statistical Analysis
Data was entered into Microsoft excel data sheet and analysed using SPSS 22 version software. Categorical data was represented in the form of frequencies and proportions. Unpaired t-test was used as test of significance for qualitative data.
Results
Patient included in the study were in second to seventh decade of life, youngest being 19 years and the oldest 73 years of age. Male to female ratio was 1:6. There was predominance of females as pfannestial incision is mainly used for hysterectomy and lower abdomen and pelvis approaches. Outcome parameters with respect to different types of incisions are shown in [Table/Fig-1,2 and 3]. There was statistically significant increase in the mean time taken for incision in Group A when compared with Group B in case of pfannestiel incision (310.18±72.63 and 231.5±112.45 respectively; p=0.009 [Table/Fig-3].
Outcome parameters comparison between two groups in respect to Kochers incision.
| Technique | N | Mean | Std. deviation | Median | Minimum | Maximum | T-value | p-value* |
|---|
| Time taken in seconds | Scalpel | 2 | 273 | 72.12 | 273 | 222 | 324 | 0.753 | 0.530 |
| Electrocautery | 2 | 199 | 118.79 | 199 | 115 | 283 |
| Blood loss in gm | Scalpel | 2 | 31.5 | 4.95 | 31.5 | 28 | 35 | 1.317 | 0.318 |
| Electrocautery | 2 | 20 | 11.31 | 20 | 12 | 28 |
| Length (cm) | Scalpel | 2 | 11.7 | 1.84 | 11.7 | 10.4 | 13 | 0.405 | 0.724 |
| Electrocautery | 2 | 10.8 | 2.55 | 10.8 | 9 | 12.6 |
| Thickness (cm) | Scalpel | 2 | 3.8 | 0.28 | 3.8 | 3.6 | 4 | 1.807 | 0.216 |
| Electrocautery | 2 | 4.2 | 0.14 | 4.2 | 4.1 | 4.3 |
| VAS At 8 Hrs | Scalpel | 2 | 7.5 | 0.71 | 7.5 | 7 | 8 | 2.24 | 0.155 |
| Electrocautery | 2 | 5 | 1.41 | 5 | 4 | 6 |
| At 14 Hrs | Scalpel | 2 | 5.5 | 0.71 | 5.5 | 5 | 6 | 2.817 | 0.106 |
| Electrocautery | 2 | 3.5 | 0.71 | 3.5 | 3 | 4 |
| At 24 Hrs | Scalpel | 2 | 3 | 0 | 3 | 3 | 3 | NA | NA |
| Electrocautery | 2 | 2 | 0 | 2 | 2 | 2 |
*unpaired t-test
Outcome parameters comparison between two groups in respect to Midline incision.
| Technique | N | Mean | Std. deviation | Median | Minimum | Maximum | T-value | p-value* |
|---|
| Time taken in seconds | Scalpel | 11 | 222.82 | 93.5 | 201 | 120 | 440 | 0.935 | 0.361 |
| Electrocautery | 11 | 186.91 | 86.43 | 160 | 74 | 300 |
| Blood loss in gm | Scalpel | 11 | 24.18 | 13.46 | 22 | 8 | 58 | 3.403 | 0.003 |
| Electrocautery | 11 | 8.91 | 6.35 | 10 | 2 | 20 |
| Length (cm) | Scalpel | 11 | 14.29 | 2.61 | 14.8 | 9.6 | 18 | 0.873 | 0.393 |
| Electrocautery | 11 | 15.61 | 4.28 | 15 | 8 | 22 |
| Thickness (cm) | Scalpel | 11 | 2.75 | 0.72 | 2.8 | 1.5 | 3.8 | 0.150 | 0.893 |
| Electrocautery | 11 | 2.8 | 0.84 | 2.7 | 1.8 | 4.3 |
| VAS At 8 Hrs | Scalpel | 11 | 6.45 | 1.69 | 7 | 3 | 8 | 1.950 | 0.065 |
| Electrocautery | 11 | 5.09 | 1.58 | 4 | 3 | 8 |
| At 14 Hrs | Scalpel | 11 | 3.91 | 1.51 | 3 | 2 | 7 | 2.685 | 0.014 |
| Electrocautery | 11 | 2.27 | 1.35 | 2 | 1 | 4 |
| At 24 Hrs | Scalpel | 11 | 1.91 | 1.14 | 2 | 0 | 4 | 2.982 | 0.007 |
| Electrocautery | 11 | 0.73 | 0.65 | 1 | 0 | 2 |
*unpaired t-test
Outcome parameters comparison between two groups with respect to Pfannestiel incision.
| Technique | N | Mean | Std. deviation | Median | Minimum | Maximum | T-value | p-value* |
|---|
| Time Taken in seconds | Scalpel | 22 | 310.18 | 72.63 | 317 | 180 | 434 | 2.757 | 0.009 |
| Electrocautery | 22 | 231.5 | 112.45 | 222.5 | 74 | 444 |
| Blood Loss in gm | Scalpel | 22 | 31.91 | 9.06 | 33 | 12 | 48 | 5.225 | <0.001 |
| Electrocautery | 22 | 14.91 | 12.28 | 10 | 2 | 40 |
| Length (cm) | Scalpel | 22 | 12.45 | 1.35 | 12.3 | 9.8 | 15 | 0.000 | 0.985 |
| Electrocautery | 22 | 12.45 | 1.86 | 12.2 | 9.8 | 16.4 |
| Thickness (cm) | Scalpel | 22 | 3.98 | 0.61 | 4.1 | 2.9 | 5 | 0.477 | 0.631 |
| Electrocautery | 22 | 3.89 | 0.64 | 3.8 | 2.9 | 5.3 |
| VAS At 8 Hrs | Scalpel | 22 | 6.95 | 1.17 | 7 | 4 | 8 | 4.729 | <0.001 |
| Electrocautery | 22 | 5 | 1.54 | 5 | 3 | 8 |
| At 14 Hrs | Scalpel | 22 | 4.59 | 1.01 | 4.5 | 3 | 6 | 3.820 | <0.001 |
| Electrocautery | 22 | 3.09 | 1.54 | 2 | 2 | 6 |
| At 24 Hrs | Scalpel | 22 | 2.64 | 1.14 | 2.5 | 0 | 5 | 3.039 | 0.004 |
| Electrocautery | 22 | 1.5 | 1.34 | 1 | 0 | 4 |
*unpaired t-test
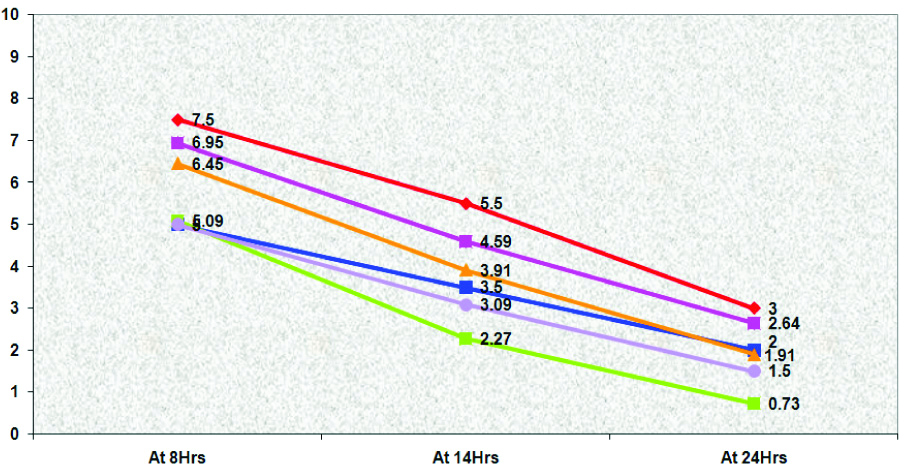
Similarly, mean blood loss was statistically higher in Group A when compared with Group B (31.91±9.06 and 14.91±12.28 gm respectively; p<0.001) [Table/Fig-3]. Only one patient each, developed wound infection in the scalpel and the electrocautery groups. Change in VAS score with respect to different type of incision at different interval of time is shown in [Table/Fig-4].
Change in VAS w.r.t time in different incisions and techniques
Discussion
Initial studies with diathermy suggested that, electrosurgical incisions showed excessive scarring and poor wound healing. With the use of sinusoidal current, better control of energy dispensed was developed. In the present study, mean incision time and amount of blood loss was significantly reduced in electrocautery group in comparison to the scalpel group. These findings are in concordance with the study conducted by Nandurkar VS et al., in which statistically significant increase was noted in the mean time taken for incision in scalpel group when compared with electrocautery group (36.8±8.8 and 27.0±10.1 respectively; p<0.001) [1]. Our findings also corroborated with Chau JK et al., (210.33±68.82 in electrocautery group and 239±82.99 in scalpel group) and by Dixon AR and Watkin DF, (90±22 in electrocautery group and 126±25 in scalpel group) [6,7]. Similarly mean blood loss was statistically higher in Group A when compared with Group B (3.4±1.5 mL and 2.6±1.5 mL respectively; p=0.021) [1]. These findings are also similar to Talpur AA and Khaskheli AB, who in their study reported statistically significant reduction in mean incision time and mean blood loss with electrocautery when compared with scalpel [8].
Similarly, Ly J et al., in their systemic review and meta-analysis of fourteen randomised trials comprising of 2541 patients (1267 undergoing abdominal wall incision by cutting diathermy and 1274 by scalpel), noticed significantly reduced amounts of blood loss (mean difference of 0.72 mL/cm2 (p<0.001) and shorter incision time (mean difference of 36 seconds; p<0.001) with diathermy incisions as compared to scalpel incisions [9]. The average pain score in present study was found to be lower in electrocautery group in all the incisions; however it was statistically significant in pfannestiel incision. These findings are similar to the findings by Nandurkar VS et al., which concluded that post-operative pain is significantly less (p-value 0.021) in the electrocautery group on day 1 [1]. Our findings are also similar to other published studies by Ayandipo OO and Afuwape OO, and Kearns SR et al., Aird LN and Brown CJ, also noted that electrocautery significantly reduced post-operative wound pain [2,10,11]. Other studies whose results are in agreement with the present study were by Siraj A et al., Gilmore M et al., and Shivagouda P et al., which showed that elective laparotomy incisions made with electrocautery had major benefits in terms of reduced early post-operative pain [12-14]. Only one patient in each group, developed wound infection in the scalpel and the electrocautery groups which was not statistically significant. These findings are similar to studies conducted by Nandurkar VS et al., and Talpur AA et al., [1,8].
Limitation
Small sample size is major limitation of the study.
Conclusion
Electrosection proves to be safe and efficient than conventional scalpel method in terms of patient comfort, by causing less post-operative pain. Electrosection is the ideal method of incision in high risk patients, where both the blood loss and operating time are at premium.
*unpaired t-test
*unpaired t-test
*unpaired t-test
Author Declaration:
Financial or Other Competing Interests: No
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 01, 2019
Manual Googling: Sep 09, 2019
iThenticate Software: Sep 18, 2019 (13%)
[1]. Nandurkar VS, Mohan Kumar K, Prakash M, Suma S, Diathermy versus scalpel incisions in elective abdominal surgery: a comparative studyInt Surg J 2018 5(9):3124-28.10.18203/2349-2902.isj20183734 [Google Scholar] [CrossRef]
[2]. Kearns SR, Connolly EM, McNally S, McNamara DA, Deasy J, Randomised clinical trial of diathermy versus scalpel incision in elective midline laparotomyBritish Journal of Surgery 2001 88:41-44.10.1046/j.1365-2168.2001.01625.x11136307 [Google Scholar] [CrossRef] [PubMed]
[3]. Soderstrom R, Brill AI, Principles of Electrosurgery as Applied to GynecologyIn Te Linde’s Operative Gynecology 2008 tenth editionPhiladelphia, PALippincott-Raven Publishers:280-297.(e/c book) [Google Scholar]
[4]. Kim H, Brunner E, Ritter E, Relevance of methods of skin incision technique on development of wound infectionAm Surg 1990 56:129-30. [Google Scholar]
[5]. Rappaport WD, Hunter GC, Allen R, Lick S, Halldorsson A, Chvapil T, Effect of electrocautery on wound healing in midline laparotomy incisionsAm J Surg 1990 160:618-20.10.1016/S0002-9610(05)80757-3 [Google Scholar] [CrossRef]
[6]. Chau JK, Dsigielewski P, Mlynarek A, Cote DW, Allen H, Harris JR, Steel scalpel versus electrocautery blade: Comparison of cosmetic and patient satisfaction outcomes of different incision methodsJ Otolaryngol Head Neck Surg 2009 38:427-33. [Google Scholar]
[7]. Dixon AR, Watkin DF, Electrosurgical skin incision versus conventional scalpel: A prospective trialJ R Coll Surg Edinb 1990 35:299-301. [Google Scholar]
[8]. Talpur AA, Khaskheli AB, Randomised, clinical trial on diathermy and scalpel incisions in elective general surgeryIran Red Crescent Med J 2015 17:e1407810.5812/ircmj.1407825834739 [Google Scholar] [CrossRef] [PubMed]
[9]. Ly J, Mittal A, Windsor J, Systematic review and meta-analysis of cutting diathermy versus scalpel for skin incisionBr J Surg 2012 99:613-20.10.1002/bjs.870822367850 [Google Scholar] [CrossRef] [PubMed]
[10]. Ayandipo OO, Afuwape OO, Diathermy versus scalpel incision in a heterogeneous cohort of general surgery patients in a Nigerian teaching hospitalNiger J Surg 2015 21:43-47.10.4103/1117-6806.15319325838766 [Google Scholar] [CrossRef] [PubMed]
[11]. Aird LN, Brown CJ, Systematic review and meta-analysis of electrocautery versus scalpel for surgical skin incisionsAm J Surg 2012 204:216-21.10.1016/j.amjsurg.2011.09.03222537473 [Google Scholar] [CrossRef] [PubMed]
[12]. Siraj A, Gilani AAS, Dar MF, Rasiq S, Elective midline laparotomy: Comparison of diathermy and scalpel incisionsProfessional Med J 2011 18:106-11. [Google Scholar]
[13]. Kearns , Gilmore M, McCabe JP, Kaar K, Curtin W, Diathermy versus scalpel incisions for hemiarthroplasty: A randomised prospective trialBone Joint Surg Br 2004 86:129Available at: https://online.boneandjoint.org.uk/doi/abs/10.1302/0301-620X.86BSUPP_II.0860129c [Google Scholar]
[14]. Shivagouda P, Gogeri BV, Godhi AS, Metgud SC, Comparing the efficacy of diathermy incision versus scalpel incision over skin in patients undergoing inguinal hernia repair: Prospective randomised control trialRecent Research Sci Tech 2010 2:44-47. [Google Scholar]