Tumours of Salivary gland compromise about 3% to 5.4% of head and neck malignant neoplasms. According to WHO, they are 24 different types [1]. Malignant salivary gland tumours represent the 2nd most common malignancy of the oral cavity after squamous cell carcinoma [2]. MEC representing the commonest one [3].
Many studies have tried to understand the behaviour of MEC both histologically and clinically, due to complexity and heterogeneity of these neoplasms [4].
The ACC is uncommon tumour but detected frequently in the salivary gland. There is no consistent histological parameter that can be used as specific marker for metastasis and recurrence. Though, the most dependable factors for predicting tumour behaviour is histological classification into cribriform, tubular, and solid subtypes with the last subtype considered the highly aggressive one [5].
Both salivary and mammary glands which are tubulo-acinar exocrine glands having the same morphological characteristics and their tumours sharing similar histological features. Although their neoplasms showing variable incidence and clinical presentation, similar biological characteristics were recognised in these 2 tumours, thus promising common targeted therapy could be considered [6-8].
The surrounding stroma of the solid cancers composed mainly of fibroblasts, smooth muscle cells, endothelial cells and immune cells. So, there is a well-recognised relationship between malignancy and inflammation [9]. The major inflammatory component in tumour microenvironment is TAMs [10]. There is a great conflict about the definitive role of TAMs in tumour development. Their main function was supposed to exert direct cytotoxic effects on tumour cells, engulf the cellular debris of apoptotic or necrotic cell, and present antigens of the neoplasms to T cells [11]. Many researches also recommend that TAMs can encourage cancer growth and metastasis [12,13].
Numerous macrophage-related markers such as CD68, CD14, and CD23 are expressed by TAMs. CD68 is a protein extremely expressed by the cells of the monocyte family (e.g., monocytes, phagocytes, osteoclasts), by tissue macrophages (e.g., Kupffer cells, microglia) and by circulating macrophages [14].
Ki-67 is a nuclear proliferative marker that is used to determine the outcome of neoplasms and predict the rate of recurrence following radiation [15].
Frequent researches concluded that many tumours rather than breast cancers showing steroid hormone receptor expression [16-18]. These steroid hormone receptors were thought to play a key role in development, progression and therapy of these neoplasms [19]. To establish the role of Oestrogen Receptor (ER) and Progesterone Receptor (PR) expression in the development and targeted therapy of salivary gland tumours, they have been extensively investigated, but considerable controversy was noticed [20,21].
HER-2 is an oncogene that belong to the family of epidermal growth factor receptor. Many researches documented that overexpression of HER-2 play a crucial role in the pathogenesis and expansion of aggressive breast cancers [22].
Study the expression of sex hormone receptors and HER-2 in tumours of salivary glands has been increasing due to the possibilities for using hormone antagonists and targeted HER-2 therapy especially in aggressive salivary duct carcinomas [23, 24].
The aim of the present work was to assess the immunohistochemical expression of TAMs related marker CD68 and proliferative marker Ki-67 in a group of Egyptian patients with malignant salivary tumours (MEC and ACC). Furthermore, to study their correlation with clinicopathological factors, ERα, and HER-2 and detect the usefulness of these markers in the prognosis of such tumours.
Materials and Methods
Patients and Clinical Data
Type of study: Cross sectional study,
Place of study: Departments of Pathology and Surgery, Zagazig and Banha Universities, Egypt.
Sample size: The study included 37 salivary carcinomas (25 cases of MEC and 12 cases of ACC). The control group consisted of 10 normal salivary tissues that were obtained from patients who underwent sialoadenectomy for treatment of intraglandular sialolithiasis.
Sample collection method: The studied cases were selected randomly from the archives of pathology departments from January 2015 to May 2018. Tumours were staged according to the American Joint Committee on Cancer (AJCC) TNM system [25]. Grading of MEC have followed AFIP grading system [26] and of ACC was done according to Spiro RH and Huvos AG, [27]. Clinical and pathological information were collected from patient’s medical records.
All the patients did not receive chemotherapy or radiation prior to surgery. The Institutional Research Board of Zagazig University (ZU-IRB) approved this research. All paraffin blocks were dissected at 4-5 microns and stained with H&E to confirm the diagnosis and grade the tumours.
Immunohistochemical Staining
The sections cut from the blocks were deparaffinized, rehydrated, and placed in hydrogen peroxide to block the activity of endogenous peroxidase. Antigen retrieval was achieved by keeping in 0.01 M citrate buffer for 5 minutes in a pressure cooker. The primary antibodies were added to the sections at room temperature for 60 minutes. The norm streptavidin-biotin-peroxidase complex system was performed for CD68 (Mouse Monoclonal Antibody, clone KP1, Dilution 1:200, catalogue no. MA5-13324, Thermo Fisher Scientific/Lab. Vision Corporation, Rockford, USA.), Ki 67 (Rabbit Polyclonal antibody, Dilution 1:20, catalogue no. PA5-16785, Thermo Fisher Scientific/Lab. Vision Corporation, Rockford, USA.), ERα (Rabbit Polyclonal antibody, Dilution 1 μg/mL, catalogue no. PA1-311, Thermo Fisher Scientific/Lab. Vision Corporation, Rockford, USA.) And HER-2 (Rabbit Polyclonal antibody, Dilution 1:10, catalogue no. PA5-14635, Thermo Fisher Scientific/Lab. Vision Corporation, Rockford, USA) by applying DAB as the chromogen. Human tonsil (germinal centre macrophages) were used as a positive control for CD68, while breast carcinoma was used as a positive control for Ki-67, ERα, and HER-2. Negative controls for all markers were performed by omitting the primary antibody.
Evaluation of Immunohistochemical Staining
CD68 expression was regarded positive if there was any brown membranous staining. Intratumoral TAMs counts was determined semi-quantitatively as described previously, with some modification [28]. Firstly, the stained sections were screened using low power to recognise the regions of highest macrophage density. TAMs were scored as low (1-20%) and high (>20%) groups, indicating proportion of positive cells in the intratumoral and stromal area [28].
Ki-67 expression was regarded positive only if nuclear staining was present. The Ki-67 Proliferative Index (PI) was judged by counting at least 500 tumour cells in 5 high power fields. The Ki-67 PI was scored as high (>25%) and low (<25%) groups, indicating proportion of positive cells [29].
HER-2 membranous immunoreactivity were scored into four groups {negative (0), weak positive (1+), intermediate (2+), and strongly positive (3+)} [30]. Finally, for statistical analysis we have 2 groups, negative (0,1) and positive (2,3).
ER nuclear immunoreactivity was scored using semi-quantitative method as previously described [31]. This system considers both the intensity (the intensity score ranges from 0 to 3) and the proportion (proportion score ranges from 0 to 5) of stained cells. Both scores were added to get a total score from 0 to 8. Finally, for statistical analysis we have 2 groups, negative (0-2) and positive (3-8).
Statistical Analysis
The results from the continuous variables analysis were expressed as a Means±Standard Deviation (SD). Categorical data analysis was performed using the χ2 or Fisher’s exact test, Spearman correlation test was done for correlation analysis. The statistical analyses were done using SPSS software (version 19.0; SPSS, Chicago, IL) and p≤0.05 was regarded as indicator of a statistically significant difference.
Results
Clinicopathological Results
The mean age of the studied 37 salivary carcinomas patients at initial surgery was 50.16±12.01 years (range 23-72 years). 67.6% of cases were MEC and 32.4% were ACC. All carcinoma patients’ clinic-pathological data are outlined in [Table/Fig-1].
Clinicopathological characteristics of the studied 37 malignant salivary tumours (MEC and ACC).
| Variables | MEC n (%) | ACC n (%) |
|---|
| Age at surgery (Years) |
| <50 | 9 (36.0%) | 4 (33.3%) |
| ≥50 | 16 (64.0%) | 8 (66.7%) |
| Gender |
| Male | 14 (56.0%) | 9 (75.0%) |
| Female | 11 (44.0%) | 3 (25.0%) |
| Location |
| Major salivary gland | 19 (76.0%) | 10 (83.3%) |
| Minor salivary gland | 6 (24.0%) | 2 (16.6%) |
| Grade |
| Low/Intermediate | 16 (64.0%) | 7 (58.3%) |
| High | 9 (36.0%) | 5 (41.7%) |
| Tumour size (cm) |
| ≤3 | 14 (56.0%) | 9 (75.0%) |
| >3 | 11 (44.0%) | 3 (25.0%) |
| Lymh node involvement |
| No | 18 (72.0%) | 10 (83.3%) |
| Yes | 7 (28.0%) | 2 (16.6%) |
| Perineural invasion |
| No | 18 (72.0%) | 10 (83.3%) |
| Yes | 7 (28.0%) | 2 (16.6%) |
| Staging |
| I/II | 14 (56.0%) | 6 (50.0%) |
| III/IV | 11 (44.0%) | 6 (50.0%) |
| Total | 25 (100%) | 12 (100%) |
Results of Immunohistochemical Expression of CD68 (TAMs), Ki-67, ER-α, and HER-2
Immunohistochemical expression of CD68 (TAMs count): CD68 immunoreactivity was overexpressed (high TAMs) in 64.0% of the studied MEC compared to 41.7% overexpression in ACC. The difference in CD68 expression between MEC and ACC was not statistically significant (p=0.199) [Table/Fig-2]. All the studied normal salivary tissues (10 controls) were negatively express CD68. Analysis of CD68 immunoexpression (TAMs) with the clinicopathological criteria of the studied 37 carcinomas revealed that CD68 is more significantly expressed (high TAMs) in high grades carcinomas (p=0.006 and 0.045 for MEC and ACC respectively). High TAMs were also more significantly detected in MEC and ACC with advanced FIGO stage (p=0.033 and 0.015 for MEC and ACC respectively). In MEC, high TAMs was detected significantly with larger tumours size (p=0.017), but not in ACC (p=0.636). No correlation was found between high TAMs and other clinicopathological factors (p>0.05) [Table/Fig-3,4a-c].
Results of immunohistochemical expression of CD68 (TAMs), Ki-67, HER-2 and ER-α among the studied 37 malignant salivary tumours.
| Variables | Expression | MEC n=(25) | ACC n=(12) |
|---|
| TAMs | Low | 9 (36.0%) | 7 (58.3%) |
| (CD68) | High | 16 (64.0%) | 5 (41.7%) |
| p-value | 0.199 |
| Ki-67 PI | Low | 8 (32.0%) | 8 (66.7%) |
| High | 17 (68.0%) | 4 (33.3%) |
| p-value | 0.046 |
| ERα | (+) | 4 (16.0%) | 3 (25.0%) |
| (-) | 21 (84.0%) | 9 (75.0%) |
| p-value | 0.406 |
| HER-2 | (+) | 3 (12.0%) | 2 (16.7%) |
| (-) | 22 (88.0%) | 10 (83.3%) |
| p-value | 0.529 |
Association CD68 (TAMs) and Ki67 expressions with clinicopathological parameters, ER α, and HER-2 in the studied 37 malignant salivary tumours (MEC, ACC).
| Variable | MEC | ACC |
|---|
| TAMs | Ki-67 PI | TAMs | Ki-67 PI |
|---|
| Low n (%) | High n (%) | Low n (%) | High n (%) | Low n (%) | High n (%) | Low n (%) | High n (%) |
|---|
| Age at surgery (Years) |
| <50 | 5 (20.0) | 4 (16.0) | 4 (16.0) | 5 (20.0) | 3 (25.0) | 1 (8.33) | 2 (16.7) | 2 (16.7) |
| ≥50 | 4 (16.0) | 12(48.0) | 4 (16.0) | 12(48.0) | 4 (33.33) | 4 (33.33) | 6 (50.0) | 2 (16.7) |
| p-value | 0.137 | 0.287 | 0.424 | 0.406 |
| Gender |
| Male | 4 (16.0) | 10 (40.0) | 4 (16.0) | 10 (40.0) | 5 (41.7) | 4 (33.33) | 5 (41.7) | 4 (33.33) |
| Female | 5 (20.0) | 6 (24.0) | 4 (16.0) | 7 (28.0) | 2 (16.7) | 1 (8.33) | 3 (25.0) | 0 (0.0) |
| p-value | 0.324 | 0.504 | 0.636 | 0.254 |
| Location |
| Major salivary gland | 7 (28.0) | 12 (48.0) | 6 (24.0) | 13 (52.0) | 6 (50.0) | 4 (33.33) | 7 (58.3) | 3 (25.0) |
| Minor salivary gland | 2 (8.0) | 4 (16.0) | 2 (8.0) | 4 (16.0) | 1 (8.33) | 1 (8.33) | 1 (8.33) | 1 (8.33) |
| p-value | 0.637 | 0.650 | 0.681 | 0.575 |
| Grade |
| Low/Intermediate | 9 (36.0) | 7 (28.0) | 8 (32.0) | 8 (32.0) | 6 (50.0) | 1 (8.33) | 7 (58.3) | 0 (0.0) |
| High | 0 (0.0) | 9 (36.0) | 0 (0.0) | 9 (36.0) | 1 (8.33) | 4 (33.33) | 1 (8.33) | 4 (33.33) |
| p-value | 0. 0.006 | 0.011 | 0.045 | 0.010 |
| Tumour size (cm) |
| ≤3 | 8 (32.0) | 6 (24.0) | 5 (20.0) | 9 (36.0) | 5 (41.7) | 4 (33.33) | 5 (41.7) | 4 (33.33) |
| >3 | 1 (4.0) | 10 (40.0) | 3 (12.0) | 8 (32.0) | 2 (16.7) | 1 (8.33) | 3 (25.0) | 0 (0.0) |
| p-value | 0.017 | 0.495 | 0.636 | 0.254 |
| Lymh node involvement |
| No | 7 (28.0) | 11 (44.0) | 5 (20.0) | 13 (52.0) | 6 (50.0) | 4 (33.33) | 7 (58.3) | 3 (25.0) |
| Yes | 2 (8.0) | 5 (20.0) | 3 (12.0) | 4 (16.0) | 1 (8.33) | 1 (8.33) | 1 (8.33) | 1 (8.33) |
| p-value | 0.500 | 0.393 | 0.681 | 0.575 |
| Perineural invasion |
| No | 6 (24.0) | 12 (48.0) | 4 (16.0) | 14 (56.0) | 5 (41.7) | 5 (41.7) | 6 (50.0) | 4 (33.33) |
| Yes | 3 (12.0) | 4 (16.0) | 4 (16.0) | 3 (12.0) | 2 (16.7) | 0 (0.0) | 2 (16.7) | 0 (0.0) |
| p-value | 0.499 | 0.115 | 0.318 | 0.424 |
| Staging |
| I/II | 8 (32.0) | 6 (24.0) | 5 (20.0) | 9 (36.0) | 6 (50.0) | 0 (0.0) | 3 (25.0) | 3 (25.0) |
| III/IV | 1 (4.0) | 10 (40.0) | 3 (12.0) | 8 (32.0) | 1 (8.33) | 5 (41.7) | 5 (41.7) | 1 (8.33) |
| p-value | 0.033 | 0.495 | 0.015 | 0.272 |
| ER-α expression |
| (+) | 2 (8.0) | 1 (4.0) | 1 (4.0) | 2 (8.0) | 2 (16.7) | 0 (0.0) | 2 (16.7) | 1 (8.33) |
| (-) | 7 (28.0) | 15 (60.0) | 7 (28.0) | 15 (60.0) | 5 (41.7) | 5 (41.7) | 6 (50.0) | 3 (25.0) |
| p-value | 0.116 | 0.381 | 0.159 | 0.763 |
| HER-2 expression |
| (+) | 2 (8.0) | 1 (4.0) | 1 (4.0) | 2 (8.0) | 2 (16.7) | 0 (0.0) | 2 (16.7) | 0 (0.0) |
| (-) | 7 (28.0) | 15 (60.0) | 7 (28.0) | 15 (60.0) | 5 (41.7) | 5 (41.7) | 6 (50.0) | 4 (33.33) |
| p-value | 0.286 | 0.704 | 0.318 | 0.424 |
| Total | 9 (36.0) | 16 (64.0) | 8 (32.0) | 17 (68) | 7 (58.3) | 5 (41.7) | 8 (66.7) | 4 (33.33) |
| 25 (100) | 25 (100) | 12 (100) | 12 (100) |
Representative samples of Immunohistochemical expression of CD68 & Ki-67: a) Normal salivary tissue showing lack of CD68 immunostaining (100x); b) low grade ACC showing postive CD68 immunostaining with low TAMs count; c) High grade MEC showing postive CD68 immunostaining with high TAMs count; d) low grade ACC showing low Ki-67 immunostaining; e) High grade ACC showing strong Ki-67 immunostaining; f) High grade MEC showing strong Ki-67 immunostaining (400x).
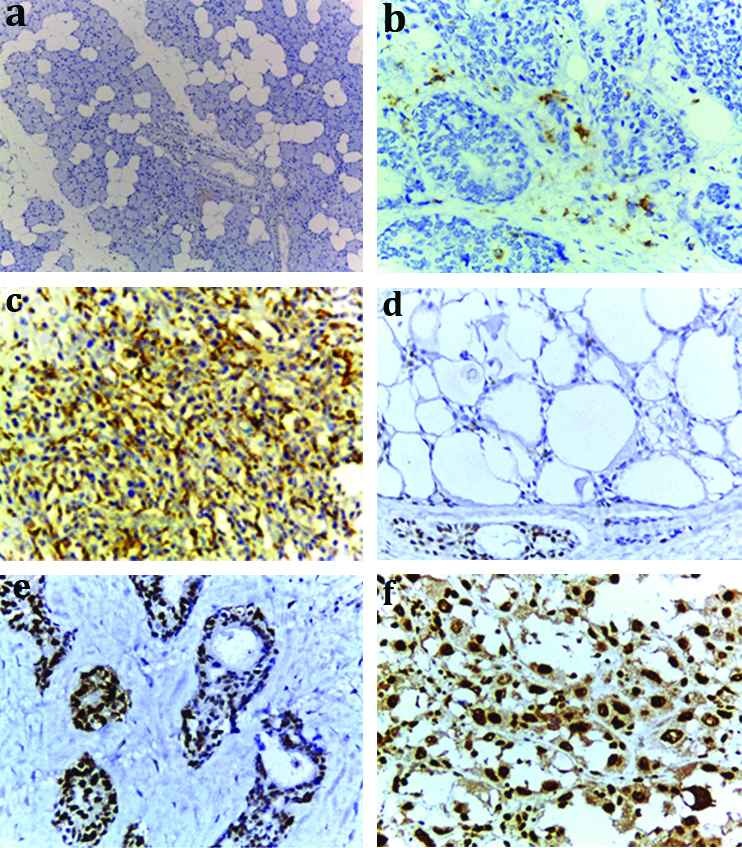
Immunohistochemical expression of Ki-67: Ki-67 immunoreactivity was highly expressed in MEC (68.0%) compared to ACC (33.3%) with statistically significant difference (p=0.046) [Table/Fig-2]. All the controls were negatively express Ki-67. Analysis of Ki-67 immunoexpression with the clinicopathological criteria of the studied 37 carcinomas revealed that Ki-67 was more strongly expressed in high-grade carcinomas with a significant relationship (p=0.011 and 0.01, for MEC and ACC respectively). No significant association could be seen between proliferative activity and HER-2 or ER expression in both MEC and ACC [Table/Fig-3,4d-f].
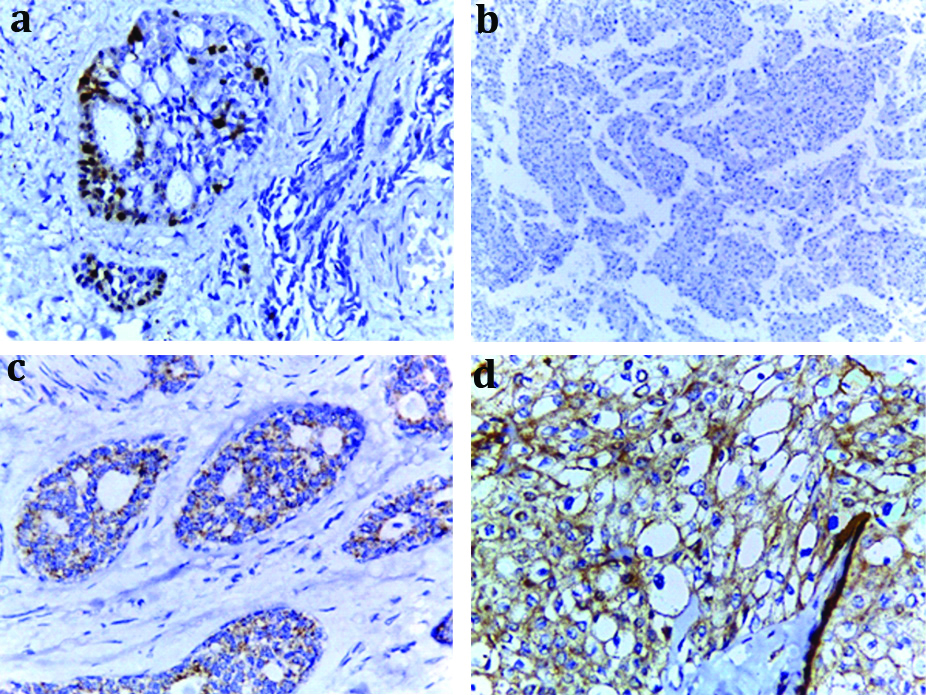
Immunohistochemical expression of ERα, and HER-2: ERα immunoreactivity was detected in 16.0% and 25.0% of the studied MEC and ACC respectively, while HER-2 immunoreactivity was only detected in 12.0% and 16.7% of the studied MEC and ACC. The difference in ERα and HER-2 expression between the two types of salivary carcinomas was not significant (p>0.05). All the controls showed negative expression for both ERα and HER-2. [Table/Fig-2,5].
Representative samples of Immunohistochemical expression of of ER-α and HER-2: a) ACC showing postive nuclear ER-α immunostaining (400x); b) MEC showing lack of ER-α immunostaining (100x); c) ACC showing partial faint membranous HER-2 immunostaining (Score +1) (400x); d) MEC showing complete strong membranous HER-2 immunostaining (Score +3) (400x).
The Correlation Analysis between CD68 and Ki-67 Expressions among the Studied Salivary Carcinomas
A significant moderate positive correlation was detected between the expression of CD68 (TAMs count) and Ki-67 (proliferative activity) among the studied carcinomas (Spearman correlation [r]=0.449, p=0.005), [Table/Fig-6].
Correlation analysis between the expression of CD68 and Ki-67 among the studied 37 malignant salivary tumours (MEC, ACC).
| | Ki-67 PI | |
|---|
| Low expression | High expression | Total |
|---|
| TAMs | Low expression | 11 | 5 | 16 |
| Count (% of total) | (29.7%) | (13.5%) | (43.2%) |
| High expression | 5 | 16 | 21 |
| Count (% of total) | (13.5%) | (43.2%) | (56.8%) |
| Total | 16 | 21 | 37 |
| Count (% of total) | (43.2%) | (56.8%) | (100%) |
*Spearman correlation (r)=0.449; p-value=0.005
Discussion
In the majority of carcinomas including MEC, staging and grading are considered the most valuable prognostic factors for targeted therapy [32]. Nevertheless, new prognostic factors for MEC are required due to high rate of recurrence even with early stage disease. ACC also needs more effective treatment as it show high rate of recurrence and metastasis, even after surgery and radiotherapy [33].
TAMs play an essential role in tumour development and progression by their association with cellular proliferation, angiogenesis and apoptosis [34]. Cellular proliferation measured by Ki-67 is extremely important mechanism in tumorigenesis [35]. The crucial role of sex hormones and epidermal growth factor receptor family in pathogenesis and progression of salivary carcinomas still unclear [34].
In this study, we examined CD68 and Ki-67 expressions in 37 salivary carcinomas and correlated their expression with HER-2, ERα and other clinicopathological factors. Ten normal salivary gland tissues were used as a control.
The present study analysis of CD68 immunoreactivity revealed that high TAMs was detected in 64.0% and 41.7% of the studied MEC and ACC respectively. Shieh YS et al., reported high TAMs in only 48.8% of their studied MEC [34], such difference in TAMs count may be due to different methodology (especially the counting technique) and variations in the type of studied tumours and number of the cases (Shieh YS et al.,: 41 MEC, ours: 25 MEC, 12 ACC). In the present study, correlations of TAMs count with the clinicopathological features of the studied salivary carcinomas revealed significant association of high TAMs with larger tumour size in MEC cases and higher grades and advanced stage in both MEC and ACC. These findings were in concordance with previous related study [34] and support the role of TAMs expressed by CD68 in progression and aggressiveness of salivary carcinomas, and thus TAMs could be regarded as a poor prognostic parameter in MEC and ACC, thus controlling the level of TAMs may have promoting role in targeted therapy.
In the present study, high Ki-67 PI was detected in 68.0% of MEC compared to 33.3% of the studied ACC, with a statistically significant difference between the two tumour type, this is agree with Tadbir AA et al., who reported significant differences in Ki-67 expression between benign salivary gland, pleomorphic adenoma, ACC and MEC with the highest expression was in MEC [36]. However, in contrast to the present finding that reported only negative Ki-67 in normal salivary tissue but not in carcinomas, many previous studies such as Tadbir AA et al., and Alves F et al., reported considerable Ki-67 negativity in the studied carcinomas (Tadbir AA et al.,: 11% and 16% and Alves F et al.,: 53.3% and 40% of the studied MEC and ACC respectively) [36,37]. Fonseca I et al., also reported lower Ki-67 expression in ACC compared to the present [38]. The variations of Ki-67 expression in different researches may be due to difference in the primary antibody used (monoclonal or polyclonal) and different counting methods.
In the present study, Ki-67 was significantly expressed in higher grades MEC and ACC, this is agree with Shieh YS et al., who reported significant correlation of Ki-67 with the grades of studied MEC [34]. This is also in concordance with Elkablawy MA et al., who reported significant association between Ki-67 and poor prognostic variables of the studied breast carcinomas including high tumour grade [29]. The present authors reported no significant association between Ki-67 and other clinicopathological parameters such as tumour size, stage, metastasis, ER or HER-2, agree with previous related study [29]. Expression of Ki-67 was seen in the studied carcinomas and was significantly associated with high grades, supporting the role of this proliferative marker in carcinogenesis and aggressive nature of these neoplasms.
The control cases (normal salivary gland) were negative for both ERα and HER-2, while both markers showed positive expression in few MEC and ACC. ERα was expressed in 16.0% and 25.0% of the studied MEC and ACC respectively, this agree with previous related studies [39-43]. But, Luo SD et al., reported a higher and variable positivity of hormone receptors (vary between 0 and 100%) in their study compared to ours. This wide variability of ER/PR expressions in salivary tumours could be explained by differences in sex, age, histology of the tumours, variability of primary antibodies and using different techniques such as tissue fixation and antigen retrieval [44]. Sex hormone receptors could have important role in management of patients with salivary carcinomas [43], but our results pointed towards a limited application of hormone receptors in therapy due to limited ER positivity in the present studied carcinomas.
The present analysis reported HER-2 positivity in 12.0% and 16.7% of studied MEC and ACC respectively, this is consistent with the result obtained by previous related studies that reported variable HER-2 positivity (vary between 13%-21%) in MEC [43,45], and in ACC (vary between 4%-16%) [33,43,45]. These differences in the level of HER-2 expression may be due to a different techniques and variable mode of quantification of marker positivity. Can NT et al., concluded that amplification of HER-2 in salivary carcinomas may have important implications for targeted therapy [43], but the present data, unfortunately, did not support this conclusion and limits the utility of Herceptin in management of both MEC and ACC due to low level of HER-2 expression in the studied carcinomas.
We reported no significant association between the level of TAMs and the expression of ERα or HER-2. This was in agreement with the study of Lindesten T et al. that reported insignificant association between level of macrophage and HER-2 expression in the studied 17 breast carcinomas, but in contrast to our result, Lindesten T et al., reported a significant negative association of macrophage level with ERα [28]. This difference could be explained by difference in hormone receptor sensitivity and expression between breast and salivary carcinomas.
A significant positive correlation was detected between the expression of CD68 and Ki-67 among the studied salivary carcinomas. This is consistent with the finding obtained by Lindsten T et al., who reported a significant positive correlations between the extent of macrophage infiltration of the tumour measured by CD68 and the proliferation marker Ki-67 among the studied 17 breast carcinomas [28]. This positive correlation between CD68 and Ki-67, supporting the present suggestion that both are poor prognostic parameters and may warn a more aggressive progression in MEC and ACC.
Limitation and Future Recommendations
The present results pointed towards a limited application of ERα and HER-2 in targeted therapy due to limited expressions. A wide scaled research is recommended to study the relationship between ERα, HER-2, level of macrophage and proliferative activity to clarify their role in management of salivary carcinomas.
Conclusion
High level of TAMs expressed by CD68 and high proliferative activity measured by Ki-67 could be regarded as a poor prognostic parameter in MEC and ACC. Moreover, there was a strong correlation between both markers, thus controlling the level of TAMs may have promoting role in targeted therapy for these patient.